Abstract
Background
Nineteen US states and D.C. have used the Affordable Care Act Medicaid health home waiver to create behavioral health home (BHH) programs for Medicaid beneficiaries with serious mental illness (SMI). BHH programs integrate physical healthcare management and coordination into specialty mental health programs. No studies have evaluated the effects of a BHH program created through the Affordable Care Act waiver on cardiovascular care quality among people with SMI.
Objective
To study the effects of Maryland’s Medicaid health home waiver BHH program, implemented October 1, 2013, on quality of cardiovascular care among individuals with SMI.
Design
Retrospective cohort analysis using Maryland Medicaid administrative claims data from July 1, 2010, to September 30, 2016. We used marginal structural modeling with inverse probability of treatment weighting to account for censoring and potential time-dependent confounding.
Participants
Maryland Medicaid beneficiaries with diabetes or cardiovascular disease (CVD) participating in psychiatric rehabilitation programs, the setting in which BHHs were implemented. To qualify for psychiatric rehabilitation programs, individuals must have SMI. The analytic sample included BHH and non-BHH participants, N = 2605 with diabetes and N = 1899 with CVD.
Main Measures
Healthcare Effectiveness Data and Information Set (HEDIS) measures of cardiovascular care quality including annual receipt of diabetic eye and foot exams; HbA1c, diabetic nephropathy, and cholesterol testing; and statin therapy receipt and adherence among individuals with diabetes, as well as HEDIS measures of annual receipt of cholesterol testing and statin therapy and adherence among individuals with CVD.
Key Results
Relative to non-enrollment, enrollment in Maryland’s BHH program was associated with increased likelihood of eye exam receipt among individuals with SMI and co-morbid diabetes, but no changes in other care quality measures.
Conclusions
Additional financing, infrastructure, and implementation supports may be needed to realize the full potential of Maryland’s BHH to improve cardiovascular care for people with SMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
People with serious mental illnesses (SMIs) such as schizophrenia and bipolar disorder die 10–20 years earlier than the overall US population, primarily due to cardiovascular disease (CVD).1,2,3,4,5 Prevalence of every cardiovascular risk factor and behavior is elevated among people with SMI.6,7,8,9,10,11,12 High cardiovascular risk in this group is driven by multiple factors. Antipsychotic medications cause weight gain and alter glucose metabolism.13,14 High rates of poverty, unemployment, housing instability, and criminal justice system involvement in the US population with SMI impede adoption of healthy behaviors and access to services.15,16,17,18,19,20,21,22 Further, the US specialty mental health sector’s historic separation from the general medical sector presents challenges for coordinating mental and physical healthcare.23,24,25 Studies have shown lower rates of receipt of guideline-recommended post-myocardial infarction and diabetes care among populations with versus without SMI,26,27,28,29,30 with particularly low rates of guideline-concordant care among those covered by Medicaid,31 the insurer for nearly 70% of US adults with SMI.32
The 2010 Patient Protection and Affordable Care Act (ACA) Medicaid health home waiver allowed states to create health homes for high-cost, high-need subsets of Medicaid beneficiaries.33,34 Through the waiver program, states can bill Medicaid for care management and coordination which are not traditionally reimbursable services.34 As of June 2019, 19 US states and D.C. have used the ACA Medicaid health home waiver to create a “behavioral health home” (BHH) program for Medicaid beneficiaries with SMI.34 BHHs integrate general medical care management and coordination into the specialty mental health settings where many people with SMI receive the majority of their healthcare services.25,35 BHH implementation is typically led by a nurse care manager embedded in the community mental health setting.36,37,38
No prior studies have examined the effects a BHH program created through the ACA Medicaid health home waiver on quality of cardiovascular care for people with SMI. While a BHH intervention tested in a clinical trial improved cardiovascular care,37 it is important to rigorously evaluate real-world programs given the well-documented “voltage drop” phenomenon, in which the beneficial effects of interventions observed in clinical trials are muted when implemented in real-world settings in the absence of research funding and infrastructure.39 In this study, we evaluate the effects of Maryland’s ACA waiver BHH program on receipt of guideline-concordant cardiovascular care among Medicaid beneficiaries with SMI and co-morbid diabetes or CVD.
