Abstract
Background
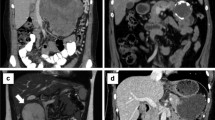
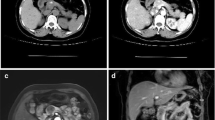
Solid pseudopapillary tumors (SPTs) are rare, benign tumors of the pancreas that present as heterogeneous masses. We sought to evaluate the short- and long-term outcomes of surgical resected SPTs. Patients managed via initial surveillance were compared to those who underwent upfront resection.
Methods
A prospectively maintained institutional database was used to identify patients who underwent surgical resection for a SPT between 1988 and 2018. Data on clinicopathological features and outcomes were collected and analyzed.
Results
Seventy-eight patients underwent surgical resection for SPT during the study period. The mean age was 34.0 ± 14.6 years and a majority were female (N = 67, 85.9%) and white (N = 46, 58.9%). Thirty patients (37.9%) were diagnosed incidentally. Imaging-based presumed diagnosis was SPT in 49 patients (62.8%). A majority were located in the body or tail of the pancreas (N = 47, 60.3%), and 48 patients (61.5%) underwent a distal pancreatectomy. The median tumor size was 4.0 cm (IQR, 3.0–6.0), nodal disease was present in three patients (3.9%), and R0 resection was performed in all patients. No difference was observed in clinicopathological features and outcomes between patients who were initially managed via surveillance and those who underwent upfront resection. None of the patients under surveillance had nodal disease or metastasis at the time of resection; however, one of them developed recurrence of disease 95.1 months after resection. At a median follow-up of 36.1 months (IQR, 8.1–62.1), 77 (%) patients were alive and one patient (1.3%) had a recurrence of disease at 95.1 months after resection and subsequently died due to disease.
Conclusions
SPTs are rare pancreatic tumors that are diagnosed most frequently in young females. While a majority are benign and have an indolent course, malignant behavior has been observed. Surgical resection can result in exceptional outcomes.



Similar content being viewed by others
References
Martin RC, Klimstra DS, Brennan MF, Conlon KC. Solid-pseudopapillary tumor of the pancreas: a surgical enigma? Ann Surg Oncol 2002; 9: 35–40.
Frantz V. Tumors of the Pancreas. Atlas of Tumor Pathology 1959; 2.
Hruban RH. Solid Pseudopapillary tumors of the pancreas. 2007.
Kloppel. Histological typing of tumors of the exocrine pancreas. 1996.
Kawamoto S, Scudiere J, Hruban RH et al. Solid-pseudopapillary neoplasm of the pancreas: spectrum of findings on multidetector CT. Clin Imaging 2011; 35: 21–28.
Reddy S, Cameron JL, Scudiere J et al. Surgical management of solid-pseudopapillary neoplasms of the pancreas (Franz or Hamoudi tumors): a large single-institutional series. J Am Coll Surg 2009; 208: 950–957; discussion 957-959.
Zheng X, Tan X, Wu B. [CT imaging features and their correlation with pathological findings of solid pseudopapillary tumor of pancreas]. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 2014; 31: 107–112.
Guo N, Zhou QB, Chen RF et al. Diagnosis and surgical treatment of solid pseudopapillary neoplasm of the pancreas: analysis of 24 cases. Can J Surg 2011; 54: 368–374.
Ng KH, Tan PH, Thng CH, Ooi LL. Solid pseudopapillary tumour of the pancreas. ANZ J Surg 2003; 73: 410–415.
Machado MC, Machado MA, Bacchella T et al. Solid pseudopapillary neoplasm of the pancreas: distinct patterns of onset, diagnosis, and prognosis for male versus female patients. Surgery 2008; 143: 29–34.
Mao C, Guvendi M, Domenico DR et al. Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world’s literature. Surgery 1995; 118: 821–828.
Sanfey H, Mendelsohn G, Cameron JL. Solid and papillary neoplasm of the pancreas. A potentially curable surgical lesion. Ann Surg 1983; 197: 272–275.
Zinner MJ, Shurbaji MS, Cameron JL. Solid and papillary epithelial neoplasms of the pancreas. Surgery 1990; 108: 475–480.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213.
Law JK, Ahmed A, Singh VK et al. A systematic review of solid-pseudopapillary neoplasms: are these rare lesions? Pancreas 2014; 43: 331–337.
Khashab MA, Kim K, Lennon AM et al. Should we do EUS/FNA on patients with pancreatic cysts? The incremental diagnostic yield of EUS over CT/MRI for prediction of cystic neoplasms. Pancreas 2013; 42: 717–721.
Law JK, Stoita A, Wever W et al. Endoscopic ultrasound-guided fine needle aspiration improves the pre-operative diagnostic yield of solid-pseudopapillary neoplasm of the pancreas: an international multicenter case series (with video). Surg Endosc 2014; 28: 2592–2598.
Bender AM, Thompson ED, Hackam DJ et al. Solid Pseudopapillary Neoplasm of the Pancreas in a Young Pediatric Patient: A Case Report and Systematic Review of the Literature. Pancreas 2018; 47: 1364–1368.
