Abstract
Purpose
The impact of preoperative sarcopenia on postoperative complications and overall survival has been recently debated. Our meta-analysis aims to ascertain whether preoperative sarcopenia increases the risk of poor outcomes and to attempt to provide new ideas for the prognosis of outcomes for patients with gastric cancer.
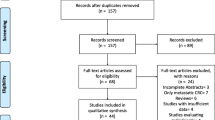
Methods
We searched for all relevant articles on PubMed, the EMBASE database, and Web of Science (up to September 1, 2017). Data synthesis and statistical analysis were carried out using RevMan 5.3 software.
Results
Thirteen studies involving 4262 patients who underwent gastrectomy for gastric cancer were analyzed (sarcopenia group = 1234; non-sarcopenia group = 3028). The results showed that preoperative sarcopenia significantly associated with poor pathological staging (high pT: OR = 1.86, 95% CI = 1.49–2.31; P < 0.01; pN+: OR = 1.61, 95% CI = 1.33–1.94; P < 0.01; high TNM category: OR = 1.84, 95% CI = 1.53–2.22; P < 0.01). Patients with preoperative sarcopenia had an increased risk of total postoperative complications (OR = 2.17, 95% CI = 1.53–3.08; P < 0.01), severe complications (OR = 1.65, 95% CI = 1.09–2.50; P = 0.02), and poorer OS (HR = 1.70, 95% CI = 1.45–1.99; P < 0.01). The results of subgroup analyses revealed that patients with preoperative sarcopenia over 65 years old and those from Asian populations had higher risks for total postoperative complications and severe complications.
Conclusion
This meta-analysis reveals that preoperative sarcopenia may be used as a new indicator of poor pathological staging, impaired overall survival, and increased postoperative complications. Notably, patients with gastric cancer who are over 65 years old and from Asia should be routinely screened for sarcopenia before surgery to adequately assess the risk of postoperative complications in clinical practice.





Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA: a cancer journal for clinicians. 2017;67(1):7–30. https://doi.org/10.3322/caac.21387.
Zhou J, Zhou Y, Cao S, Li S, Wang H, Niu Z et al. Multivariate logistic regression analysis of postoperative complications and risk model establishment of gastrectomy for gastric cancer: A single-center cohort report. Scandinavian Journal of Gastroenterology. 2016;51(1):8–15. https://doi.org/10.3109/00365521.2015.1063153.
Zhou CJ, Chen FF, Zhuang CL, Pang WY, Zhang FY, Huang DD et al. Feasibility of radical gastrectomy for elderly patients with gastric cancer. European Journal of Surgical Oncology : the Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2016;42(2):303–11. https://doi.org/10.1016/j.ejso.2015.11.013.
Kubota T, Hiki N, Sano T, Nomura S, Nunobe S, Kumagai K et al. Prognostic significance of complications after curative surgery for gastric cancer. Annals of Surgical Oncology. 2014;21(3):891–8. https://doi.org/10.1245/s10434-013-3384-9.
Li QG, Li P, Tang D, Chen J, Wang DR. Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World Journal of Gastroenterology. 2013;19(25):4060–5. https://doi.org/10.3748/wjg.v19.i25.4060.
Nakashima Y, Saeki H, Nakanishi R, Sugiyama M, Kurashige J, Oki E et al. Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Annals of Surgery. 2017. https://doi.org/10.1097/SLA.0000000000002252.
Begini P, Gigante E, Antonelli G, Carbonetti F, Iannicelli E, Anania G et al. Sarcopenia predicts reduced survival in patients with hepatocellular carcinoma at first diagnosis. Annals of Hepatology. 2017;16(1):107–14. https://doi.org/10.5604/16652681.1226821.
Sharma P, Zargar-Shoshtari K, Caracciolo JT, Fishman M, Poch MA, Pow-Sang J et al. Sarcopenia as a predictor of overall survival after cytoreductive nephrectomy for metastatic renal cell carcinoma. Urologic Oncology. 2015;33(8):339 e17–23. https://doi.org/10.1016/j.urolonc.2015.01.011.
Nishigori T, Tsunoda S, Okabe H, Tanaka E, Hisamori S, Hosogi H et al. Impact of sarcopenic obesity on surgical site infection after laparoscopic total gastrectomy. Annals of surgical Oncology. 2016;23(Suppl 4):524–31. https://doi.org/10.1245/s10434-016-5385-y.