METHODS
Behavioral Health Homes
Maryland implemented its BHH program on October 1, 2013.40 BHHs were implemented by psychiatric rehabilitation programs, community-based programs affiliated with outpatient mental health clinics that deliver psychosocial rehabilitation services such as vocational training and mental health case management.41 To qualify for a psychiatric rehabilitation program, Medicaid beneficiaries must have SMI, defined as significant functional impairment resulting from a mental disorder.41
Sixty-three of 255 total psychiatric rehabilitation programs in Maryland had operational BHHs during the study period.42 At each site, the BHH was led by a nurse care manager responsible for leading general medical care management and coordination activities, with support from a medical director and consulting primary care physician or nurse practitioner.40,43 The nurse care manager led BHH enrollment, with psychiatric rehabilitation program participants actively consenting to join the program.40,43 Maryland’s BHH model has been described in detail previously.36
Study Design
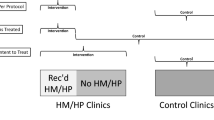
We conducted a retrospective cohort study comparing quality of cardiovascular care among BHH enrollees before and after program implementation to quality of care over the same period among non-enrollees weighted to equate, on measurable characteristics, to BHH participants (see “Analytic Strategy”).
Data and Study Period
We used Maryland Medicaid administrative claims data from July 1, 2010, to September 30, 2016. Data for the 38 months prior to the BHH program’s start date of October 1, 2013 (July 1, 2010–September 30, 2013) was used to identify the cohort of individuals with diabetes and CVD (details below). We evaluated the effects of the BHH on outcomes of interest from October 1, 2012, to September 30, 2016, encompassing at least 1 year pre- and up to 3 years post-BHH implementation data for each individual in the sample, with variation depending upon when a given BHH participant was enrolled.
Study Sample
The study sample included BHH participants and comparison individuals not participating in Maryland’s BHH program, ages 18–64, who met three criteria. First, enrollment in Maryland Medicaid from October 1, 2012, to September 30, 2013, the year prior to BHH implementation. Second, diagnosis of diabetes or CVD prior to BHH implementation (details below). Third, greater than five psychosocial rehabilitation services during the analytic study period of October 1, 2012–September 30, 2016; as Maryland’s BHH program is implemented in psychiatric rehabilitation programs, only the subset of Medicaid beneficiaries with SMI receiving psychosocial rehabilitation services in such programs were eligible for BHH enrollment. Given that all BHH participants received > 5 psychosocial rehabilitation services, we limited the sample to include comparison participants who received a similar level of psychosocial rehabilitation during the study period (our analytic approach further accounted for individual-level differences in psychosocial rehabilitation service utilization among individuals in the sample; see below).
Individuals with diabetes were defined as those with at least two uniquely dated claims with any diagnosis code from the Healthcare Effectiveness Data and Information Set (HEDIS) diabetes value set or any dispensation of insulin, hypoglycemic/antihyperglycemics, or metformin44 in the 38 months prior to BHH implementation (July 1, 2010, the first month of the Maryland Medicaid fiscal year of July 1, 2010–June 30, 2011 to September 30, 2013, the month prior to BHH implementation). Individuals with CVD were defined as those with any inpatient claim code from the HEDIS myocardial infarction or acute myocardial infarction value sets, or any inpatient or outpatient claim code from the HEDIS coronary artery bypass graft value set, percutaneous coronary intervention value set, or ischemic vascular disease value set44 in the 38 months prior to BHH implementation.
BHH participants met the criteria above and were enrolled in the BHH program at any time point after the program began on October 1, 2013; comparison individuals were those not enrolled. As individuals were enrolled in BHHs on a rolling basis, our marginal structural modeling analytic strategy is designed to account for the potential time-dependent confounding related to this variation.
Measures
All measures were constructed at the person-year level.
Independent Variable
In primary analyses, BHH enrollment was measured as a 0/1 indicator that changed from 0 to 1 in the first year that an individual became enrolled. Consistent with the idea of an intent-to-treat analysis, we assumed that once enrolled, individuals participated in the BHH for the remainder of the study or until they censored out of the sample due to Medicaid disenrollment. In a sensitivity analysis, we defined the independent variable as cumulative years of BHH enrollment per person.
