Abstract
Background
Primary closure of post-operative facial dehiscence (FD) is associated with a high incidence of recurrence, revisional surgery, and incisional hernia. This retrospective study compares outcomes of implantation of non-absorbable intra-abdominal meshes with primary closure of FD. The outcomes of different mesh materials were assessed in subgroup analysis.
Methods
A total of 119 consecutive patients with FD were operated (70 mesh group and 49 no mesh group) between 2001 and 2015. Primary outcome parameter was hernia-free survival. Secondary outcome parameters include re-operations of the abdominal wall, intestinal fistula, surgical site infections (SSI), and mortality. Kaplan-Meier analysis for hernia-free survival, adjusted Poisson regression analysis for re-operations and adjusted regression analysis for chronic SSI was performed.
Results
Hernia-free survival was significantly higher in the mesh group compared to the no mesh group (P = 0.005). Fewer re-operations were necessary in the mesh group compared to the no mesh group (adjusted incidence risk ratio 0.44, 95% confidence interval [CI] 0.20–0.93, P = 0.032). No difference in SSI, intestinal fistula, and mortality was observed between groups. Chronic SSI was observed in 7 (10%) patients in the mesh group (n = 3 [6.7%] with polypropylene mesh and 4 [28.6%] with polyester mesh). The risk for chronic SSI was significantly higher if a polyester mesh was used when compared to a polypropylene mesh (adjusted odds ratio 8.69, 95% CI 1.30–58.05, P = 0.026).
Conclusion
Implantation of a polypropylene but not polyester-based mesh in patients with FD decreases incisional hernia with a low rate of mesh-related morbidity.
Similar content being viewed by others
Introduction
Fascial dehiscence (FD) is a surgical complication in which the fascia dissociates along the surgical incision and potentially leads to evisceration. The incidence ranges from 0.5 to 2.9% following abdominal surgery.1,2 Potential risk factors for FD include technical failure, elevated intra-abdominal pressure (e.g., in obese patients), and deep or superficial surgical site infection (SSI).3
Patients after FD are at high risk of re-rupture of the abdominal fascia following primary closure with an incidence of up to 44.4%.4 This recurrence might potentially end in an open abdomen requiring multiple revisional operations. Additionally, these patients are at exceedingly high risk of developing incisional hernia with an incidence of up to 83% of patients.5
Despite such high rates of complications, little evidence-based therapeutic or prophylactic options are currently available. Strategies to treat FD include (1) direct closure of the abdominal wall, (2) implantation of an absorbable mesh, and (3) implantation of a non-absorbable mesh. Because the first option is associated with a high incidence of recurrent FD and incisional hernia,4,6 implantation of meshes has been attempted to prevent recurrent FD.7 However, usage of absorbable meshes did not reduce incisional hernia in comparison to direct closure of the abdominal wall.8
Thus, only implantation of non-absorbable meshes potentially prevents both, early recurrence of FD and incisional hernia formation.6,9 Despite such theoretical advantages, prosthetic non-absorbable meshes are not commonly used mainly because of potential risks of mesh-related morbidity in a contaminated or dirty surgical field, which is typically found in patients with FD.10 Such restrictive use, however, is not based on solid scientific data beyond case reports. While some evidence exists showing safety in hernia surgery in the contaminated field, evidence is lacking of the use of non-absorbable meshes in FD.11,12 Such analysis is complicated by the plethora of meshes currently available. Mesh material potentially determines survival and clearance of bacteria as well as biofilm formation.13,14 In particular, multi-filamentous polyester meshes (PE) seem to be more prone to chronic SSI because of decreased bacterial resistance and clearance compared to polypropylene meshes (PP).15
This study is based on the hypothesis that non-absorbable meshes may reduce recurrent FD and incisional hernia. Thus, the aim of this single-center study was to compare the results of non-absorbable mesh implantation with conventional closure using a single running suture in patients with FD. The goal was to obtain a risk-benefit assessment of the potential treatment strategies in this severe clinical condition. In order to determine the relevance of mesh material, a subgroup analysis was performed to compare between PP and PE meshes.
