Abstract
Background
Hepatic parenchymal transection is the most invasive step in donor operation. During this step, blood loss and unintended injuries to the intrahepatic structures and hepatic remnant may occur. There is no evidence to prove the ideal techniques for hepatic parenchymal transection. The aim of this study is to compare the safety, efficacy, and outcome of clamp-crush technique versus harmonic scalpel as a method of parenchymal transection in living-donor hepatectomy.
Methods
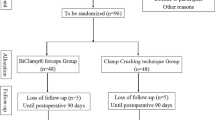
Consecutive living liver donors, undergoing right hemi-hepatectomy, during the period between May 2015 and April 2016, were included in this prospective randomized study. Cases were randomized into two groups; group (A) harmonic scalpel group and group (B) Clamp-crush group.
Results
During the study period, 72 cases underwent right hemi-hepatectomy for adult living donor liver transplantation and were randomized into two groups. There were no statistically significant differences between the two groups regarding preoperative demographic and radiological data. Longer operation time and hepatectomy duration were found in group B. There were no significant differences between the two groups regarding blood loss, blood loss during hepatectomy, and blood transfusion. More unexpected bleeding events occurred in group A. Higher necrosis at the cut margin of the liver parenchyma was noted in group A. There were no statistically significant differences between the two groups regarding postoperative ICU stay, hospital stay, postoperative morbidities, and readmission rates.
Conclusion
Clamp-crush technique is advocated as a simple, easy, safe, and cheaper method for hepatic parenchymal transection in living donors.


Similar content being viewed by others
References
Maluf DG, Stravitz RT, Cotterall AH, et al. Adult living donor versus deceased donor liver transplantation: a 6-year single center experience. American Journal of Transplantation 2005;5:149–156.
Rahbari NN, Koch M, Schmidt T, et al. Meta-analysis of the clamp-crushing technique for transection of the parenchyma in elective hepatic resection: back to where we started? Annals of Surgical Oncology 2009;16(3):630–639.
Smyrniotis V, Arkadopoulos N, Kostopanagiotou G, et al. Sharp liver transection versus clamp crushing technique in liver resections: a prospective study. Surgery 2005;137(3):306–11.
Kaibori M, Matsui K, Ishizaki M, et al. A prospective randomized controlled trial of hemostasis with a bipolar sealer during hepatic transection for liver resection. Surgery 2013;154(5):1046–52.
Jagannath P, Chhabra DG, Sutariya KR, Shah RC. Fusion technique for liver transection with Kelly-clysis and harmonic technology. World Journal of Surgery 2010;34(1):101–5.
Poon RT. Current techniques of liver transection. HPB (Oxford) 2007;9(3):166–173.
El Moghazy WM, Hedaya MS, Kaido T, Egawa H, Uemoto S, Takada Y. Two different methods for donor hepatic transection: cavitron ultrasonic surgical aspirator with bipolar cautery versus cavitron ultrasonic surgical aspirator with radiofrequency coagulator-A randomized controlled trial. Liver Transplantation 2009;15(1):102–5.
Takatsuki M, Eguchi S, Yamanouchi K, et al. Two-surgeon technique using saline-linked electric cautery and ultrasonic surgical aspirator in living donor hepatectomy: its safety and efficacy. American Journal of Surgery 2009;197(2):e25–7.
Salah T, Sultan MA, Fathy MO, Elshobary MM, Elghawalby AN, Sultan A, et al. Outcome of Right Hepatectomy for Living Liver Donors: A Single Egyptian Center Experience. Journal of Gastrointestinal Surgery 2012;16:1181–1188.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery 2004;240(2):205–213.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery. Surgery 2011;149(5):680–688.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011;149(5):713–724.
Marcos A, Fisher RA, Ham JM, et al. Right lobe living donor liver transplantation. Transplantation 1999;68(6):798–803.
Khalaf H, El-Meteini M, El-Sefi T, et al. Evolution of living donor liver transplantation in Egypt. Saudi Medical Journal 2005;26(9): 1394–1397.
Chan SC, Fan ST, Lo CM, et al. Effect of side and size of graft on surgical outcomes of adult-to-adult live donor liver transplantation. Liver Transplantation 2007;13(1):91–98.
Yi NJ, Suh KS, Cho JY, et al. Three-quarters of right liver donors experienced postoperative complications. Liver Transplantation 2007;13(6):797–806.
Kaneko H, Otsuka Y, Takagi S, Tsuchiya M, Tamura A, Shiba T. Hepatic resection using stapling devices. American Journal of Surgery 2004;187(2):280–4.
Nagano Y, Matsuo K, Kunisaki C, et al. Practical usefulness of ultrasonic surgical aspirator with argon beam coagulation for hepatic parenchymal transection. World Journal of Surgery 2005;29(7):899–902.
