Abstract
Background
Physical exercise prehabilitation has been proposed to improve postoperative outcomes in patients undergoing major abdominal surgery. The aim of this systematic review was to investigate the effect of preoperative exercise training compared with standard care on postoperative outcomes in major abdominal surgery.
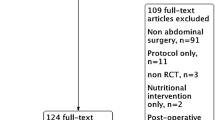
Methods
Randomized controlled trials (RCT) comparing prehabilitation with standard care were identified by a systematic literature search of MEDLINE and CENTRAL. Qualitative and quantitative analyses of perioperative outcome data were conducted. Meta-analyses were performed wherever possible and meaningful.
Results
A total of eight trials including 442 patients met the inclusion criteria. These trials investigated the effect of prehabilitation in patient cohorts undergoing major liver, colorectal, gastroesophageal, and general abdominal surgery. Quantitative analyses of all included trials showed a significant reduction in postoperative pulmonary complications (OR 0.37; 0.20 to 0.67; p = 0.001) as well as in postoperative overall morbidity (OR 0.52; 0.30 to 0.88; p = 0.01) in the prehabilitation group compared with standard care. The length of hospital stay showed no significant differences between the groups (MD − 0.58; − 1.28 to 0.13; p = 0.11). Risk of bias and methodological quality varied substantially among the trials, most of which were small single-center studies.
Conclusion
Prehabilitation including a physical exercise intervention may lead to a reduction of postoperative pulmonary complications as well as less overall morbidity compared with standard care in patients undergoing major abdominal surgery. Further, well-designed RCT are needed to evaluate these potential positive effects in more detail and to identify suitable target populations.
Protocol Registration
PROSPERO 2017 CRD42017080366





Similar content being viewed by others
References
Straatman, J., et al., Predictive Value of C-Reactive Protein for Major Complications after Major Abdominal Surgery: A Systematic Review and Pooled-Analysis. PLoS One, 2015. 10(7): p. e0132995.
Cunningham, D., et al., Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med, 2006. 355(1): p. 11-20.
Ychou, M., et al., Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol, 2011. 29(13): p. 1715-21.
Mariette, C., et al., Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer. N Engl J Med, 2019. 380(2): p. 152-162.
Smith, P.R., et al., Postoperative pulmonary complications after laparotomy. Respiration, 2010. 80(4): p. 269-74.
Visioni, A., et al., Enhanced Recovery After Surgery for Noncolorectal Surgery?: A Systematic Review and Meta-analysis of Major Abdominal Surgery. Ann Surg, 2018. 267(1): p. 57-65.
Carli, F. and C. Scheede-Bergdahl, Prehabilitation to enhance perioperative care. Anesthesiol Clin, 2015. 33(1): p. 17-33.
Wynter-Blyth, V. and K. Moorthy, Prehabilitation: preparing patients for surgery. BMJ, 2017. 358: p. j3702.
Singh, F., et al., A systematic review of pre-surgical exercise intervention studies with cancer patients. Surg Oncol, 2013. 22(2): p. 92-104.
Moyer, R., et al., The Value of Preoperative Exercise and Education for Patients Undergoing Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev, 2017. 5(12): p. e2.
Carli, F., et al., Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg, 2010. 97(8): p. 1187-97.
Soares, S.M., et al., Pulmonary function and physical performance outcomes with preoperative physical therapy in upper abdominal surgery: a randomized controlled trial. Clin Rehabil, 2013. 27(7): p. 616-27.
Gillis, C., et al., Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology, 2014. 121(5): p. 937-47.
Barberan-Garcia, A., et al., Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann Surg, 2018. 267(1): p. 50-56.
Boden, I., et al., Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ, 2018. 360: p. j5916.
Parikh, M., et al., Does a preoperative medically supervised weight loss program improve bariatric surgery outcomes? A pilot randomized study. Surg Endosc, 2012. 26(3): p. 853-61.
Moran, J., et al., The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: A systematic review and meta-analysis. Surgery, 2016. 160(5): p. 1189-1201.
Bruns, E.R., et al., The effects of physical prehabilitation in elderly patients undergoing colorectal surgery: a systematic review. Colorectal Dis, 2016. 18(8): p. O267-77.
Luther, A., et al., The Impact of Total Body Prehabilitation on Post-Operative Outcomes After Major Abdominal Surgery: A Systematic Review. World J Surg, 2018. 42(9): p. 2781-2791.
Treanor, C., T. Kyaw, and M. Donnelly, An international review and meta-analysis of prehabilitation compared to usual care for cancer patients. J Cancer Surviv, 2018. 12(1): p. 64-73.
Panic, N., et al., Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS One, 2013. 8(12): p. e83138.
Goossen, K., et al., Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg, 2018. 403(1): p. 119-129.
Higgins, J.P., et al., The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 2011. 343: p. d5928.
Hozo, S.P., B. Djulbegovic, and I. Hozo, Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol, 2005. 5: p. 13.
Dronkers, J.J., et al., Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil, 2010. 24(7): p. 614-22.