Materials and Methods
Study Design
In this retrospective study, all medical records of patients treated for FD between January 2001 and December 2015 were screened. In total, 171 patients with FD were identified. Then, 52 patients were excluded because no primary fascial closure was achieved (laparostomy or open abdomen) resulting in 119 patients analyzed in the current study. This study has been approved by the ethics committee of Bern, Switzerland.
Patients who underwent intraperitoneal mesh implantation (mesh group) were compared to primary fascial closure (no mesh group). In 2006, intraperitoneal, non-absorbable mesh implantation became standard of care at the institution for the treatment of patients with FD because of the clinical observation of severe abdominal wall complications in patients with primary fascial closure (recurrent FD, hernia). Thus, assignment to groups was dependent on the year of treatment: 79.6% (39/49) of patients in the no mesh group were treated before 2006 and 20.4% (10/49) were treated after 2006. Reasons for no mesh treatment after 2006, thus deviation from standard of care (n = 10), were severe intra-abdominal contamination or underlying disease (supporting information, Table S1).
Primary outcome parameter was hernia-free survival. Follow-up was recorded at 3 months, 1 year, and 2 years in addition to the last follow-up. Hernia-free was defined as no occurrence of a clinically apparent hernia. Clinically apparent hernia was defined as (1) if an operation was performed because of hernia or (2) if clinically identified by an independent observer. Secondary outcome parameters comprised mesh-related morbidity such as intestinal fistula, SSI, partial mesh explantation, and re-operations. Different mesh materials (polypropylene (PP), polyester (PE)) were assessed in conjunction to mesh-related morbidity.
Post-surgical complications were classified according to Clavien-Dindo16 and SSI according to CDC.17 Chronic SSI was defined by clinical evidence of SSI lasting longer than 268 days, which represents the median duration of SSI in the mesh group. Intestinal (enterocutaneous) fistula was defined as cutaneous secretion of bowel contents after FD repair. Re-operations were defined as revisional surgeries under general anesthesia related to complications of the abdominal wall. Revisional surgeries included fistula takedown, revisional surgery because of SSI, incisional hernia, reconstruction of the abdominal wall, and partial or complete mesh explantation. Partial mesh explantation was defined as a surgical procedure removing parts of the mesh under general anesthesia. Anastomotic leakage was defined as a defect of the anastomotic site associated with a leak of intestinal contents. The Mannheim peritonitis index was assessed using the previously published weighting score.18 The grade of contamination and existing adhesions was assessed using the Björck classification.19
In addition to our own historical cohort (no mesh implantation), published series with and without non-absorbable mesh implantation were identified and important outcome parameter (incisional hernia, intestinal fistula, SSI, mesh explantation) were recorded and compared to the current results. The results were plotted with the outcome parameter on the Y-axis and duration of follow-up on the X-axis.
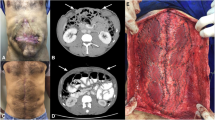
Surgical Technique
Patients with FD were taken to the operating room. First, the underlying pathology was explored and treated adhering to standards. The abdominal cavity was extensively rinsed with saline.
In the no mesh group, the abdominal fascia was primarily closed with a single running suture using loop 0-PDS (PDS®, Ethicon Sarl) in a standardized technique using a suture:wound ratio of 1:4. The skin was closed using loose single sutures or a vacuum dressing.
In the mesh group, a non-absorbable mesh was implanted intraperitoneally before fascial closure. The chosen mesh material (PP vs. PE) was at the discretion of the responsible surgeon. The meshes overlapped the incision by at least 5 cm on all sides. Any form of preperitoneal dissection has been avoided. The mesh was fixed using running 3–0 polypropylene sutures interrupted every 10 cm (Prolene®, Ethicon Sarl). The fascia was closed using a 0 PDS running suture (PDS®, Ethicon Sarl) in a standardized technique using a suture:wound ratio of 1:4. The skin was closed using loose single sutures or a vacuum dressing. The application of a vacuum dressing was at the discretion of the surgeon, e.g., if a SSI was highly likely to occur. The dressings were changed at an interval of 3–4 days. The vacuum dressings were removed when there was evidence of granulation tissue in addition to clean wound conditions.
