Abstract
Background
Limited data are available regarding the natural history of patients undergoing primary surveillance for intraductal papillary mucinous neoplasm (IPMN). We hypothesize that symptoms, radiologic characteristics, and cytopathology will predict cancer risk during surveillance.
Methods
Between March 2002 and March 2010, 522 patients were diagnosed with IPMN at a single, high-volume institution. Low versus high oncologic risk was stratified prospectively. Patients with under 3 months of surveillance were excluded.
Results
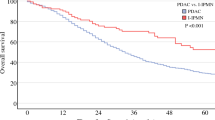
Two hundred ninety-two patients underwent primary surveillance for IPMN. Two hundred forty-four (84%) were classified as low-risk IPMN. Mean surveillance duration was 35 (4–99) months. Thirty (12%) patients initially stratified as low-risk developed a new indication for pancreatic resection. Only 28 underwent resection, and pathologic tissue analysis revealed 27 (96%) low-grade IPMN and one (4%) high-grade dysplastic IPMN. Overall, two (1%) patients initially determined to be low-risk developed invasive cancer. Forty-eight (16%) patients stratified as high-risk IPMN were initially managed nonoperatively. Of the 13 (27%) high-risk patients that died during follow-up, two (15%) died from pancreatic cancer.
Conclusions
Progression to pancreatic cancer during surveillance for low-risk IPMN was rare. Current indications for resection did not forecast malignancy. Poor operative candidates with high-risk IPMN progressed to invasive cancer more commonly, though a substantial portion succumbed to non-IPMN-related death.


Similar content being viewed by others
References
Sohn TA, Y.C., Cameron JL, Iacobuzio-Donahue CA, Hruban RH, Lillemoe KD., Intraductal papillary mucinous neoplasms of the pancreas: an increasingly recognized clinicopathologic entity. Ann Surg, 2001. 234(3): p. 313–21
Tanaka, M., et al., International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology, 2006. 6(1–2): p. 17–32.
Gourgiotis, S., M.P. Ridolfini, and S. Germanos, Intraductal papillary mucinous neoplasms of the pancreas. European Journal of Surgical Oncology (EJSO), 2007. 33(6): p. 678–684.
Hruban, R.H.M.T., Kyoichi MD, PhD; Klimstra, David S MD; Adsay, N Volkan MD; Albores-Saavedra, Jorge MD; Biankin, Andrew V MBBS, PhD; Biankin, Sandra A MBBS; Compton, Carolyn MD, PhD; Fukushima, Noriyoshi MD, PhD; Furukawa, Toru MD, PhD; Goggins, Michael MD; Kato, Yo MD, PhD; Kloppel, Gunter MD; Longnecker, Daniel S MD; Luttges, Jutta MD; Maitra, Anirban MBBS; Offerhaus, G Johan A MD; Shimizu, Michio MD, PhD; Yonezawa, Suguru MD, PhD, An Illustrated Consensus on the Classification of Pancreatic Intraepithelial Neoplasia and Intraductal Papillary Mucinous Neoplasms. The American Journal of Surgical Pathology, 2004. 28(8): p. 977–987.
Longnecker DS, A.G., Hruban RH, Kloppel G, Intraductal papillary-mucinous neoplasms of the pancreas, in World Health Organization Classification of Tumors. Pathology and Genetics of Tumors of the Digestive System:, A.L. Hamilton SR, Editor. 2000, Lyon, IARC Press. p. 237–241
Sho, M., et al., Pattern of Recurrence after Resection for Intraductal Papillary Mucinous Tumors of the Pancreas. World Journal of Surgery, 1998. 22(8): p. 874–878.
Sawai, Y., Yamao K, Bhatia V, Chiba T, N. Mizuno, A. Sawaki, K. Takahashi, M. Tajika, Y. Shimizu, Y. Yatabe, A. Yanagisawa, Development of pancreatic cancers during long-term follow-up of side-branch intraductal papillary mucinous neoplasms. Endoscopy, 2010. 42(12): p. 1077–1084.