Tamandl D, Paireder M, Asari R, Baltzer PA, Schoppmann SF, Ba-Ssalamah A. Markers of sarcopenia quantified by computed tomography predict adverse long-term outcome in patients with resected oesophageal or gastro-oesophageal junction cancer. European Radiology. 2016;26(5):1359–67. https://doi.org/10.1007/s00330-015-3963-1.
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. The Lancet Oncology. 2008;9(7):629–35. https://doi.org/10.1016/S1470-2045(08)70153-0.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age and ageing. 2010;39(4):412–23. https://doi.org/10.1093/ageing/afq034.
Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. European journal of cancer. 2016;57:58–67. https://doi.org/10.1016/j.ejca.2015.12.030.
Pamoukdjian F, Bouillet T, Levy V, Soussan M, Zelek L, Paillaud E. Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: A systematic review. Clinical Nutrition. 2017. https://doi.org/10.1016/j.clnu.2017.07.010.
Lou N, Chi CH, Chen XD, Zhou CJ, Wang SL, Zhuang CL et al. Sarcopenia in overweight and obese patients is a predictive factor for postoperative complication in gastric cancer: A prospective study. European Journal of Surgical Oncology : the Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2017;43(1):188–95. https://doi.org/10.1016/j.ejso.2016.09.006.
Zhou CJ, Zhang FM, Zhang FY, Yu Z, Chen XL, Shen X et al. Sarcopenia: a new predictor of postoperative complications for elderly gastric cancer patients who underwent radical gastrectomy. The Journal of Surgical Research. 2017;211:137–46. https://doi.org/10.1016/j.jss.2016.12.014.
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T et al. Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer : Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2016;19(3):986–93. https://doi.org/10.1007/s10120-015-0546-4.
Zhuang CL, Huang DD, Pang WY, Zhou CJ, Wang SL, Lou N et al. Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: analysis from a large-scale cohort. Medicine. 2016;95(13):e3164. https://doi.org/10.1097/MD.0000000000003164.
Tegels JJ, van Vugt JL, Reisinger KW, Hulsewe KW, Hoofwijk AG, Derikx JP et al. Sarcopenia is highly prevalent in patients undergoing surgery for gastric cancer but not associated with worse outcomes. Journal of Surgical Oncology. 2015;112(4):403–7. https://doi.org/10.1002/jso.24015.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Kudou K, Saeki H, Nakashima Y, Edahiro K, Korehisa S, Taniguchi D et al. Prognostic significance of sarcopenia in patients with esophagogastric junction cancer or upper gastric cancer. Annals of Surgical Oncology. 2017;24(7):1804–10. https://doi.org/10.1245/s10434-017-5811-9.
Black D, Mackay C, Ramsay G, Hamoodi Z, Nanthakumaran S, Park KGM et al. Prognostic value of computed tomography: measured parameters of body composition in primary operable gastrointestinal cancers. Annals of Surgical Oncology. 2017;24(8):2241–51. https://doi.org/10.1245/s10434-017-5829-z.
Huang DD, Chen XX, Chen XY, Wang SL, Shen X, Chen XL et al. Sarcopenia predicts 1-year mortality in elderly patients undergoing curative gastrectomy for gastric cancer: a prospective study. Journal of Cancer Research and Clinical Oncology. 2016;142(11):2347–56. https://doi.org/10.1007/s00432-016-2230-4.
Chen FF, Zhang FY, Zhou XY, Shen X, Yu Z, Zhuang CL. Role of frailty and nutritional status in predicting complications following total gastrectomy with D2 lymphadenectomy in patients with gastric cancer: a prospective study. Langenbeck’s Archives of Surgery. 2016;401(6):813–22. https://doi.org/10.1007/s00423-016-1490-4.
Huang DD, Zhou CJ, Wang SL, Mao ST, Zhou XY, Lou N et al. Impact of different sarcopenia stages on the postoperative outcomes after radical gastrectomy for gastric cancer. Surgery. 2017;161(3):680–93. https://doi.org/10.1016/j.surg.2016.08.030.
Mirkin KA, Luke FE, Gangi A, Pimiento JM, Jeong D, Hollenbeak CS et al. Sarcopenia related to neoadjuvant chemotherapy and perioperative outcomes in resected gastric cancer: a multi-institutional analysis. Journal of Gastrointestinal Oncology. 2017;8(3):589–95. https://doi.org/10.21037/jgo.2017.03.02.
Sakurai K, Kubo N, Tamura T, Toyokawa T, Amano R, Tanaka H et al. Adverse effects of low preoperative skeletal muscle mass in patients undergoing gastrectomy for gastric cancer. Annals of Surgical Oncology. 2017;24(9):2712–9. https://doi.org/10.1245/s10434-017-5875-6.
