Abstract
Background
The socioeconomic status (SES) gradient in hospital and emergency room utilization among adults with type 2 diabetes (T2DM) is partially driven by cost-related non-adherence.
Objective
To test the impact of the Diabetes Health Plan (DHP), a diabetes-specific health plan incorporating value-based insurance design principles on healthcare utilization among low-income adults with T2DM.
Design
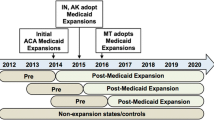
To examine the impact of the DHP on healthcare utilization, we employed a difference-in-differences (DID) study design with a propensity-matched comparison group. We modeled count and dichotomous outcomes using Poisson and logit models, respectively.
Participants
Cohort of adults (18–64) with T2DM, with an annual household income <$ 30,000, and who were continuously enrolled in an employer-sponsored UnitedHealthcare plan for at least 2 years between 2009 and 2014.
Interventions
The DHP reduces or eliminates out-of-pocket costs for disease management visits, diabetes-related medicines, and diabetes self-monitoring supplies. The DHP also provides access to diabetes-specific telephone case management as well as other online resources.
Main Measures
Number of disease management visits (N = 1732), any emergency room utilization (N = 1758), and any hospitalization (N = 1733), within the year.
Key Results
DID models predicting disease management visits suggested that DHP-exposed beneficiaries had 1.7 fewer in-person disease management visits per year (− 1.70 [95% CI: − 2.19, − 1.20], p < 0.001), on average, than comparison beneficiaries. Models for emergency room (0.00 [95% CI: − 0.06, 0.06], p = 0.966) and hospital utilization (− 0.03 [95% CI: − 0.08, − 0.01], p = 0.164) did not demonstrate statistically significant changes associated with DHP exposure.
Conclusions
While no relationship between DHP exposure and high-cost utilization was observed in the short term, fewer in-person disease management visits were observed. Future studies are needed to determine the clinical implications of these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The prevalence of diabetes has increased over the past two decades in the USA, disproportionately affecting populations with low incomes. Between 2011 and 2014, compared with persons with high income, the relative percentage increase in diabetes prevalence was 40.0%, 74.1%, and 100.4% for those classified as middle income, near poor, and poor, respectively.1 Furthermore, studies have found a socioeconomic gradient in diabetes-related complications and healthcare utilization.2 Non-adherence to medications and treatment recommendations due to cost is an important driver of the socioeconomic status (SES) gradient in morbidity among adults with diabetes.3 Although isolated copayments for medications and medical visits may be low, taken in the aggregate, these costs may pose a financial burden for individuals with low incomes, forcing tradeoffs between medical care and basic necessities.4 Consequently, patients may opt to forgo needed treatments, leading to diabetes-related complications. Cross-sectional studies have demonstrated a negative relationship between medication adherence, emergency room utilization, and hospitalizations.5,6,7
Methodologically rigorous studies suggest that health insurance plans that incorporate value-based insurance design (VBID) principles such as lowering out-of-pocket costs for medications used to treat chronic disease may be particularly effective for improving medication adherence among patients with low SES, but few studies have evaluated the healthcare utilization effects of such plans among this subpopulation. Choudhry et al. found that a randomized control trial in which patients with a recent myocardial infarction were randomized to either a health insurance plan that eliminated co-insurance, copayments for disease management visits, and copayments for secondary prevention medications, or usual health insurance coverage, reduced racial/ethnic disparities in major vascular events or revascularization among the intervention group.8 Observational studies of the utilization implications of health insurance plans incorporating VBID principles among the broader patient population have demonstrated reductions in emergency room utilization and hospitalization among these beneficiaries; however, it is not clear that these findings can be extrapolated to populations with low SES.9 There may be differences in health literacy, self-management knowledge, access to primary care, and other social determinants of health that translate into different healthcare utilization implications of these types of health insurance plans among the subpopulation with low socioeconomic status.10 Given the upfront costs to insurers of incorporating VBID principles into health insurance plans and associated costs due to increases in medication adherence, it will be important to have information regarding how healthcare utilization may be impacted among one of the most affected subpopulations of beneficiaries. The objective of this study is to examine the impact of the Diabetes Health Plan (DHP), (the first condition-specific health insurance plan based on VBID principles), on healthcare utilization among beneficiaries with low household incomes (< $30 K annually).