Dependent Variables
Dependent variables were HEDIS CVD risk factor/CVD care quality indicators that can be measured entirely with administrative claims data, specifically measures of quality of diabetes mellitus and CVD care (detailed specifications in Table 3).44 Diabetes quality of care measures, assessed among the full study sample with diabetes as defined above, included annual receipt of diabetic eye and foot exams; hemoglobin A1c monitoring; diabetic nephropathy testing; and cholesterol testing (including total cholesterol, LDL-C, HDL, and/or triglyceride testing). We also measured annual receipt of any statin therapy and statin adherence, defined as receipt of statin prescriptions covering at least 80% of days from initial statin therapy dispensation to end of measurement year, among the subset of individuals with diabetes aged 40–64 without co-morbid diagnoses of CVD. We measured annual receipt of cholesterol testing in the full sample with CVD, and annual receipt of any statin therapy and statin adherence among males with CVD aged 21–64 and females with CVD aged 40–64. For all analyses involving statin measures, individuals with any dispensation for clomiphene and any code from the HEDIS pregnancy, in vitro fertilization, end-stage renal disease, or cirrhosis value sets were excluded. 44 Each of these measures was coded as a dichotomous 0/1 variable, with 1 indicating service receipt.
Covariates
Since BHH participants were enrolled on a rolling basis, our analytic strategy incorporated both time-invariant and time-varying covariates. Time-invariant covariates included baseline age, sex, race/ethnicity, SMI diagnosis type, and size of the patient population of the psychiatric rehabilitation program where each individual in the sample was enrolled; Medicaid managed care organization; and Maryland region of residence. Time-varying covariates were measured in the baseline period (October 2012–September 2013) and during each subsequent year. To ensure these variables were measured prior to the outcomes and exposure of a given time period, they were lagged by one time period. Time-varying covariates included eligibility for Medicaid via disability, co-morbid substance use disorder diagnosis, Elixhauser comorbidity index, number of psychosocial rehabilitation services received, number of visits with a primary care physician, and prior-year quality of cardiovascular care outcomes.
Analytic Strategy
We used a marginal structural modeling approach to account for potential time-dependent confounding and for censoring due to Medicaid disenrollment. We fit the marginal structural model by applying inverse probability of treatment weights for every person-year in the study cohort.45,46,47 These models estimate the effect of an exposure of interest for the entire study population. In our case, the marginal structural modeling approach estimated the effects of BHH enrollment on outcomes using weighting to generate estimates as if the entire study population had been enrolled in a BHH versus not enrolled.
An advantage of the marginal structural modeling (MSM) approach is that, unlike difference-in-differences analyses or regression models with fixed or random effects, MSM can account for confounding due to time-varying variables (e.g., co-morbid substance use disorder diagnosis and Elixhauser comorbidity index) that may be (1) impacted by BHH enrollment and (2) prognostic for future BHH enrollment and the outcome.48 MSMs were specifically designed to handle this type of confounding, which can occur in many settings where the intervention starts at different times for different participants. The MSM approach makes the following assumptions:45 no unobserved confounders; anyone in the reference population is eligible to enroll in BHH; dropout is independent of the outcome conditioned on the observed history; the inverse probability of treatment weight and marginal structural models are correctly specified; and there is no impact of BHH enrollment on the psychosocial rehabilitation service use measure used to define the study sample.
First, we estimated the inverse probability of BHH enrollment for each person-year, adjusting for time-invariant and time-varying confounders. To control for each individual’s history of treatment and other covariates, the weights for each person-year were calculated as the product of the inverse probabilities in prior person-years (see Appendix 2 for full weighting details). Second, we calculated censoring weights to account for factors that may influence censoring (dropout) due to Medicaid disenrollment. We calculated the inverse probability of Medicaid disenrollment for each person-year, adjusting for time-invariant and time-varying confounders; the censoring weight for a given person-year was the product of the inverse probabilities in prior years. The final weight for any given person-year observation was the product of the treatment and censoring weights.
We examined covariate balance in BHH-enrolled versus non-enrolled participants in the baseline period by assessing the absolute difference in the mean value of each baseline covariate between the two groups divided by the standard deviation of the relevant covariate in the entire sample. We then fit weighted logistic regression models (see Appendix 2 for full model specification) to estimate the effect of BHH enrollment on outcomes adjusting for year. To facilitate interpretation of results, we calculated the predicted probability of annual receipt of each measure of guideline-concordant care among BHH enrollees and non-enrollees. In a sensitivity analysis, we examined the effects of total years of BHH enrollment on outcomes. This study was deemed exempt by the Johns Hopkins School of Medicine Institutional Review Board.
RESULTS
The diabetes sample included 914 BHH and 1691 non-BHH–enrolled individuals with SMI, 277 of whom were censored during the study period due to Medicaid disenrollment. Of the 919 BHH participants with diabetes, 72% (N = 661) were enrolled in the year 1 of implementation of Maryland’s BHH program; 19% (N = 176) were enrolled in year 2; and 8% (N = 77) were enrolled in year 3. The CVD sample included 601 BHH and 1298 non-BHH–enrolled participants, 195 of whom were censored during the study period due to Medicaid disenrollment. Of these, 70% (N = 420) were enrolled in year 1; 19% (N = 114) in year 2; and 11% (N = 67) in year 3.
