Abstract
Background
For medically refractory or obstructive Crohn’s disease (CD), ostomy surgery remains an important therapeutic option. Outcomes and complications of this approach have not been well described in the era of biological therapies. Our study aims to characterize CD patients undergoing ostomy creation and assess outcome predictors.
Methods
We performed a retrospective chart review of CD patients who underwent ostomy creation in our center from 2011 to 2014. Data collected include patient demographics, detailed disease- and surgery-related variables, and clinical outcomes after 26 weeks of follow-up.
Results
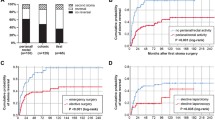
Of the 112 patients, 54 % were female, the median age was 39 years (range 19–78), the median disease duration was 13 years (range 0–50), 54 % had ileo-colonic disease, 55 % had stricturing phenotype, and 59 % had perianal disease. Sixty-two percent received end ostomies, and 38 % received loop ostomies. The leading indications for surgery were stricturing, fistulizing, and perianal disease (35 %). Forty-three (38 %) patients had 76 major complications, including dehydration (22 cases), intra-abdominal infection (16), and obstruction (14). Increased major postoperative complications correlated with penetrating disease (p = 0.02, odds ratio [OR] = 5.52, 95 % confidence interval [CI] = 1.25–24.42), the use of narcotics before surgery (p = 0.04, OR = 2.54, 95 % CI = 1.02–6.34), and loop ostomies (p = 0.004, OR = 4.2, 95 % CI = 1.57–11.23).
Conclusions
Penetrating phenotype, the use of narcotics before surgery, and loop ostomies are associated with major complications in CD patients undergoing ostomy creation. These findings may influence risk management of CD patients needing ostomies.



Similar content being viewed by others
References
Peyrin-Biroulet L, Loftus EV, Jr., Colombel JF, Sandborn WJ. The natural history of adult Crohn’s disease in population-based cohorts. The American journal of gastroenterology 2010;105:289–97.
McIlrath DC. Diverting ileostomy or colostomy in the management of Crohn’s disease of the colon. Archives of surgery 1971;103:308–10.
Zelas P, Jagelman DG. Loop illeostomy in the management of Crohn’s colitis in the debilitated patient. Annals of surgery 1980;191:164–8.
Coscia M, Gentilini L, Laureti S, et al. Risk of permanent stoma in extensive Crohn’s colitis: the impact of biological drugs. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2013;15:1115–22.
Ludwig KA, Milsom JW, Church JM, Fazio VW. Preliminary experience with laparoscopic intestinal surgery for Crohn’s disease. American journal of surgery 1996;171:52–5; discussion 5–6.
Regimbeau JM, Panis Y, Pocard M, et al. Long-term results of ileal pouch-anal anastomosis for colorectal Crohn’s disease. Diseases of the colon and rectum 2001;44:769–78.
Colombel JF, Loftus EV, Jr., Tremaine WJ, et al. Early postoperative complications are not increased in patients with Crohn’s disease treated perioperatively with infliximab or immunosuppressive therapy. The American journal of gastroenterology 2004;99:878–83.
Marchal L, D’Haens G, Van Assche G, et al. The risk of post-operative complications associated with infliximab therapy for Crohn’s disease: a controlled cohort study. Alimentary pharmacology & therapeutics 2004;19:749–54.
de Miguel Velasco M, Jimenez Escovar F, Parajo Calvo A. [Current status of the prevention and treatment of stoma complications. A narrative review]. Cirugia espanola 2014;92:149–56.
Porter JA, Salvati EP, Rubin RJ, Eisenstat TE. Complications of colostomies. Diseases of the colon and rectum 1989;32:299–303.
Takahashi K, Funayama Y, Fukushima K, et al. Stoma-related complications in inflammatory bowel disease. Digestive surgery 2008;25:16–20.
Uchino M, Ikeuchi H, Matsuoka H, et al. Clinical features and management of parastomal pyoderma gangrenosum in inflammatory bowel disease. Digestion 2012;85:295–301.
Hoentjen F, Colwell JC, Hanauer SB. Complications of peristomal recurrence of Crohn’s disease: a case report and a review of literature. Journal of wound, ostomy, and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society / WOCN 2012;39:297–301.
Leal-Valdivieso C, Marin I, Manosa M, et al. Should we monitor Crohn’s disease patients for postoperative recurrence after permanent ileostomy? Inflammatory bowel diseases 2012;18:E196.
Markham DW, Ruppert M, Noel R, Surawicz CM. A parastomal hernia causing small-bowel obstruction. Journal of clinical gastroenterology 1996;22:218–9.
Parascandolo ME. Multiple ostomy complications in a patient with Crohn’s disease: a case study. Journal of wound, ostomy, and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society / WOCN 2001;28:236–41; discussion 41–3.
Tsao SK, Baker M, Nightingale JM. High-output stoma after small-bowel resections for Crohn’s disease. Nature clinical practice Gastroenterology & hepatology 2005;2:604–8; quiz 9.
Kelly C. WOC nurse consult: peristomal complication. Journal of wound, ostomy, and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society / WOCN 2012;39:425–7.
Carlsson E, Bosaeus I, Nordgren S. What concerns subjects with inflammatory bowel disease and an ileostomy? Scandinavian journal of gastroenterology 2003;38:978–84.
Knowles SR, Wilson J, Wilkinson A, et al. Psychological well-being and quality of life in Crohn’s disease patients with an ostomy: a preliminary investigation. Journal of wound, ostomy, and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society / WOCN 2013;40:623–9.
Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Diseases of the colon and rectum 2012;55:175–80.
Duchesne JC, Wang YZ, Weintraub SL, Boyle M, Hunt JP. Stoma complications: a multivariate analysis. The American surgeon 2002;68:961–6; discussion 6.
Bass EM, Del Pino A, Tan A, Pearl RK, Orsay CP, Abcarian H. Does preoperative stoma marking and education by the enterostomal therapist affect outcome? Diseases of the colon and rectum 1997;40:440–2.
Arumugam PJ, Bevan L, Macdonald L, et al. A prospective audit of stomas—analysis of risk factors and complications and their management. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2003;5:49–52.
Parmar KL, Zammit M, Smith A, et al. A prospective audit of early stoma complications in colorectal cancer treatment throughout the Greater Manchester and Cheshire colorectal cancer network. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2011;13:935–8.
Shabbir J, Britton DC. Stoma complications: a literature overview. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2010;12:958–64.
Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infections and mortality in association with therapies for Crohn’s disease: TREAT registry. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 2006;4:621–30.
Long MD, Martin C, Sandler RS, Kappelman MD. Increased risk of pneumonia among patients with inflammatory bowel disease. The American journal of gastroenterology 2013;108:240–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirsch, A., Yarur, A.J., Dezheng, H. et al. Penetrating Disease, Narcotic Use, and Loop Ostomy Are Associated with Ostomy and IBD-related Complications After Ostomy Surgery in Crohn’s Disease Patients. J Gastrointest Surg 19, 1852–1861 (2015). https://doi.org/10.1007/s11605-015-2908-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2908-y