Dunne, D.F., et al., Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg, 2016. 103(5): p. 504-12.
Gillis, C., et al., Prehabilitation with Whey Protein Supplementation on Perioperative Functional Exercise Capacity in Patients Undergoing Colorectal Resection for Cancer: A Pilot Double-Blinded Randomized Placebo-Controlled Trial. J Acad Nutr Diet, 2016. 116(5): p. 802-12.
Kaibori, M., et al., Perioperative exercise for chronic liver injury patients with hepatocellular carcinoma undergoing hepatectomy. Am J Surg, 2013. 206(2): p. 202-9.
Yamana, I., et al., Randomized Controlled Study to Evaluate the Efficacy of a Preoperative Respiratory Rehabilitation Program to Prevent Postoperative Pulmonary Complications after Esophagectomy. Dig Surg, 2015. 32(5): p. 331-7.
Kim, D.J., et al., Responsive measures to prehabilitation in patients undergoing bowel resection surgery. Tohoku J Exp Med, 2009. 217(2): p. 109-15.
Dindo, D., N. Demartines, and P.A. Clavien, Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004. 240(2): p. 205-13.
Probst, P., et al., Blinding in randomized controlled trials in general and abdominal surgery: protocol for a systematic review and empirical study. Syst Rev, 2016. 5: p. 48.
Zingg, U., et al., Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann Surg Oncol, 2011. 18(5): p. 1460-8.
Barbalho-Moulim, M.C., et al., Effects of preoperative inspiratory muscle training in obese women undergoing open bariatric surgery: respiratory muscle strength, lung volumes, and diaphragmatic excursion. Clinics (Sao Paulo), 2011. 66(10): p. 1721-7.
Limongi, V., et al., Effects of a respiratory physiotherapeutic program in liver transplantation candidates. Transplant Proc, 2014. 46(6): p. 1775-7.
Lingsma, H.F., et al., Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res, 2018. 18(1): p. 116.
Fiore, J.F., Jr., et al., Time to readiness for discharge is a valid and reliable measure of short-term recovery after colorectal surgery. World J Surg, 2013. 37(12): p. 2927-34.
Curtis, N.J., et al., Time from colorectal cancer diagnosis to laparoscopic curative surgery-is there a safe window for prehabilitation? Int J Colorectal Dis, 2018. 33(7): p. 979-983.
Kulkarni, S.R., et al., Pre-operative inspiratory muscle training preserves postoperative inspiratory muscle strength following major abdominal surgery - a randomised pilot study. Ann R Coll Surg Engl, 2010. 92(8): p. 700-7.
Bond, D.S., et al., Bari-Active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis, 2015. 11(1): p. 169-77.
Baillot, A., et al., Impacts of Supervised Exercise Training in Addition to Interdisciplinary Lifestyle Management in Subjects Awaiting Bariatric Surgery: a Randomized Controlled Study. Obes Surg, 2016. 26(11): p. 2602-2610.
Llorens, J., et al., Preoperative inspiratory muscular training to prevent postoperative hypoxemia in morbidly obese patients undergoing laparoscopic bariatric surgery. A randomized clinical trial. Obes Surg, 2015. 25(6): p. 1003-9.
Haasenritter, J., et al., [Impact of a pre-operative mobilisation program using the Viv-Arte training model based on kinesthetic mobilisation on mobility, pain, and post-operation length of stay of patients receiving an elective medial laparotomy: a prospective, randomised, controlled pilot study]. Pflege, 2009. 22(1): p. 19-28.
Mayo, N.E., et al., Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery, 2011. 150(3): p. 505-14.
van Adrichem, E.J., et al., Comparison of two preoperative inspiratory muscle training programs to prevent pulmonary complications in patients undergoing esophagectomy: a randomized controlled pilot study. Ann Surg Oncol, 2014. 21(7): p. 2353-60.
Hijazi, Y., U. Gondal, and O. Aziz, A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg, 2017. 39: p. 156-162.
Bolshinsky, V., et al., Multimodal Prehabilitation Programs as a Bundle of Care in Gastrointestinal Cancer Surgery: A Systematic Review. Dis Colon Rectum, 2018. 61(1): p. 124-138.
Funding
The resources and facilities of the University of Heidelberg were used in conducting this study. No additional funding was applied for or received.
Author information
Authors and Affiliations
Contributions
PH and ALM developed the study concept. MKD, PP, JW, and KS helped to develop the study concept and gave methodological advice. PH and ALM carried out the literature search and data extraction. PH and ALM conducted statistical analyses. PH and ALM wrote the first draft of the manuscript. MKD, PP, JW, and KS provided scientific input for the study’s background and rationale and contributed to interpretation of the data. All authors read, critically revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
: Example of a search strategy for MEDLINE (via PubMed). (DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Heger, P., Probst, P., Wiskemann, J. et al. A Systematic Review and Meta-analysis of Physical Exercise Prehabilitation in Major Abdominal Surgery (PROSPERO 2017 CRD42017080366). J Gastrointest Surg 24, 1375–1385 (2020). https://doi.org/10.1007/s11605-019-04287-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04287-w