Sato T, Aoyama T, Hayashi T, Segami K, Kawabe T, Fujikawa H et al. Impact of preoperative hand grip strength on morbidity following gastric cancer surgery. Gastric Cancer : Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2016;19(3):1008–15. https://doi.org/10.1007/s10120-015-0554-4.
Wang SL, Zhuang CL, Huang DD, Pang WY, Lou N, Chen FF et al. Sarcopenia adversely impacts postoperative clinical outcomes following gastrectomy in patients with gastric cancer: a prospective study. Annals of Surgical Oncology. 2016;23(2):556–64. https://doi.org/10.1245/s10434-015-4887-3.
Zheng ZF, Lu J, Zheng CH, Li P, Xie JW, Wang JB et al. A novel prognostic scoring system based on preoperative sarcopenia predicts the long-term outcome for patients after R0 resection for gastric cancer: experiences of a high-volume center. Annals of Surgical Oncology. 2017;24(7):1795–803. https://doi.org/10.1245/s10434-017-5813-7.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al. The Clavien-Dindo classification of surgical complications: five-year experience. Annals of Surgery. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Rolland Y, Czerwinski S, Abellan Van Kan G, Morley JE, Cesari M, Onder G et al. Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. The Journal of Nutrition, Health & Aging. 2008;12(7):433–50.
Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007;297(16):1772–4. https://doi.org/10.1001/jama.297.16.1772-b.
Doherty TJ. Invited review: Aging and sarcopenia. Journal of Applied Physiology. 2003;95(4):1717–27. https://doi.org/10.1152/japplphysiol.00347.2003.
Koo BK, Roh E, Yang YS, Moon MK. Difference between old and young adults in contribution of beta-cell function and sarcopenia in developing diabetes mellitus. Journal of Diabetes Investigation. 2016;7(2):233–40. https://doi.org/10.1111/jdi.12392.
Morley JE, Kaiser FE, Perry HM, 3rd, Patrick P, Morley PM, Stauber PM et al. Longitudinal changes in testosterone, luteinizing hormone, and follicle-stimulating hormone in healthy older men. Metabolism: Clinical and Experimental. 1997;46(4):410–3.
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB et al. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2002;57(5):M326–32.
Cesari M, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BW, Lenchik L et al. Sarcopenia, obesity, and inflammation—results from the Trial of Angiotensin Converting Enzyme Inhibition and Novel Cardiovascular Risk Factors study. The American Journal of Clinical Nutrition. 2005;82(2):428–34.
Rizzoli R. Nutrition and sarcopenia. Journal of Clinical Densitometry : the Official Journal of the International Society for Clinical Densitometry. 2015;18(4):483–7. https://doi.org/10.1016/j.jocd.2015.04.014.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. Journal of the American Medical Directors Association. 2011;12(4):249–56. https://doi.org/10.1016/j.jamda.2011.01.003.
Miyamoto Y, Baba Y, Sakamoto Y, Ohuchi M, Tokunaga R, Kurashige J et al. Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Annals of Surgical Oncology. 2015;22(8):2663–8. https://doi.org/10.1245/s10434-014-4281-6.
Levolger S, van Vledder MG, Muslem R, Koek M, Niessen WJ, de Man RA et al. Sarcopenia impairs survival in patients with potentially curable hepatocellular carcinoma. Journal of Surgical Oncology. 2015;112(2):208–13. https://doi.org/10.1002/jso.23976.
Psutka SP, Boorjian SA, Moynagh MR, Schmit GD, Costello BA, Thompson RH et al. Decreased skeletal muscle mass is associated with an increased risk of mortality after radical nephrectomy for localized renal cell cancer. The Journal of Urology. 2016;195(2):270–6. https://doi.org/10.1016/j.juro.2015.08.072.
Levolger S, van Vugt JL, de Bruin RW, JN IJzermans. Systematic review of sarcopenia in patients operated on for gastrointestinal and hepatopancreatobiliary malignancies. The British Journal of Surgery. 2015;102(12):1448–58. https://doi.org/10.1002/bjs.9893.
Papenfuss WA, Kukar M, Oxenberg J, Attwood K, Nurkin S, Malhotra U et al. Morbidity and mortality associated with gastrectomy for gastric cancer. Annals of Surgical Oncology. 2014;21(9):3008–14. https://doi.org/10.1245/s10434-014-3664-z.
Jiang N, Deng JY, Ding XW, Zhang L, Liu HG, Liang YX et al. Effect of complication grade on survival following curative gastrectomy for carcinoma. World Journal of Gastroenterology. 2014;20(25):8244–52. https://doi.org/10.3748/wjg.v20.i25.8244.