In 2009, UnitedHealthCare (UHC) introduced the DHP which includes financial incentives to encourage patient engagement in evidence-based diabetes care, including reduced or eliminated out-of-pocket patient expenses for disease management visits; free diabetes self-monitoring training and supplies; and reduced or eliminated out-of-pocket expenses for diabetes-related medicines (Table 1).11,12 The DHP also provides access to diabetes-specific telephone case management as well as other online resources. Additionally, the DHP provides scorecards with reminders to complete health maintenance activities, such as biannual hemoglobin A1C and cholesterol screening and an annual retinal eye exam. Overall, the DHP provides between $150 and 500 in annual out-of-pocket savings for enrollees.13 The DHP standard benefit design can be modified by purchasing employers to better suit the needs of beneficiaries, which include both employees and their dependents. Uptake of the DHP, across employers, has spanned the years since 2009 and varied across years. Some employers use an opt-in enrollment strategy (employees must choose to participate) while others use an opt-out strategy (all eligible employees enrolled initially). Studies have shown that DHP uptake can range from a low of 8% among opt-in plans to a high of 85% for opt-out plans.14 Additionally, studies have shown variability in the demographic characteristics of DHP participants as a consequence of the enrollment strategy. Specifically, Kimbro et al. found that DHP participants enrolled in an opt-out plan were more likely to be dependents, were more racially and ethnically diverse, and had a broader range of incomes and educational backgrounds relative to participants enrolled in opt-in plans, who tended to have higher incomes and more education and who were less likely to be Hispanic.12 Studies have previously demonstrated the beneficial impact of the DHP on medication adherence and emergency room utilization among the broader cohort of beneficiaries.13,15 However, the results of studies examining the effects of the DHP among low-income beneficiaries have been mixed. Huang et al. found no relationship between the DHP and medication adherence among beneficiaries with household incomes of $50,000 or less.16 While Narain et al. found that the DHP was associated with improved adherence to oral hypoglycemic medications among beneficiaries with household incomes $30,000 or less and low baseline medication adherence.17
METHODS
Data Source and Population
The analytic data set is limited to 26 large employer groups that purchased the DHP and standard benefit plans from UHC (2009–2014) that have (1) internal pharmacy contracts, (2) complete pharmacy claims data, (3) sufficient medical claims and lab data to identify employees with type 2 diabetes (T2DM), and (4) fewer than 15% of employees enrolled in high deductible health plans. In addition to the above-mentioned criteria, the DHP employer groups must have at least 1 year of standard benefit plan data, prior to the purchase of the DHP, and comparison employer groups are further limited to those that have overlapping propensity scores with DHP employers after employer-level matching (described further below) and who have at least 2 years of continuous enrollment in the standard benefit plan during the duration of the match to the DHP employer.
A diabetes diagnosis was defined as having any of the following prior to the implementation of the DHP: (1) at least one 250.X ICD-9 diagnosis code from an inpatient, outpatient, or emergency department claim; (2) hemoglobin A1C laboratory value of 6.5% or greater or a 2-h value on an oral glucose tolerance test of greater than 200 mg/dl; or (3) at least one prescription fill for an oral hypoglycemic medication other than metformin or insulin. Estimated household income is obtained from the AmeriLINK data.18 This data source incorporates consumer financial survey responses, publicly available information (public records, census information, and retail transaction records), and zip-code-level information from the Internal Revenue Service to generate individual-level estimates of household income. The sample size flow chart for the unique DHP and comparison beneficiaries are shown in Figures 1 and 2, respectively.
Propensity Score Matching
Matching criteria for both the DHP and comparison employers were derived with respect to the 12-month period preceding the date of DHP adoption for the DHP employers or standard insurance plan contract renewal (the index date). The matching criteria included the following as reported by UHC: average employee salary, geographic region, number of employees, % female, % in each racial/ethnic category (White, Black, Asian, Hispanic), health benefit plan generosity, % of employees with a HDHP, and % of beneficiaries with each one of the following claims-based co-morbidities (hypertension, hyperlipidemia, coronary artery disease, anxiety/depression, dementia, osteoarthritis, rheumatoid arthritis, non-skin cancer, chronic obstructive pulmonary disease, congestive heart failure, atrial fibrillation, end-stage renal disease, peripheral vascular disease, stroke, schizophrenia) as well as the index date. A single comparison employer could be matched to more than one DHP employer. Individual-level matching criteria were based on the following pre-index date criteria: race and ethnicity, age, gender, Charlson Comorbidity Index, insulin use status, presence of any diabetes complication (retinopathy, nephropathy, neuropathy, cardio/peripheral vascular disease, history of a diabetes-related hospitalization), and baseline healthcare utilization. Nearest-neighbor matching was conducted with replacement using a caliper equal to 25% of the propensity score standard deviation, in an effort to get 3 comparison matches for each DHP beneficiary.19 The employer and beneficiary matching was done using PROC PSMATCH in SAS version 9.4.