For both the diabetes and CVD samples, the unweighted baseline characteristics of the BHH-enrolled and non-enrolled groups differed, underscoring the need for weighting (Table 1). Weighting improved covariate balance: at baseline, the average absolute standardized mean difference of covariate values between the BHH and weighted comparison groups in the diabetes and CVD (Figs. 1 and 2) samples was near or below 20%, a cut point used to mark good covariate balance.47
BHH enrollment was associated with increased likelihood of annual eye exam receipt (OR 1.86, 95% CI 1.19–2.91) among those study participants with SMI and diabetes (Table 2). BHH enrollment had no statistically significant effects on any of the other measures of guideline-concordant diabetes or CVD care examined. Results of the sensitivity analysis (Table 4) showed that the duration of BHH enrollment did not affect outcomes.
DISCUSSION
Our study is the first to examine the effects of a state Medicaid BHH program created through the ACA Medicaid health home waiver on receipt of guideline-concordant cardiovascular care among individuals with SMI. Findings suggest that the BHH did not achieve the goals of either primary prevention of CVD among those with diabetes or secondary prevention among those who had already experienced a myocardial infarction or CVD procedure. BHH enrollment was associated with improvement on a single indicator of guideline-concordant care: likelihood of eye exam receipt among individuals with diabetes. Eye exams may be “low hanging fruit,” in that they are minimally invasive and straightforward for providers to conduct and individuals with SMI to complete. Further, qualitative studies have found that individuals with diabetes are highly motivated to protect their vision.49,50 Only two prior studies have assessed the effects of a BHH on quality of cardiovascular care. The results of one clinical trial showed that a BHH implemented in a community mental health clinic improved receipt of guideline-concordant diabetes and hypertension, but not dyslipidemia, care (our study’s use of administrative claims data precluded us from assessing quality of hypertension and dyslipidemia care, as our data does not include laboratory results).37 Similar to our findings, an evaluation of another real-world, SAMHSA grant–funded51 BHH program found no effect of BHHs implemented in seven New York community mental health centers on HbA1c monitoring among participants with diabetes.52 These findings suggest that while the BHH model holds promise for improving cardiovascular care quality, additional resources and supports to ensure high-fidelity implementation in real-world settings may be needed.
Prior studies by our team examined implementation of Maryland’s BHH program.36,53 Key challenges included difficulty coordinating care with PCPs and lack of effective health IT infrastructure.36 Only 15% of Maryland’s BHHs have a co-located PCP, none of whom work full-time at the psychiatric rehabilitation program implementing the BHH.36 As all BHH participants are allowed to choose their own PCP, BHH staff at sites with co-located PCPs reported that not all participants used the on-site provider. Relatedly, Maryland BHH programs do not have shared electronic medical records with the various PCPs serving their participants with SMI in the community.36 These challenges are consistent with those identified in other BHH programs.38,54,55,56,57
In Maryland, BHHs receive a $102.86 per-member monthly payment for delivering at least two health home services to each enrolled participant.40,43 As 100% of this payment goes to the psychiatric rehabilitation program implementing the BHH, external providers have no financial incentive to participate in care coordination for BHH participants with SMI. Alternative structures such as hub-and-spoke58 or accountable care organization models33 that can create funding streams for both the community mental health programs implementing BHHs and external primary care partners may help facilitate guideline-concordant cardiovascular care. Integrating BHHs into accountable care organizations may also support delivery of guideline-concordant cardiovascular care by tying payment incentives to performance metrics, such as the HEDIS measures examined in this study.59
Maryland’s BHH program is implemented in psychiatric rehabilitation programs, whereas other states implementing BHHs through the ACA Medicaid health home waiver do so in community mental health clinics.34 While the organizational structure and implementation challenges encountered in Maryland are similar to those that have been documented in outpatient mental health clinic BHHs38,54,55,56,57—and this study’s results were consistent with those of an evaluation of a BHH program implemented in New York community mental health centers52—future research should consider differences in BHH implementation and outcomes in less clinical settings, like psychiatric rehabilitation programs, relative to more clinical specialty mental health settings. A potential benefit of implementation in psychiatric rehabilitation programs which exist in all 50 US states60 is that they serve the high-need subset of people with SMI with significant functional impairment.