Hayashi T, Yoshikawa T, Aoyama T, Ogata T, Cho H, Tsuburaya A. Severity of complications after gastrectomy in elderly patients with gastric cancer. World Journal of Surgery. 2012;36(9):2139–45. https://doi.org/10.1007/s00268-012-1653-6.
Prado CM, Heymsfield SB. Lean tissue imaging: a new era for nutritional assessment and intervention. JPEN Journal of Parenteral and Enteral Nutrition. 2014;38(8):940–53. https://doi.org/10.1177/0148607114550189.
Hall JC. Nutritional assessment of surgery patients. Journal of the American College of Surgeons. 2006;202(5):837–43. https://doi.org/10.1016/j.jamcollsurg.2005.12.010.
Lutz CT, Quinn LS. Sarcopenia, obesity, and natural killer cell immune senescence in aging: altered cytokine levels as a common mechanism. Aging 2012;4(8):535–46. https://doi.org/10.18632/aging.100482.
Bahat G, Tufan A, Ozkaya H, Tufan F, Akpinar TS, Akin S et al. Relation between hand grip strength, respiratory muscle strength and spirometric measures in male nursing home residents. The Aging Male: the Official Journal of the International Society for the Study of the Aging Male. 2014;17(3):136–40. https://doi.org/10.3109/13685538.2014.936001.
Wu XJ, Miao RL, Li ZY, Bu ZD, Zhang LH, Wu AW et al. Prognostic value of metastatic lymph node ratio as an additional tool to the TNM stage system in gastric cancer. European Journal of Surgical Oncology: the Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2015;41(7):927–33. https://doi.org/10.1016/j.ejso.2015.03.225.
Di Girolamo FG, Situlin R, Mazzucco S, Valentini R, Toigo G, Biolo G. Omega-3 fatty acids and protein metabolism: enhancement of anabolic interventions for sarcopenia. Current Opinion in Clinical Nutrition and Metabolic Care. 2014;17(2):145–50. https://doi.org/10.1097/MCO.0000000000000032.
Phillips SM. Nutritional supplements in support of resistance exercise to counter age-related sarcopenia. Advances in Nutrition. 2015;6(4):452–60. https://doi.org/10.3945/an.115.008367.
Yamamoto K, Nagatsuma Y, Fukuda Y, Hirao M, Nishikawa K, Miyamoto A et al. Effectiveness of a preoperative exercise and nutritional support program for elderly sarcopenic patients with gastric cancer. Gastric Cancer: Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2017;20(5):913–8. https://doi.org/10.1007/s10120-016-0683-4.
Aoyama T, Yoshikawa T. Adjuvant therapy for locally advanced gastric cancer. Surgery Today. 2017;47(11):1295–302. https://doi.org/10.1007/s00595-017-1493-y.
Fuentes E, Ahmad R, Hong TS, Clark JW, Kwak EL, Rattner DW et al. The impact of neoadjuvant therapy for gastroesophageal adenocarcinoma on postoperative morbidity and mortality. Journal of surgical oncology. 2016;113(5):560–4. https://doi.org/10.1002/jso.24179.
Qi J, Zhang P, Wang Y, Chen H, Li Y. Does total gastrectomy provide better outcomes than distal subtotal gastrectomy for distal gastric cancer? A systematic review and meta-analysis. PloS one. 2016;11(10):e0165179. https://doi.org/10.1371/journal.pone.0165179.
Acknowledgements
We thank the department of Surgical Oncology of First Hospital of China Medical University for technical assistance in this analysis.
Funding
This study was funded by Key Laboratory Grant of Education Department of Liaoning Province (grant number LS201602).
Author information
Authors and Affiliations
Contributions
Study concepts: Yanan Xing
Study design: Zhengdao Yang; Yanan Xing
Data acquisition: Zhengdao Yang; Xin Zhou
Quality control of data and algorithms: Bin Ma
Data analysis and interpretation: Zhengdao Yang; Xin Zhou
Manuscript preparation: Zhengdao Yang; Xin Zhou
Manuscript review: Xue Jiang; Zhenning Wang
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic Supplementary Material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Yang, Z., Zhou, X., Ma, B. et al. Predictive Value of Preoperative Sarcopenia in Patients with Gastric Cancer: a Meta-analysis and Systematic Review. J Gastrointest Surg 22, 1890–1902 (2018). https://doi.org/10.1007/s11605-018-3856-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3856-0