Statistics
Data are reported as median and interquartile ranges (IQR), or numbers and percentages. The primary endpoint, hernia-free survival, was analyzed with Kaplan-Meier curves and a log-rank test for statistical comparison. Secondary outcomes were compared using Fisher’s exact test and Mann-Whitney U test for categorical and continuous variables respectively. Effects are reported as risk differences or c-statistics with 95% confidence intervals (CI). The effect of mesh treatment on hernia-free survival and secondary outcomes was further tested in a univariable and multivariable (adjusted) regression model. Clinically important variables (age, gender, BMI, smoker, malignancy, ASA score, immunosuppressive drugs, and type of laparotomy) were tested and included in the regression model. Co-variables with a P value below 0.2 on univariable analysis were included. Logistic, Cox, or Poisson regression were fitted for binary, time-to-event, or count outcomes, respectively. Results are reported as odds ratio (OR), hazard ratio (HR), or incidence risk ratio (IRR) with 95% CI and P values. Identified studies reporting synthetic mesh vs no mesh in patients with fascial dehiscence were summarized using the random effects model. All statistical tests were performed by using SPSS Statistics (Version 17.0.0, SPSS Inc., Chicago, IL). A two-sided P value of < 0.05 was considered statistically significant.
Results
Different meshes used in our patient cohorts were in 54 (77.1%) patients a large-pore, mono-filamentous, dual-layered PP mesh [in 50 (71.4%) patients Parietene Composite®, Medtronic, and in 4 (5.7%) patients Dynamesh®, FEG Textiltechnik mbH] and in 16 (22.9%) patients a large-pore, multi-filamentous, dual-layered PE mesh (Parietex Composite®, Medtronic).
Short-Term Outcome
Patient characteristics are shown in Table 1. Detailed operative characteristics are shown in Table 2. During surgery for FD, there was no difference in anastomotic leakage between the two groups. Post-operative results are shown in Table 3. There was no statistically significant difference in intestinal fistula and in-hospital mortality between the two groups. A significant decrease in complications above grade IIIa according to Clavien-Dindo was found if a mesh was implanted (P = 0.034) leading to an adjusted odds ratio (OR) of 0.46 (P = 0.067, Table 4).
Long-Term Outcome
SSI at last follow-up was observed in 12 (30.0%) patients in the no mesh group and in 10 (16.9%) patients in the mesh group (risk difference − 13.1, 95% CI − 30.2–4.1, P = 0.145) after a median follow-up of 281 days (IQR 69–770) in the no mesh group and 335 days (IQR 84–1304) in the mesh group (P = 0.441). Median rate of re-operations was significantly higher in the no mesh group compared to the mesh group (P < 0.001). The incidence of re-operations per 1000 person days was 0.88 (95% CI 0.57–1.31) in the no mesh group and 0.44 (95% CI 0.21–0.80) in the mesh group. Adjusted incidence risk ratio for re-operations (probability of re-operation per person time) for the mesh group vs no mesh group was 0.44 (95% CI 0.20–0.93, P = 0.032, Table 4). Incisional hernia was observed in 15 of 40 (37.5%) patients in the no mesh group and 8 of 59 (13.6%) patients in the mesh group (risk difference − 23.9, 95% CI − 41.3 to − 6.6, P = 0.008). Hernia-free survival showed a significantly different curve separation when comparing mesh vs no mesh (P = 0.005, Fig. 1). The site of hernia recurrence in the mesh group was mainly at the borders of the meshes (n = 2) or after mesh removal because of infectious complications in an intention to treat analysis (n = 2). Adjusted Cox regression analysis revealed non-absorbable mesh implantation as a significant protective factor for incisional hernia (HR 0.27, 95% CI 0.10–0.72, P = 0.008, Table 4).