Cai YQ, Xie SM, Ran X et al. Solid pseudopapillary tumor of the pancreas in male patients: report of 16 cases. World J Gastroenterol 2014; 20: 6939–6945.
Lee SE, Jang JY, Hwang DW et al. Clinical features and outcome of solid pseudopapillary neoplasm: differences between adults and children. Arch Surg 2008; 143: 1218–1221.
Lanke G, Ali FS, Lee JH. Clinical update on the management of pseudopapillary tumor of pancreas. World J Gastrointest Endosc 2018; 10: 145–155.
Wolfgang CL, Herman JM, Laheru DA et al. Recent progress in pancreatic cancer. CA Cancer J Clin 2013; 63: 318–348.
Abraham SC, Klimstra DS, Wilentz RE et al. Solid-pseudopapillary tumors of the pancreas are genetically distinct from pancreatic ductal adenocarcinomas and almost always harbor beta-catenin mutations. Am J Pathol 2002; 160: 1361–1369.
Tanaka Y, Kato K, Notohara K et al. Frequent beta-catenin mutation and cytoplasmic/nuclear accumulation in pancreatic solid-pseudopapillary neoplasm. Cancer Res 2001; 61: 8401–8404.
Zhang Y, Han X, Wu H, Zhou Y. Bioinformatics analysis of transcription profiling of solid pseudopapillary neoplasm of the pancreas. Mol Med Rep 2017; 16: 1635–1642.
Amato E, Mafficini A, Hirabayashi K et al. Molecular alterations associated with metastases of solid pseudopapillary neoplasms of the pancreas. J Pathol 2018.
Serra S, Chetty R. Revision 2: an immunohistochemical approach and evaluation of solid pseudopapillary tumour of the pancreas. J Clin Pathol 2008; 61: 1153–1159.
Kim EK, Jang M, Park M, Kim H. LEF1, TFE3, and AR are putative diagnostic markers of solid pseudopapillary neoplasms. Oncotarget 2017; 8: 93404–93413.
Jutric Z, Rozenfeld Y, Grendar J et al. Analysis of 340 Patients with Solid Pseudopapillary Tumors of the Pancreas: A Closer Look at Patients with Metastatic Disease. Ann Surg Oncol 2017; 24: 2015–2022.
Serrano PE, Serra S, Al-Ali H et al. Risk factors associated with recurrence in patients with solid pseudopapillary tumors of the pancreas. JOP 2014; 15: 561–568.
Tajima H, Takamura H, Kitagawa H et al. Multiple liver metastases of pancreatic solid pseudopapillary tumor treated with resection following chemotherapy and transcatheter arterial embolization: A case report. Oncol Lett 2015; 9: 1733–1738.
El Nakeeb A, Abdel Wahab M, Elkashef WF et al. Solid pseudopapillary tumour of the pancreas: Incidence, prognosis and outcome of surgery (single center experience). Int J Surg 2013; 11: 447–457.
Fried P, Cooper J, Balthazar E et al. A role for radiotherapy in the treatment of solid and papillary neoplasms of the pancreas. Cancer 1985; 56: 2783–2785.
Maffuz A, Bustamante Fde T, Silva JA, Torres-Vargas S. Preoperative gemcitabine for unresectable, solid pseudopapillary tumour of the pancreas. Lancet Oncol 2005; 6: 185–186.
D'Haese JG, Werner J. Surgery of Cystic Tumors of the Pancreas - Why, When, and How? Visc Med 2018; 34: 206–210.
You L, Yang F, Fu DL. Prediction of malignancy and adverse outcome of solid pseudopapillary tumor of the pancreas. World J Gastrointest Oncol 2018; 10: 184–193.
Kang CM, Choi SH, Kim SC et al. Predicting recurrence of pancreatic solid pseudopapillary tumors after surgical resection: a multicenter analysis in Korea. Ann Surg 2014; 260: 348–355.
Nishihara K, Nagoshi M, Tsuneyoshi M et al. Papillary cystic tumors of the pancreas. Assessment of their malignant potential. Cancer 1993; 71: 82–92.
Rastogi A, Assing M, Taggart M et al. Does Computed Tomography Have the Ability to Differentiate Aggressive From Nonaggressive Solid Pseudopapillary Neoplasm? J Comput Assist Tomogr 2018; 42: 405–411.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the conception of the study. AAJ, MJWr, TS, and YZ preformed data collection and composed the first draft of the manuscript. RAB, JU, JH, JLC, MAM, CLW, and MJWe critically reviewed and edited the final draft of the manuscript. All the authors take responsibility for the accuracy of the repotted data.
Corresponding author
Ethics declarations
The study was approved by the Institutional Review Board for Human Research and complied with all Health Insurance Portability and Accountability Act regulations.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wright, M.J., Javed, A.A., Saunders, T. et al. Surgical Resection of 78 Pancreatic Solid Pseudopapillary Tumors: a 30-Year Single Institutional Experience. J Gastrointest Surg 24, 874–881 (2020). https://doi.org/10.1007/s11605-019-04252-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04252-7