Outcomes
We coded “disease management visits” as a count variable based on the composite number of outpatient visits with providers who may perform diabetes management during the course of a visit (endocrinologist, internal medicine, family practice, urgent care specialist, nurse practitioner, physician assistant). Patients with an unusually high number of disease management appointments in the baseline year were excluded from this analysis prior to matching using the 1.5 interquartile range heuristic for identifying outliers.20 We treated emergency room and hospital utilization as dichotomous variables. Both variables were indicators coded as “1” if the utilization was present during the post-period year and coded as “0” if the utilization was not present. These utilization outcomes were not restricted to those exclusively related to diabetes.
Statistical Analyses
We used a DID study to examine the impact of the DHP on utilization. The key assumption of the DID study is the parallel trends assumption which necessitates that the pre-intervention trends for outcome measures across the treatment and comparison groups are the same.21 If the parallel trend assumption is met, any difference in the pre-post intervention change in slope across treatment and comparison groups is attributed to intervention effects. We use the propensity-matched sample to increase the likelihood that the DHP and comparison groups have a similar trend of utilization during the pre-intervention time period.22 Non-linear statistical models were run for each of the utilization outcomes using the PROC GENMOD procedure in SAS. The model used for disease management visits employed a Poisson distribution with a log link function, and binomial logit models were used to model emergency room and hospital utilization. These models include an indicator for time (post-index vs. pre-index) that was coded as “1” if the observation was from the post-index year and coded as “0” if the observation was from the pre-index (baseline) year, and an indicator for group (DHP group vs. comparison group) that was coded as “1” if the observation was from the DHP group and coded as “0” if the observation was from the comparison group and the interaction between time and group, among our matched samples. Specifically, the between-group differences in the change of the outcome variables, post-index, were estimated by the interaction effects.
Sensitivity Analyses
We conducted an additional test to assess the sensitivity of our results to selection bias by repeating the above-mentioned analyses with DHP employers that use an opt-out enrollment strategy as the sole source of the treatment population. This methodological change should allow for evaluation of the DHP utilization effects among a less motivated subset of beneficiaries than the subset including individuals that proactively enrolled in the DHP.12
RESULTS
The final analytic samples were 1732, 1758, and 1733 matches with replacement for disease management visits, emergency room use, and hospitalizations, respectively. Across all three samples, prior to matching, the DHP sample was older, had a higher proportion of females, was more likely to be non-Hispanic Black, was more likely to have a diabetes complication, and had a higher Charleston Co-morbidity Index (Tables 2, 3 and 4). Post-matching mean standardized differences for all covariates included in the propensity score models are < 0.1, across the DHP and comparison beneficiaries, indicating sufficient matching.19
DID models predicting disease management visits suggested that DHP-exposed beneficiaries had 1.7 fewer disease management visits per year, on average, than comparison beneficiaries ([95% CI: − 2.19, − 1.20], p < 0.001; Table 5). Models for emergency room (0.00 [95% CI: − 0.06, 0.06], p = 0.966) and hospital utilization (− 0.03 [95% CI: − 0.08, − 0.01], p = 0.164) did not demonstrate statistically significant changes associated with DHP exposure. In sensitivity analyses including only employers enrolling DHP beneficiaries using an opt-out strategy as the treatment population, once again, we find a negative association between DHP exposure and disease management visits, with DHP beneficiaries visiting providers 2.0 fewer times, on average, 1 year after exposure compared to controls (95% CI: − 2.7, − 1.4, p < 0.001), but no association with emergency room (− 0.05 [95% CI: − 0.13, 0.02], p = 0.165) or hospital utilization (0.00 [95% CI: − 0.06, 0.06], p = 0.982; Table 6).