Next, incidence of incisional hernia was compared to published series reporting outcomes with and without non-absorbable meshes in patients with FD (Fig. 2, Tables S2 and S3 (supporting information)).5,6,20,21,22 There is a linear increase (R2 = 0.923) in incidence of incisional hernia over time without mesh implantation. Pooled odds ratio for incisional hernia formation after mesh implantation was 0.27 (95% CI 0.09–0.76, P = 0.013) compared to no mesh (Supplementary fig. S1).6,20
Morbidity Related to Mesh Material
Overall, SSI at first follow-up was observed in 24 of 59 patients (40.7%). SSI at first follow-up was found in 16 of 45 (35.6%) patients if a PP mesh and in 8 of 14 (57.1%) patients if a PE mesh was implanted (risk difference − 21.5, 95% CI − 7.9–51.0, P = 0.214, Fig. 3). Overall, chronic SSI (duration > 268 days) was found in 7 of 59 (11.9%) patients after mesh implantation. Chronic SSI was found in 3 of 45 (6.7%) with PP mesh and in 4 of 14 (28.6%) with PE mesh. The incidence of chronic SSI with a PE mesh was significantly increased when compared to PP in unadjusted (OR 5.60, 95% CI 1.08–29.11, P = 0.040) and adjusted logistic regression analysis (OR 8.69, 95% CI 1.30–58.05, P = 0.026). Partial mesh removal was required in 2 of 45 (4.4%) PP meshes, and in 2 of 14 (14.3%) PE meshes (P = 0.236) (Table 5).
Median percentage of non-absorbable mesh explantation in published series is 4.5 (1.8–10.8) (Fig. 4).6,10,12,23,24,25
Discussion
In the current study, implantation of synthetic, non-absorbable, dual-layered PP mesh was associated with decreased incisional hernia and a low rate of mesh-related morbidity in patients with FD. An important observation is that PE meshes are associated with an increased risk of chronic SSI when compared to PP meshes.
Reported incidence of hernia in patients with FD without mesh implantation ranges from 25 to 83%. Regression analysis of published series addressing the rate of incisional hernia after FD show a linear increase in hernia incidence as shown in Fig. 2a (Supplementing material, Table S2).5,6,20,21,22 Such data highlight the importance of addressing abdominal wall reinforcement in this high risk population. The current study reveals that mesh implantation during repair for FD seems to be an effective therapeutic approach. Recurrence was mainly observed at the mesh borders, which underlines the importance of an adequate surgical technique aiming to sufficiently overlap the incision.
Putative disadvantages of mesh implantation include any type of SSI and intestinal fistula. The current study, however, shows that the incidence of these risks is not increased in patients after mesh implantation compared to controls without meshes from the same institution as well from published series.26,27 SSI after synthetic mesh implantation in contaminated abdominal cavity have been reported to occur in between 22.8 and 77% of patients (Supplementing material, Table S3).6,10,12,23,24,25 The wide variability in reported occurrence of SSI is the consequence of the heterogeneity because of varying inclusion criteria, mesh types, and localization. Exceptional high rates of wound complications of 77% with 17% of enterocutaneous fistulae seem to be the consequence of the use of non-dual-layered meshes.10 Such findings underline the relevance of visceral protection that are allowed in part by the use of dual-layered meshes. Thus, fistula formation and mesh explantation were very rare in the current series, which is consistent with other recent publications (Fig. 4).6,10,12,23,24,25
The present study reveals that not just visceral protection but also mesh material is of major importance for the success of intraperitoneal mesh implantation. Consistent with our data, Leber et al. already reported in 1998 that PE meshes are associated with a higher incidence of SSI, fistula formation, hernia recurrences, and overall complications compared to PP meshes.28 This observation is also supported by experimental data that show significant reduced numbers of colony forming units per gram tissue in PP meshes compared to PE meshes.15 This observation was made before the introduction of dual-layered meshes. The present study confirms these results with dual-layered PP that was superior to PE in contaminated abdomen with an OR of 8.69 for chronic SSI using PE-based meshes.