Our results should be interpreted in the context of potential limitations. We examined quality of cardiovascular care outcomes 3 years post-BHH implementation, though due to the rolling nature of BHH enrollment in Maryland, about 30% of our study sample were enrolled in the BHH program in year 2 or 3; longer term follow-up studies are needed. Measures of receipt of statin therapy were based on prescription fills, and were unable to measure patients’ medication adherence with claims data. While our analyses accounted for censoring due to Medicaid disenrollment, the claims data did not include information on reason for disenrollment. In addition, we were unable to determine which patients saw a PCP co-located within a BHH program. Tobacco smoking is a significant source of cardiovascular risk in SMI,61 but due to a lack of claims-based measures, guideline-concordant cessation treatment was not examined in our study. Our claims-based measures may be subject to measurement error due to incomplete documentation of the CPT codes by healthcare providers. Our marginal structural modeling analysis assumes no unobserved confounding and correct model specification. A possible extension of this research is to apply alternative robust methods for fitting the marginal structural model.62,63,64
CONCLUSIONS
Additional financing, infrastructure, and implementation supports may be needed to realize the potential of Maryland’s BHH to improve cardiovascular care for people with SMI.
References
Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature mortality among adults with schizophrenia in the United States. JAMA psychiat. 2015;72(12):1172–1181.
Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry. 1997;171:502–508.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? . Arch Gen Psychiatry. 2007;64(10):1123–1131.
Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Rsearch Database. Arch Gen Psychiatry. 2007;64(2):242–249.
Daumit G, Anthony C, Ford DE, et al. Pattern of mortality in a sample of maryland residents with severe mental illness. Psychiatry Res. 2010;176(2–3):242–245.
Osborn DP, Wright CA, Levy G, King MB, Deo R, Nazareth I. Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: systematic review and metaanalysis. BMC Psychiatry. 2008;8:84–98.
Compton MT, Daumit GL, Druss BG. Cigarette smoking and overweight/obesity among individuals with serious mental illness: a preventive perspective. Harv Rev Psychiatry. 2006;14(4):212–222.
Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284(20):2606–2610.
Lê Cook B, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311(2):172–182.
Daumit G, Goldberg R, Anthony C, et al. Physical Activity Patterns in Adults with Severe Mental Illness. J Nerv Ment Dis. 2005;193(10):641–646.
Jerome GJ, Young DR, Dalcin A, et al. Physical activity levels of persons with mental illness attending psychiatric rehabilitation programs. Schizophr Res. 2009;108(1–3):252–257.
Henderson DC, Borba CP, Daley TB, et al. Dietary intake profile of patients with schizophrenia. Ann Clin Psychiatry. 2006;18(2):99–105.
Casey DE. Metabolic issues and cardiovascular disease in patients with psychiatric disorders. Am J Med. 2005;118 Suppl 2:15S–22S.
McGinty EE, Daumit GL. Epidemiology of Obesity. Psychiatr Ann. 2011;41(10):484–488.
Mueser KT, McGurk SR. Schizophrenia. Lancet. 2004;363(9426):2063–2072.
Julian Chun-Chung C, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. 2003;93(5):792–797.
Steadman HJ, Osher FC. Pamela Clark Robbins B, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatr Serv. 2009;60(6):761–765.
Lamb HR, Weinberger LE. Persons with severe mental illness in jails and prisons: a review. New directions for mental health services. 2001;(90):29–49.
Calloway MO, Morrissey JP. Overcoming service barriers for homeless persons with serious psychiatric disorders. Psychiatr Serv. 1998;49(12):1568–1572.
Draine J, Salzer MS, Culhane DP, Hadley TR. Roles of Social Disadvantage in Crime, Joblessness, and Homelessness Among Persons with Serious Mental Illness. Psychiatr Serv. 2002;53(5).
Drake RE, Skinner JS, Bond GR, Goldman HH. Social Security And Mental Illness: Reducing Disability With Supported Employment. Health Aff. 2009;28(3):761–770.
Perkins R, Rinaldi M. Unemployment rates among patients with long-term mental health problems: A decade of rising unemployment. Psychiatr Bull. 2002;26(8):295–298.
Druss BG. The mental health/primary care interface in the United States: history, structure, and context. Gen Hosp Psychiatry. 2002;24:2002.
Druss BG, Bornemann TH. Improving health and health care for persons with serious mental illness: the window for US federal policy change. JAMA. 2010;303(19):1972–1973.