DISCUSSION
Using a strong quasi-experimental study design, we evaluated the relationship between the DHP exposure and healthcare utilization among low-income beneficiaries. Our findings of a negative association between DHP exposure and disease management visits in the absence of an association with emergency room and hospital utilization make an important contribution to the literature, as this is the only study to our knowledge to assess the relationship between the DHP and healthcare utilization at the individual level and the only study to our knowledge to assess this relationship among a cohort of beneficiaries with low household incomes. The robustness of the results to sensitivity analyses conducted using only DHP-exposed beneficiaries enrolled using an opt-out strategy lends credibility to the findings by lowering the likelihood that the observed results are merely a product of selection bias.
While a decline in disease management visits associated with the DHP seems somewhat counterintuitive, plausible explanations include reduced disease management visits in the setting of reduced clinical need and/or substitution of some disease management visits with telephone case management visits. However, we lack data points such as HbA1c values and the frequency of telephone case management visits that could help to further elucidate the mechanisms driving these results. An alternative explanation for these results is reduced access to care driven by the DHP. However, this explanation is less likely given that there is no accompanying increase in emergency room utilization. Furthermore, the positive association between the DHP and oral hypoglycemic medication adherence among beneficiaries with low household incomes (< $30 K annually) and low baseline medication adherence found by Narain et al. makes this explanation less likely.17 With respect to the emergency room and hospitalization findings, we suspect that a relatively short study time horizon may have contributed to the null results. Emergency room and hospital utilization among diabetes patients typically stems from the complications of chronic diseases associated with long-standing diabetes such as congestive heart failure and coronary artery disease.23 The prevalence of congestive heart failure and coronary artery disease for individuals in our study sample is only roughly 3% and 10% respectively.
Our results for ER utilization diverge from that of the Moin et al. study which find reductions in ER utilization associated with DHP exposure.15 These differences may stem from differences in the study designs. Specifically, differences between the study populations used in the Moin et al. study and this study include analysis of beneficiaries of all income levels rather than an emphasis on beneficiaries with low household incomes and inclusion of beneficiaries with both pre-diabetes and diabetes while we restrict our sample to beneficiaries with diabetes. Additionally, the Moin et al. study findings are based on an employer-level analysis rather than an individual-level one. As such, they propensity score match at the employer level while we propensity score match at both the employer and individual levels.
The study results must be viewed in the context of some important limitations. A key underlying assumption of the DID approach is that secular time trends for the DHP-exposed and comparison beneficiaries do not differ in the pre-treatment time period. We use propensity score matching in an effort to ensure similarity of pre-treatment secular time trends across the DHP-exposed and comparison beneficiaries, but this strategy does not account for differences in unmeasurable factors. Our study approach also reflects an intent-to-treat design which may result in beneficiaries without DHP insurance coverage being included in the treatment population. Consequently, DHP effect estimates may be biased towards the null. However, this intent-to-treat design reduces the risk of selection bias being a plausible explanation for our results. Additionally, given that our data source is claims data, we lack data on health outcomes that could be valuable for providing context to the study results. Lastly, our results also reflect average effect estimates for the DHP. As such, effects may vary across DHP implementation strategies.
We do not find changes in emergency room and hospital utilization among DHP-exposed beneficiaries with low household incomes. These null findings may be attributable to a relatively healthy and young study population in addition to a relatively short duration of follow-up.9 In light of the DHP-associated benefits for medication adherence found by Narain et al., studies with a larger sample size, which can stratify populations across co-morbidity level and which can follow DHP-exposed and comparison beneficiaries over a longer time horizon, may find more favorable results.17 Nonetheless, we do find a negative association between DHP exposure and reduced disease management visits which may engender some cost savings that can be used to offset the cost of implementing the program. Additionally, fewer in-person disease management visits may translate into less missed work and higher levels of employee productivity, potentially leading to indirect cost savings for employers associated with the DHP in a relatively short time frame.24
CONCLUSION
We used strong quasi-experimental studies and administrative/pharmacy claims data to evaluate the effect of the Diabetes Health Plan (the first disease-specific health plan based on value-based health insurance benefit principles) on healthcare utilization among beneficiaries with household income ≤ $30,000 and found a negative association between DHP exposure and disease management visits but no relationship with emergency room or hospital utilization. Future studies are needed to determine if the associated reduction in disease management visits reflects improved diabetes management or reduced access to care.
References
Hill-Briggs, F. et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 44, 258–279 (2020).