Biologic meshes are a potential alternative to synthetic meshes for the use in FD. However, a recent meta-analysis did not show a benefit for biologic meshes in terms of SSI or hernia recurrence in potentially contaminated hernias.29 Conversely, biologic mesh repair is associated with considerable higher rate of surgical site complications and hernia recurrence in contaminated hernia repairs compared to synthetic meshes.12,29 Therefore, the costs of biologic meshes in these settings most likely do not outweigh their benefit. Such hypothesis, however, needs clarification in a prospective controlled trial.
The limitation of this study is its retrospective design and the fact that a historic control was necessary. However, the most important outcome parameters (hernia, fistula, mortality) between groups did not change over the studied period compared to published analyses.5,6,20,21,22 Due to the fact that this is a retrospective study, unlike for symptomatic hernia, asymptomatic hernia might have been missed in our patient’ population. Additionally, the comparison to published series is limited by the quality of the included studies. Given the high rate of success with this approach a randomized trial would be difficult to be accepted by the treating surgeons. Therefore, larger multi-institutional cohorts may allow to further support the current findings.
Conclusion
The current study shows that implantation of a dual-layered PP but not dual-layered PE meshes in patients with FD decreases incisional hernia with a low rate of mesh-related morbidity.
References
Pavlidis TE, Galatianos IN, Papaziogas BT, Lazaridis CN, Atmatzidis KS, Makris JG, Papaziogas TB. Complete dehiscence of the abdominal wound and incriminating factors. Eur J Surg 2001;167:351–354.
Kenig J, Richter P, Lasek A, Zbierska K, Zurawska S. The efficacy of risk scores for predicting abdominal wound dehiscence: a case-controlled validation study. BMC Surg 2014;14:65.
Tillou A, Weng J, Alkousakis T, Velmahos G. Fascial dehiscence after trauma laparotomy: a sign of intraabdominal sepsis. Am Surg 2003;69: 927–929.
Abbott DE, Dumanian GA, Halverson AL. Management of laparotomy wound dehiscence. Am Surg 2007;73:1224–1227.
van Ramshorst GH, Eker HH, van der Voet JA, Jeekel J, Lange JF. Long-term outcome study in patients with abdominal wound dehiscence: a comparative study on quality of life, body image, and incisional hernia. J Gastrointestinal Surg 2013;17:1477–1484.
Petersson P, Montgomery A, Petersson U. Wound dehiscence: outcome comparison for sutured and mesh reconstructed patients. Hernia 2014;18:681–689.
Paye F, Rongère C, Gendreau D, Lenriot JP. Intraperitoneal resorbable mesh in the prevention of posoperative wound dehiscence. A comparative study. Ann Surg 1992;46:518–522.
Sarr MG, Hutcher NE, Snyder S, Hodde J, Carmody B. A prospective, randomized, multicenter trial of Surgisis Gold, a biologic prosthetic, as a sublay reinforcement of the fascial closure after open bariatric surgery. Surgery 2014;156:902–908.
Scholtes M, Kurmann A, Seiler CA, Candinas D, Beldi G. Intraperitoneal mesh implantation for fascial deshicence and open abdomen. World J Surg 2012;36:1557–1561.
van’t Riet M, de Vos van Steenwijk PJ, Bonjer HJ, Steyerberg EW, Jeekel J. Mesh repair for postoperative wound dehiscence in the presence of infection: is absorbable mesh safer than non-absorbable mesh? Hernia 2007;11:409–413.
Chamieh J, Tan WH, Ramirez R, Nohra E, Apakama C, Symons W. Synthetic versus biologic mesh in single-stage repair of complex abdominal wall defects in a contaminated field. Surg Infect 2017;18:112–118.
Majumder A, Winder JS, Wen Y, Pauli EM, Belyansky I, Novitsky YW. Comparative analysis of biologic versus synthetic mesh outcomes in contaminated hernia repairs. Surgery 2016;160:828–838.