Frank RG, Glied SA. Better but not well: Mental health policy in the United States since 1950. Baltimore: Johns Hopkins University Press; 2006.
Druss BG, Bradford WD, Rosenheck RA, Radford MJ, Krumholz HM. Quality of medical care and excess mortality in older patients with mental disorders. Arch Gen Psychiatry. 2001;58(6):565–572.
Banta JE, Morrato EH, Lee SW, Haviland MG. Retrospective analysis of diabetes care in california medicaid patients with mental illness. J Gen Intern Med. 2009;24(7):802–808.
Clark RE, Weir S, Ouellette RA, Zhang J, Baxter JD. Beyond health plans: behavioral health disorders and quality of diabetes and asthma care for Medicaid beneficiaries. Med Care. 2009;47(5):545–552.
Frayne SM, Halanych JH, Miller DR, et al. Disparities in diabetes care: impact of mental illness. Arch Intern Med. 2005;165(22):2631–2638.
Goldberg RW, Kreyenbuhl JA, Medoff DR, et al. Quality of diabetes care among adults with serious mental illness. Psychiatr Serv. 2007;58(4):536–543.
McGinty EE, Baller J, Azrin ST, Juliano-Bult D, Daumit GL. Quality of medical care for persons with serious mental illness: A comprehensive review. Schizophr Res. 2015;165(2–3):227–235.
Khaykin E, Eaton WW, Ford DE, Anthony CB, Daumit GL. Health insurance coverage among persons with schizophrenia in the United States. Psychiatr Serv. 2010;61(8):830–834.
Bao Y, Casalino LP, Pincus HA. Behavioral health and health care reform models: patient centered medical home, health home, and accountable care organization. J Behav Heal Serv Res. 2013;40:121–132.
Centers for Medicare and Medicaid Services. Health Home Information Resource Center. https://www.medicaid.gov/state-resource-center/medicaid-state-technical-assistance/health-homes-technical-assistance/health-home-information-resource-center.html, Accessed March 8, 2019. 2019.
Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of adults with severe mental illnesses. Health Aff (Project Hope). 2006;25(3):659–669.
McGinty EE, Kennedy-Hendricks A, Linden S, Choksy S, Stone E, Daumit GL. An innovative model to coordinate healthcare and social services for people with serious mental illness: A mixed-methods case study of Maryland's Medicaid health home program. Gen Hosp Psychiatry 2018;51:54–62.
Druss BG, von Esenwein SA, Glick GE, et al. Randomized Trial of an Integrated Behavioral Health Home: The Health Outcomes Management and Evaluation (HOME) Study. Am J Psychiatry. 2017;174(3):246–255.
Scharf DM, Eberhart NK, Schmidt N, et al. Integrating primary care into community behavioral health settings: programs and early implementation experiences. Psychiatr Serv. 2013;64(7):660–665.
Yawn BP, Dietrich A, Graham D, et al. Preventing the voltage drop: keeping practice-based research network (PBRN) practices engaged in studies. J Am Board Fam Med 2014;27(1):123–135.
Maryland Department of Health and Mental Hygiene. Maryland Chronic Health Homes. https://mmcp.dhmh.maryland.gov/pages/health-homes.aspx, Accessed March 8, 2019. 2019.
Beacon Health Options. 6.12. Mental Health - Psychiatric Rehabilitation Program (PRP). http://maryland.beaconhealthoptions.com/provider/manual/CH06_12-MH-PRP.pdf, Accessed May 14, 2017. 2017.
Maryland Department of Health and Mental Hygiene. Maryland Medicaid Chronic Health Homes Quarterly Report. https://mmcp.health.maryland.gov/SiteAssets/SitePages/Health%20Home%20Program%20Updates/Quarterly%20Health%20Home%20Report-%20July%20-%20September%202016.pdf, Accessed June 24, 2019. 2016.
Maryland Department of Health and Mental Hygiene. Maryland Health Home State Plan Amendment. https://www.medicaid.gov/state-resource-center/medicaid-state-technical-assistance/health-homes-technical-assistance/downloads/maryland-spa-13-15.pdf. 2013.
National Committee for Quality Assurance. HEDIS 2017 Volume 2: Technical Specifications for Health Plans. Item #10284–100-17. 2016.
Fewell Z, Hernán MA, Wolfe F, Tilling K, Choi H, Sterne JA. Controlling for time-dependent confounding using marginal structural models. Stata J. 2004;4(4):402–420.
Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. LWW; 2000.
Griffin BA, Ramchand R, Almirall D, Slaughter ME, Burgette LF, McCaffery DF. Estimating the causal effects of cumulative treatment episodes for adolescents using marginal structural models and inverse probability of treatment weighting. Drug Alcohol Depend. 2014;136:69–78.
Scharfstein DO, Rotnitzky A, Robins JM. Adjusting for nonignorable drop-out using semiparametric nonresponse models. J Am Stat Assoc. 1999;94(448):1096–1120.
Lake AJ, Browne JL, Rees G, Speight J. What factors influence uptake of retinal screening among young adults with type 2 diabetes? A qualitative study informed by the theoretical domains framework. J Diabetes Complicat. 2017;31(6):997–1006.
van Eijk KND, Blom JW, Gussekloo J, Polak BCP, Groeneveld Y. Diabetic retinopathy screening in patients with diabetes mellitus in primary care: Incentives and barriers to screening attendance. Diabetes Res Clin Pract. 2012;96(1):10–16.
Substance Abuse and Mental Health Administration (SAMHSA). SAMHSA Primary and Behavioral Health Care Integration Program. http://www.integration.samhsa.gov/about-us/pbhci. 2017.
Breslau J, Leckman-Westin E, Yu H, et al. Impact of a mental health based primary care program on quality of physical health care. Adm Policy Ment Health Ment Health Serv Res. 2018;45(2):276–285.
Daumit GL, Stone EM, Kennedy-Hendricks A, Choksy S, Marsteller JA, McGinty EE. Care Coordination and Population Health Management Strategies and Challenges in a Behavioral Health Home Model. Med Care. 2019;57(1):79–84.
Murphy KA, Daumit GL, Stone EM, McGinty EE. Physical Health Outcomes and Implementation of Behavioral Health Homes: A Comprehensive Review. Int Rev Psychiatry. In Press. 2019.
Scharf DM, Breslau J, Hackbarth NS, Kusuke D, Staplefoote BL, Pincus HA. An examination of New York State’s integrated primary and mental health care services for adults with serious mental illness. Rand Health Q. 2014;4(3).
Golembiewski EH, Askelson NM, Bentler SE, Damiano PC, Momany ET. Evaluation of the Integrated Health Home (IHH) program in Iowa: Qualitative interviews with site administrators. 2015.
Maragakis A, RachBeisel J. Integrated care and the behavioral health home: A new program to help improve somatic health outcomes for those with serious mental illness. J Nerv Ment Dis. 2015;203(12):891–895.
Brooklyn JR, Sigmon SC. Vermont hub-and-spoke model of care for opioid use disorder: development, implementation, and impact. J Addict Med. 2017;11(4):286.
Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care—two essential elements of delivery-system reform. N Engl J Med. 2009;361(24):2301–2303.
Psychiatric Rehabilitation Association. Individual Directory. https://netforum.avectra.com/eweb/DynamicPage.aspx?Site=praandprf&WebCode=IndSearch, Accessed December 13, 2017. 2017.
Evins AE, Cather C, Laffer A. Treatment of tobacco use disorders in smokers with serious mental illness: toward clinical best practices. Harv Rev Psychiatry. 2015;23(2):90.
Robins JM. Robust estimation in sequentially ignorable missing data and causal inference models. Paper presented at: Proceedings of the American Statistical Association2000.
Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005;61(4):962–973.
van der Laan MJ, Gruber S. Targeted minimum loss based estimation of causal effects of multiple time point interventions. Int J Biostat. 2012;8(1).
Funding
The authors gratefully acknowledge support from NIMH grants K01MH106631, P50MH115842, and R24MH102822.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Appendix 2 Marginal Structural Model Estimation
Confounders
Observed time-invariant confounders included (as measured at baseline) the following: (i) age, (ii) sex, (iii) race/ethnicity, (iv) psychiatric diagnosis, (v) the psychiatric rehabilitation patient population size at the organization where the individual received the plurality of their psychosocial rehabilitation services; (vi) indicator for enrollment in one of nine possible Medicaid managed care organizations, and (vii) region of residence. Observed time-varying variables included the following: (i) eligibility for Medicaid via disability, (ii) substance use disorder diagnosis, (iii) co-morbidity (measured via Elixhauser index), (iv) number of psychosocial rehabilitation services received, (v) past visits with a primary care clinician, and (vi) past quality of care outcomes. Time-varying variables were measured in the pre-intervention (October 2012–September 2013) and during each 1-year period throughout the study. To ensure these variables were measured prior to the outcomes and exposure of a given time period, they were lagged by one time period.