Romano F, Franciosi C, Caprotti R, Uggeri F, Uggeri F. Hepatic surgery using the Ligasure vessel sealing system. World Journal of Surgery 2005;29(1):110–112.
Gurusamy KS, Pamecha V, Sharma D, Davidson BR. Techniques for liver parenchymal transection in liver resection. Cochrane Database of Systematic Reviews 2009;(1):CD006880. https://doi.org/10.1002/14651858.CD006880.pub2.
Schmidbauer S, Hallfeldt KK, Sitzmann G, Kantelhardt T, Trupka A. Experience with ultrasound scissors and blades (UltraCision) in open and laparoscopic liver resection. Annals of Surgery 2002;235:27–30.
Hanyong S, Wanyee L, Siyuan F, et al. A prospective randomized controlled trial: comparison of two different methods of hepatectomy. European Journal of Surgical Oncology. 2015;41(2):243–248.
Rahbari NN, Elbers H, Koch M, et al. Clamp-crushing versus stapler hepatectomy for transection of the parenchyma in elective hepatic resection (CRUNSH)–a randomized controlled trial. BMC Surg 2011;11:22.
Lesuret M, Selzner M, Petrowsky H, McCormack L, Clavien PA. How should transection of liver be performed? A prospective randomized study in 100 consecutive patients: comparing four different transection strategies. Annals of Surgery 2005, 242:814–822.
Alexiou VG, Tsitsias T, Mavros MN, Robertson GS, Pawlik TM. Technology-assisted versus clamp-crush liver resection: a systematic review and meta-analysis. Surgical innovation 2013;20(4):414–428.
Takayama T, Makuuchi M, Kubota K, Harihara Y, Hui AM, Sano K, Ijichi M, Hasegawa K. Randomized comparison of ultrasonic vs clamp transection of the liver. Archives of surgery 2001;136(8):922–928.
Castaldo ET, Earl TM, Chari RS, et al. A clinical comparative analysis of crush/clamp, stapler, and dissecting sealer hepatic transection methods. HPB 2008;10(5):321–326.
Yuan Y, Gotoh M. Biliary complications in living liver donors. Surgery Today 2010;40:411–417.
Sultan AM, Salah T, Elshobary MM, Fathy OM, et al. Biliary complications in living donor right hepatectomy are affected by the method of bile duct division. Liver Transplantation 2014;20:1393–1401.
Barr ML, Belghiti J, Villamil FG, et al. A report of the Vancouver Forum on the care of the live organ donor: lung, liver, pancreas, and intestine data and medical guidelines. Transplantation 2006;81: 1373–85.
Gruttadauria S, Marsh JW, Vizzini GB, et al. Analysis of surgical and perioperative complications in seventy-five right hepatectomies for living donor liver transplantation. World Journal of Gastroenterology 2008;14:3159–3164.
Cho EH, Suh KS, Lee HW, Shin WY, Yi NJ, Lee KU. Safety of modified extended right hepatectomy in living liver donors. Transplantation International 2007;20:779–783.
Broering DC, Wilms C, Bok P, et al. Evolution of donor morbidity in living related liver transplantation. A single-center analysis of 165 cases. Annals of Surgery 2004;240:1013–1026.
Saiura A, Yamamoto J, Koga R, et al. Usefulness of Ligasure for liver resection: analysis by randomized clinical trial. American Journal of Surgery 2006,192:41–45.
Kim J, Ahmad SA, Lowy AM, Buell JF, et al. Increased biliary fistulas after liver resection with the harmonic scalpel. American Journal of Surgery 2003;69:815–9.
Bodzin AS, Leiby BE, Ramirez CG, Frank AM, Doria C. Liver resection using cavitron ultrasonic surgical aspirator (CUSA) versus harmonic scalpel: a retrospective cohort study. International Journal of Surgery 2014;12(5):500–503.
Rahbari NN, Elbers H, Koch M, et al. Randomized clinical trial of stapler versus clamp-crushing transection in elective liver resection. British Journal of Surgery 2014;101(3):200–207.
Author information
Authors and Affiliations
Contributions
The conception and design of the manuscript: Sultan AM, Shehta A.
The acquisition, analysis, or interpretation of data of the manuscript: Sultan AM, Shehta A, Monier A.
Drafting the manuscript or revising it critically for important intellectual content: all authors.
Final approval of the version of the manuscript to be published: all authors.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sultan, A.M., Shehta, A., Salah, T. et al. Clamp-Crush Technique Versus Harmonic Scalpel for Hepatic Parenchymal Transection in Living Donor Hepatectomy: a Randomized Controlled Trial. J Gastrointest Surg 23, 1568–1577 (2019). https://doi.org/10.1007/s11605-019-04103-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04103-5