Abstract
BACKGROUND
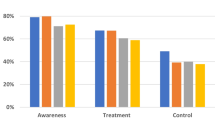
Rates of blood pressure (BP) control are lower in minority populations compared to whites.
OBJECTIVE
As part of a project to decrease health-related disparities among ethnic groups, we sought to evaluate the knowledge, attitudes, and management practices of clinicians caring for hypertensive patients in a predominantly minority community.
DESIGN/PARTICIPANTS
We developed clinical vignettes of hypertensive patients that varied by comorbidity (type II diabetes mellitus, chronic renal insufficiency, coronary artery disease, or isolated systolic hypertension alone). We randomly assigned patient characteristics, e.g., gender, age, race/ethnicity, to each vignette. We surveyed clinicians in ambulatory clinics of the 4 hospitals in East/Central Harlem, NY.
MEASUREMENTS
The analysis used national guidelines to assess the appropriateness of clinicians’ stated target BP levels. We also assessed clinicians’ attitudes about the likelihood of each patient to achieve adequate BP control, adhere to medications, and return for follow-up.
RESULTS
Clinicians’ target BPs were within 2 mm Hg of the recommendations 9% of the time for renal disease patients, 86% for diabetes, 94% for isolated systolic hypertension, and 99% for coronary disease. BP targets did not vary by patient or clinician characteristics. Clinicians rated African-American patients 8.4% (p = .004) less likely and non-English speaking Hispanic patients 8.1% (p = .051) less likely than white patients to achieve/maintain BP control.
CONCLUSIONS
Clinicians demonstrated adequate knowledge of recommended BP targets, except for patients with renal disease. Clinicians did not vary management by patients’ sociodemographics but thought African-American, non-English-speaking Hispanic and unemployed patients were less likely to achieve BP control than their white counterparts.

Similar content being viewed by others
References
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206.
Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey 1988–1991. Hypertension. 1995;25:305–13.
Chobian AV, Bakris GL, Black HR, et al. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII). JAMA. 2003;289:2560–72.
JNC 6. National High Blood Pressure Education Program. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–46.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Stamler J. End-stage renal disease in African-American and white men. 16-year MRFIT findings. JAMA. 1997;277:1293–8.
Stockwell DH, Madhavan S, Cohen H, Gibson G, Alderman MH. The determinants of hypertension awareness, treatment, and control in an insured population. Am J Public Health. 1994;84:1768–74.
Ahluwalia JS, McNagny SE, Rask KJ. Correlates of controlled hypertension in indigent, inner-city hypertensive patients. J Gen Intern Med. 1997;12:7–14.
Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med. 2000;160:2281–6.
Hyman DJ, Pavlik VN, Vallbona C. Physician role in lack of awareness and control of hypertension. J Clin Hypertens. 2000;2:324–30.
Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The fifth report of the Joint National Committee on detection, evaluation, and treatment of high blood pressure (JNC V). Arch Intern Med. 1993;153:154–83.
Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–63.
Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–20.
Van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(Suppl 1):I-140–51.
Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26.
Schwartz LM, Woloshin S, Welch HG. Misunderstandings about the effects of race and sex on physicians’ referrals for cardiac catheterization. N Engl J Med. 1999;341:279–83.
Van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–28.
Green BB, Kaplan RC, Psaty BM. How do minor changes in the definition of blood pressure control affect the reported success of hypertension treatment? Am J Manag Care. 2003;9:219–24.
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker or diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–97.
Swanson DB, Barrow HS, Friedman CP. Issues in assessment of clinical competence. Prof Educ Res. 1982;4:2.
Moskowitz AJ, Kuipers B, Kassirer JP. Dealing with uncetainty, risks, and trade offs in clinical decisions: a cognitive science approach. Ann Intern Med. 1988;108:435–49.
Jones TV, Gerrity MS, Earp J. Written case simulations: do they predict physicians’ behavior? J Clin Epidemiol. 1990;43:805–15.
Kirwan JR, Chaput de Saintonge DM, Joyce CRB, Currey HLF. Clinical judgement in rheumatoid arthritis. I. Rheumatologists’ opinions and the development of “paper patients.” Ann Rheum Dis. 1983;42:644–7.
Kirwan JR, Bellamy N, Condon H, Buchanan WW, Barnes CG. Judging “current disease activity” in rheumatoid arthritis—an international comparison. J Rheumatol 1983;10:901–5.
U.S. Centers for Disease Control and Prevention. National diabetes fact sheet. http://www.cdc.gov/diabetes/pubs/estimates.htm, accessed September 2, 2005.
Acknowledgements
This work was presented in abstract form at The Society of General Internal Medicine 26th Annual Meeting, April 30 to May 3, 2003, in Vancouver, British Columbia, and at the Academy Health Annual Research Meeting, June 27–29, 2003, in Nashville, TN.
Funding Source
Agency for Healthcare Research and Quality, P01 HS10859; National Center for Minority Health and Health Disparities, National Institutes of Health, P60 MD00270-01; and The Commonwealth Fund, 20030088.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This research project has not been published in any other peer-reviewed media and is not under review elsewhere. This study was conducted at the Mount Sinai School of Medicine, New York. All of the authors listed on the manuscript have contributed sufficiently to the project to be included as authors.
Rights and permissions
About this article
Cite this article
Goldstein, C.E., Hebert, P.L., Sisk, J.E. et al. Hypertension Management in Minority Communities: A Clinician Survey. J GEN INTERN MED 23, 81–86 (2008). https://doi.org/10.1007/s11606-007-0413-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0413-z