Abstract
Background
Evidence suggests that high-volume facilities achieve better rectal cancer outcomes.
Methods
Logistic regression was used to evaluate association of facility type with treatment after adjusting for patient demographics, stage, and comorbidities. SEER-Medicare beneficiaries who were diagnosed with stage II/III rectal adenocarcinoma at age ≥66 years from 2005 to 2009 and had Parts A/B Medicare coverage for ≥1 year prediagnosis and postdiagnosis plus a claim for cancer-directed surgery were included. Institutions were classified according to National Cancer Institute (NCI) designation, presence of residency program, or medical school affiliation.
Results
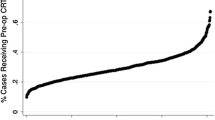
Two thousand three hundred subjects (average age = 75) met the criteria. Greater proportions of those treated at NCI-designated facilities received transrectal ultrasound (TRUS) or magnetic resonance imaging (MRI)-pelvis (62.1 vs. 29.9 %), neoadjuvant chemotherapy (63.9 vs. 41.8 %), and neoadjuvant radiation (70.8 vs. 46.3 %), all p < 0.0001. On multivariate analysis, odds ratios (95 % confidence intervals) for receiving TRUS or MRI, neoadjuvant chemotherapy, or neoadjuvant radiation among beneficiaries treated at NCI-designated facilities were 3.51 (2.60–4.73), 2.32 (1.71–3.16), and 2.66 (1.93–3.67), respectively. Results by residency and medical school affiliation were similar in direction to NCI designation.
Conclusions
Those treated at hospitals with an NCI designation, residency program, or medical school affiliation received more guideline-concordant care. Initiatives involving provider education and virtual tumor boards may improve care.

Similar content being viewed by others
References
Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27:4671–4678.
Stitzenberg KB, Meropol NJ. Trends in centralization of cancer surgery. Ann Surg Oncol. 2010;17:2824–2831.
Salz T, Sandler RS. The effect of hospital and surgeon volume on outcomes for rectal cancer surgery. Clin Gastroenterol Hepatol. 2008;6:1185–1193.
Rogers SO, Jr., Ayanian JZ, Ko CY, Kahn KL, Zaslavsky AM, Sandler RS, Keating NL. Surgeons' volume of colorectal cancer procedures and collaborative decision-making about adjuvant therapies. Ann Surg. 2009;250:895–900.
Archampong D, Borowski DW, Dickinson HO. Impact of surgeon volume on outcomes of rectal cancer surgery: a systematic review and meta-analysis. Surgeon. 2010;8:341–352.
Nugent E, Neary P. Rectal cancer surgery: volume-outcome analysis. Int J Colorectal Dis. 2010;25:1389–1396.
Schrag D, Panageas KS, Riedel E, Cramer LD, Guillem JG, Bach PB, Begg CB. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann Surg. 2002;236:583–592.
Billingsley KG, Morris AM, Green P, Dominitz JA, Matthews B, Dobie SA, Barlow W, Baldwin LM. Does surgeon case volume influence nonfatal adverse outcomes after rectal cancer resection? J Am Coll Surg. 2008;206:1167–1177.
Bilimoria KY, Bentrem DJ, Talamonti MS, Stewart AK, Winchester DP, Ko CY. Risk-based selective referral for cancer surgery: a potential strategy to improve perioperative outcomes. Ann Surg. 2010;251:708–716.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Rectal Cancer;Version 3.2014.
National Cancer Institute. SEER-Medicare Linked Database. http://appliedresearch.cancer.gov/seermedicare/. Accessed Oct 9, 2015.
University of Washington WWAMI Rural Health Research Center. Rural–urban Commuting Areas (RUCA) Version 1.11. http://depts.washington.edu/uwruca/ruca-uses.php. Accessed Oct 9, 2015.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Klabunde CN, Potosky AL, Legler JM, Warren, JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267.
Davey K, Heriot AG, Mackay J, Drummond E, Hogg A, Ngan S, Milner AD, Hicks RJ. The impact of 18-fluorodeoxyglucose positron emission tomography-computed tomography on the staging and management of primary rectal cancer. Dis Colon Rectum. 2008;51:997–1003.
Gearhart SL, Frassica D, Rosen R, Choti M, Schulick R, Wahl R. Improved staging with pretreatment positron emission tomography/computed tomography in low rectal cancer. Ann Surgical Oncol. 2006;13:397–404.
Heriot AG, Hicks RJ, Drummond EG, Keck J, Mackay J, Chen F, Kalff V. Does positron emission tomography change management in primary rectal cancer? A prospective assessment. Dis Colon Rectum. 2004;47:451–458.
Charlton ME, Lin C, Jiang D, Stitzenberg KB, Halfdanarson TR, Pendergast JF, Chrischilles EA, Wallace RB. Factors associated with use of preoperative chemoradiation therapy for rectal cancer in the Cancer Care Outcomes Research and Surveillance Consortium. Am J Clin Oncol. 2013;36:572–579.