Engelsman AF, van der Mei HC, Busscher HJ, Ploeg RJ. Morphological aspects of surgical meshes as a risk factors for bacterial colonization. Br J Surg 2008;95:1051–1059.
Deerenberg EB, Mulder IM, Grotenhuis N, Ditzel M, Jeekel J, Lange JF. Experimental study on synthetic and biological mesh implantation in a contaminated environment. Br J Surg 2012;99:1734–1741.
Majumder A, Petro CC, Liu L, Fayezizadeh M, Novitsky YW. Development of a novel murine model for treatment of infected mesh scenarios. Surg Endosc 2017;31:922–927.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–213.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 1992;13:606–608.
Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Grundlach E. The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis. Chirurg 1987;58:84–92.
Björck M, Bruhin A, Cheatham M, Hinck D, Kaplan M, Manca G, Wild T, Windsor A. Classification—important step to improve the management of patients with open abdomen. World J Surg 2009;33:1154–1157.
Lopez-Cano M, Pereira JA, Feliu X, Hernandez L, Andrada D, Gil E, Villaneuva B, Armengol-Carrasco M. Outcome of the use of a synthetic mesh in the repair of burst abdomen as compared with simple suture. Int J Clin Med 2015;6:113–118.
Gislason H, Viste A. Closure of burst abdomen after major gastrointestinal operations-comparison of different surgical techniques and later development of incisional hernia. Eur J Surg 1999;165:958–961.
Qassemyar Q, Browet F, Robbe M, Verhaeghe P, Regimbeau JM. Dynamic parietal closure: initial experience of an original parietal procedure for treatment of abdominal wound dehiscence. Arch Surg 2011;146:762–764.
Carbonell AM, Criss CN, Cobb WS, Novitsky YW, Rosen MJ. Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg 2013;217:991–998
Argudo N, Pereira JA, Sancho JJ, Membrilla E, Pons MJ, Grande L. Prophylactic synthetic mesh can be safely used to close emergency laparotomy, even in Peritonitis. Surgery 2014;156:1238–1244.
Lopez-Cano M, Quiles MT, Pereira JA, Armengol-Carrasco M, Arbos Via MA. Complex abdominal wall hernia repair in contaminated surgical fields: factors affecting the choice of prosthesis. Am Surg 2017;83:583–590.
Bhangu A, Singh P, Lundy J, Bowley DM. Systematic review and meta-analysis of randomized clinical trials comparing primary vs delayed primary skin closure in contaminated and dirty incisions. JAMA Surg 2013;148:779–786.
Hernandez K, Ramos E, Seas C, Henostroza G, Gotuzzo E. Incidence of and risk facots for surgical-site infections in a Peruvian hospital. Infect Control Hosp Epidemiol 2005;26:473–477.
Leber GE, Garb JL, Alexander AI, Reed WP. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 1998;133:378–382.
Atema JJ, de Vries FE, Boermeester MA. Systematic review and meta-analysis of the repair of potentially contaminated and contaminated abdominal wall defects. Am J Surg 2016;212:982–995.
Author information
Authors and Affiliations
Contributions
Manuel Jakob: study design, acquiring data, data analysis, and drafting article. Daniel Spari: acquiring data and drafting article. Joel Zindel: statistical analysis and critical revision of article. Tawan Pinworasarn: acquiring data and data analysis. Daniel Candinas: study design and critical revision of article. Guido Beldi: study design, data analysis, and critical revision of article.
Corresponding author
Ethics declarations
This study has been approved by the ethics committee of Bern, Switzerland.
Additional information
This work was presented to the European hernia congress (EHS), Vienna, Austria, May 2017.
Electronic Supplementary Material
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jakob, M.O., Spari, D., Zindel, J. et al. Prophylactic, Synthetic Intraperitoneal Mesh Versus No Mesh Implantation in Patients with Fascial Dehiscence. J Gastrointest Surg 22, 2158–2166 (2018). https://doi.org/10.1007/s11605-018-3873-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3873-z