Treatment Weights
At each person-year observation, the estimated treatment weight was calculated as such: Let Aij denote individual i’s treatment assignment (BHH enrollment) at time period j (A_ij = 1 indicates individual i is enrolled in a BHH at time j, and A_ij = 0 otherwise). Let Lij denote the vector of time-invariant and time-varying confounders observed for subject i at time period j. Let \( \overline{L} \)ij and \( \overline{A} \)ij represent the ith individual’s observed covariate and treatment history up through time j. By assumption, each individual i who enrolls in a BHH during the intervention period has \( \overline{A} \)ij equal to a vector of 0’s before their year of enrollment followed by 1’s; each individual who does not enroll in BHH has \( \overline{A} \)ij equal to (0,0,0). The weight for each person-year observation was defined as:
Each term in the numerator was the conditional probability of the ith individual receiving their assigned treatment (BHH enrollment or not), given past treatment assignment. Each term in the denominator was the conditional probability of the ith individual receiving their assigned treatment, given past treatment assignment and the observed time-invariant and time-varying covariates up until time j.
Censoring Weights
At each person-year observation, the estimated censoring weight was calculated as such: Let Cij denote if individual i is censored in time period j + 1 (C_ij = 1 indicates individual i is not censored in time period j + 1, and A_ij = 0 otherwise). Let Lij denote the vector of time-invariant and time-varying confounders observed for subject i at time period j. Let \( \overline{L} \)ij and \( \overline{C} \)i,j-1 represent the ith individual’s observed covariate and censoring history up through time j. The weight for each person-year observation at year t was defined as:
Each term in the numerator was the conditional probability of the ith individual receiving their assigned censoring status, given past censoring. Each term in the denominator was the conditional probability of the ith individual receiving their assigned censoring status given past censoring and the observed time-invariant and time-varying covariates up until time j. We assumed the only form of censoring was right censoring, i.e., dropout.
Final Weights
The final weight for any given person-year observation was the product of the censoring and treatment weight. To control for high variability, weights were truncated to the value of the 1st percentile and at the value of the 99th percentile of the weight distribution. Weight estimation was conducted with adaptations to Stata code developed by Fewell and colleagues.45
Weighted Regression Model
The marginal structural model for each outcome is a logistic regression model with main terms for year (1–3, or) and for BHH enrollment during the current year. For participants who dropped out of Medicaid and later re-enrolled, we only use their data up through the time when they dropped out. We fit the following weighted logistic regression model to estimate results: Pr(Outcome Eventij) = B0 + B1(HealthHomeij) + B2(Year), where HealthHomeij represents any enrollment in a given person-year period. This marginal structural model approach makes the following assumptions: no unobserved confounders; anyone in the reference population is eligible to enroll in BHH; dropout is independent of the outcome conditioned on the observed history; our models are correct; and each participant’s data vector is an independent, identically distributed draw from an unknown joint distribution. The last assumption is implicitly made in many types of analyses (e.g., analyses using fixed effects), though often it is not explicitly stated.
Appendix 3
Difference in baseline covariates in weighted versus unweighted samples of behavioral health home enrolled and non-enrolled participants, diabetes sample (N = 2605). The average absolute standardized mean difference of covariate values between the BHH and weighted comparison groups in the diabetes sample. The vertical dashed line indicates 20% standardized mean difference, a cut point used to mark good covariate balance.47 PTSD = post-traumatic stress disorder; MCO = managed care organization.
Difference in baseline covariates in weighted versus unweighted samples of behavioral health home enrolled and non-enrolled group participants, cardiovascular disease sample (N = 1899). The average absolute standardized mean difference of covariate values between the BHH and weighted comparison groups in the cardiovascular disease sample. The vertical dashed line indicates 20% standardized mean difference, a cut point used to mark good covariate balance.47 PTSD = post-traumatic stress disorder; MCO = managed care organization; CVD = cardiovascular disease.
Appendix 4
Rights and permissions
About this article
Cite this article
McGinty, E.E., Stone, E.M., Kennedy-Hendricks, A. et al. Effects of Maryland’s Affordable Care Act Medicaid Health Home Waiver on Quality of Cardiovascular Care Among People with Serious Mental Illness. J GEN INTERN MED 35, 3148–3158 (2020). https://doi.org/10.1007/s11606-020-05690-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-05690-9