Hyman N, Healey C, Osler T, Cataldo, P. Understanding variation in the management of rectal cancer: the potential of a surgeon-initiated database. Am J Surg. 2007;194:559–562.
McMullen TP, Easson AM, Cohen Z, Swallow, CJ. The investigation of primary rectal cancer by surgeons: current pattern of practice. Can J Surg. 2005;48:19–26.
Chen VW, Hsieh MC, Charlton ME, Ruiz BA, Karlitz J, Altekruse SF, Ries LA, Jessup JM. Analysis of stage and clinical/prognostic factors for colon and rectal cancer from SEER Registries: AJCC and collaborative stage data collection system. Cancer. 2014;120:3793–806.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1973–2010), National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch, released April 2013, based on the November 2012 submission.
Monson JR, Probst CP, Wexner SD, Remzi FH, Fleshman JW, Garcia-Aguilar J, Chang GJ, Dietz DW. Failure of evidence-based cancer care in the United States: the association between rectal cancer treatment, cancer center volume, and geography. Ann Surg. 2014;260:625–631.
American College of Surgeons. About the National Cancer Data Base. https://www.facs.org/quality-programs/cancer/ncdb/about. Accessed Oct 11, 2015.
Meyerhardt JA, Tepper JE, Niedzwiecki D, Hollis DR, Schrag D, Ayanian JZ, O'Connell MJ, Weeks JC, Mayer RJ, Willett CG, MacDonald JS, Benson AB 3rd, Fuchs CS. Impact of hospital procedure volume on surgical operation and long-term outcomes in high-risk curatively resected rectal cancer: findings from the Intergroup 0114 Study. J Clin Oncol. 2004;22:166–174.
Paquette IM, Kemp JA, Finlayson SR. Patient and hospital factors associated with use of sphincter-sparing surgery for rectal cancer. Dis Colon Rectum. 2010;53:115–120.
Purves H, Pietrobon R, Hervey S, Guller U, Miller W, Ludwig K. Relationship between surgeon caseload and sphincter preservation in patients with rectal cancer. Dis Colon Rectum. 2005;48:195–202.
Ricciardi R, Roberts PL, Read TE, Baxter NN, Marcello PW, Schoetz DJ. Who performs proctectomy for rectal cancer in the United States? Dis Colon Rectum. 2011;54:1210–1215.
Ricciardi R, Roberts PL, Read TE, Baxter NN, Marcello PW, Schoetz DJ. Presence of specialty surgeons reduces the likelihood of colostomy after proctectomy for rectal cancer. Dis Colon Rectum. 2011;54:207–213.
In H, Neville BA, Lipsitz SR, Corso KA, Weeks JC, Greenberg CC. The role of National Cancer Institute-designated cancer center status: observed variation in surgical care depends on the level of evidence. Ann Surg. 2012;255:890–895.
Paulson EC, Mitra N, Sonnad S, Armstrong K, Wirtalla C, Kelz RR, Mahmoud NN. National Cancer Institute designation predicts improved outcomes in colorectal cancer surgery. Ann Surg. 2008;248:675–686.
National Cancer Institute. NCI-Designated Cancer Centers. http://www.cancer.gov/research/nci-role/cancer-centers. Accessed Oct 11, 2015.
Dietz DW. Multidisciplinary management of rectal cancer: the OSTRICH. J Gastrointest Surg. 2013;17:1863–1868.
Marshall CL, Petersen NJ, Naik AD, Vander Velde N, Artinyan A, Albo D, Berger DH, Anaya DA. Implementation of a regional virtual tumor board: A prospective study evaluating feasibility and provider acceptance. Telemed J E Health. 2014;20:705–711.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Grant Support and Other Assistance
This work was supported by a pilot award from the University of Iowa Holden Comprehensive Cancer Center, which is supported in part by the National Cancer Institute at the National Institutes of Health (P30 CA086862). Technical assistance was provided by the University of Iowa Holden Comprehensive Cancer Center Population Research Core.
This work has been previously presented in part as an abstract E-poster at the American Society of Colon and Rectal Surgeons Annual Scientific Meeting, Hollywood, FL, May 17–21, 2014, and as an abstract poster presentation at the American College of Epidemiology Annual Meeting, Silver Spring, MD, September 8–9, 2014.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Online only Table 1
Codes and SEER-Medicare files used to identify pre-treatment and treatment variables (DOC 40 kb)
Rights and permissions
About this article
Cite this article
Charlton, M.E., Hrabe, J.E., Wright, K.B. et al. Hospital Characteristics Associated with Stage II/III Rectal Cancer Guideline Concordant Care: Analysis of Surveillance, Epidemiology and End Results-Medicare Data. J Gastrointest Surg 20, 1002–1011 (2016). https://doi.org/10.1007/s11605-015-3046-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-3046-2