Wild, S. H., McKnight, J. A., McConnachie, A. & Lindsay, R. S. Socioeconomic status and diabetes-related hospital admissions: a cross-sectional study of people with diagnosed diabetes. J Epidemiol Commun Health. 64, 1022–1024 (2010).
Tamblyn, R. et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 285, 421–429 (2001).
Miller, G. E., Sarpong, E. M. & Hill, S. C. Does increased adherence to medications change health care financial burdens for adults with diabetes? J Diabetes. 7, 872–880 (2015).
Pladevall, M. et al. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 27, 2800–2805 (2004).
Schectman, J. M., Nadkarni, M. M. & Voss, J. D. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care. 25, 1015–1021 (2002).
Shenolikar, R. A. & Balkrishnan, R. Oral antidiabetes medication adherence and health care utilization among Medicaid-enrolled type 2 diabetic patients beginning monotherapy. Diabetes Care. 31, e5–e5 (2008).
Choudhry, N. K. et al. Eliminating medication copayments reduces disparities in cardiovascular care. Health Affairs. 33, 863–870 (2014).
Roebuck, M. C., Liberman, J. N., Gemmill-Toyama, M. & Brennan, T. A. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Affairs. 30, 91–99 (2011).
Allen, K. & McFarland, M. How are income and education related to the prevention and management of diabetes? J Aging Health. 32, 1063–1074 (2020).
Vojta, D., De Sa, J., Prospect, T. & Stevens, S. Effective interventions for stemming the growing crisis of diabetes and prediabetes: a national payer’s perspective. Health Aff (Millwood). 31, 20–26 (2012).
Kimbro, L. B. et al. Optimizing enrollment in employer health programs: a comparison of enrollment strategies in the diabetes health plan. Am J Manag Care. 20, e311–e319 (2014).
Duru, O. K. et al. Adherence to metformin, statins, and ACE/ARBs within the Diabetes Health Plan (DHP). J Gen Intern Med. 30, 1645–1650 (2015).
Duru, O. K. et al. Evaluation of the diabetes health plan to improve diabetes care and prevention. Prev Chronic Dis. 10, E16 (2013).
Moin, T. et al. Association of the Diabetes Health Plan with emergency room and inpatient hospital utilization: a Natural Experiment for Translation in Diabetes (NEXT-D) Study. BMJ Open Diabetes Research and Care. 9, e001802 (2021).
Huang CX et al. Does the diabetes health plan have a differential impact on medication adherence among beneficiaries with fewer financial resources? J Manag Care Spec Pharm. 2022. https://doi.org/10.21203/rs.3.rs-521335/v1.
Narain, K. D. C. et al. The diabetes health plan and medication adherence among individuals with low incomes. Health Services Res. n/a.
Wonderman Data Products. AmeriLINK. Wunderman Data Products https://www.kbmg.com/products/amerilink/.
Guo, S. Y. & Fraser, M. W. Propensity score analysis: statistical methods and applications. (SAGE Publications, Inc, 2009).
Tukey, J. Exploratory data analysis. (Pearson, 2019).
Zhou, H., Taber, C., Arcona, S. & Li, Y. Difference-in-differences method in comparative effectiveness research: utility with unbalanced groups. Appl Health Econ Health Policy. 14, 419–429 (2016).
Stuart, E. A. et al. Using propensity scores in difference-in-differences models to estimate the effects of a policy change. Health Serv Outcomes Res Methodol. 14, 166–182 (2014).
Fraze, T., Jiang, H. J. & Burgess, J. Hospital Stays for Patients with Diabetes, 2008: Statistical Brief #93. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs (Agency for Healthcare Research and Quality (US), 2006).
Tabano, D. C. et al. Estimating the impact of diabetes mellitus on worker productivity using self-report, electronic health record and human resource data. J Occup Environ Med 60, e569 (2018).
Acknowledgements
The authors acknowledge Dr. Sam Ho for the content expertise provided regarding the Diabetes Health Plan and other UnitedHealthCare insurance products.
Funding
This research was supported by the Centers for Disease Control and Prevention (CDC) Grant Number U18DP006128-01 and National Institute on Aging Grant Number K08AG068372-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations:
None
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Narain, K.D.C., Turk, N., Duru, O.K. et al. The Diabetes Health Plan and Healthcare Utilization Among Beneficiaries with Low Incomes. J GEN INTERN MED 38, 1672–1680 (2023). https://doi.org/10.1007/s11606-022-07903-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07903-9