D'Angelica M, B.M., Suriawinata AA, Klimstra D, Conlon KC., Intraductal papillary mucinous neoplasms of the pancreas: an analysis of clinicopathologic features and outcome. Ann Surg, 2004. 239(3): p. 400–8.
Spinelli KS, F.T., Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, Wilson SD, Pitt HA., Cystic pancreatic neoplasms: observe or operate. Ann Surg, 2004. 239(5): p. 651–7.
Pelaez-Luna, M., et al., Do Consensus Indications for Resection in Branch Duct Intraductal Papillary Mucinous Neoplasm Predict Malignancy[quest] A Study of 147 Patients. Am J Gastroenterol, 2007. 102(8): p. 1759–1764.
Raut, C., et al., Intraductal Papillary Mucinous Neoplasms of the Pancreas: Effect of Invasion and Pancreatic Margin Status on Recurrence and Survival. Annals of Surgical Oncology, 2006. 13(4): p. 582–594.
Farnell, M.B., Surgical management of intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Journal of Gastrointestinal Surgery, 2008. 12(3): p. 414–6.
Wiesenauer, C.A., et al., Preoperative Predictors of Malignancy in Pancreatic Intraductal Papillary Mucinous Neoplasms. Arch Surg, 2003. 138(6): p. 610–618.
Schmidt CM, W.P., Waters JA, Yiannoutsos CT, Cummings OW, Baker M, Howard TJ, Zyromski NJ, Nakeeb A, DeWitt JM, Akisik FM, Sherman S, Pitt HA, Lillemoe KD., Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann Surg, 2007. 246(4): p. 644–51.
Waters, J., et al., CT vs MRCP: Optimal Classification of IPMN Type and Extent. Journal of Gastrointestinal Surgery, 2008. 12(1): p. 101–109.
Salvia R, F.-d.C.C., Bassi C, Thayer SP, Falconi M, Mantovani W, Pederzoli P, Warshaw AL, Main duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and longterm survival following resection. . Ann Surg, 2004. 239: p. 678–687
Waters, J.A. and C.M. Schmidt, Intraductal Papillary Mucinous Neoplasm--When to Resect? Advances in Surgery, 2008. 42: p. 87–108.
Bassi, C., et al., Natural History of Intraductal Papillary Mucinous Neoplasms (IPMN): Current Evidence and Implications for Management. Journal of Gastrointestinal Surgery, 2008. 12(4): p. 645–650.
Rodriguez, J.R., et al., Branch-Duct Intraductal Papillary Mucinous Neoplasms: Observations in 145 Patients Who Underwent Resection. Gastroenterology, 2007. 133(1): p. 72–79.
Salvia, R., et al., Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut, 2007. 56(8): p. 1086–1090.
Sarr, M.G., et al., Primary cystic neoplasms of the pancreas. Neoplastic disorders of emerging importance-current state-of-the-art and unanswered questions. Journal of Gastrointestinal Surgery, 2003. 7(3): p. 417–28.
Schmidt, C.M. and K.D. Lillemoe, IPMN—Controversies in an “Epidemic”. Journal of Surgical Oncology, 2006. 94(2): p. 91–93.
Sohn, T.A., et al., Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Annals of Surgery, 2004. 239(6): p. 788–97; discussion 797–9
Bernard, P., et al., Intraductal Papillary-Mucinous Tumors of the Pancreas: Predictive Criteria of Malignancy According to Pathological Examination of 53 Cases. Arch Surg, 2002. 137(11): p. 1274–1278.
Sugiyama, M. and Y. Atomi, Extrapancreatic neoplasms occur with unusual frequency in patients with intraductal papillary mucinous tumors of the pancreas. Am J Gastroenterol, 1999. 94(2): p. 470–473.
White, R., et al., Fate of the Remnant Pancreas after Resection of Noninvasive Intraductal Papillary Mucinous Neoplasm. Journal of the American College of Surgeons, 2007. 204(5): p. 987–993.
Maker, A., et al., Pancreatic Cyst Fluid and Serum Mucin Levels Predict Dysplasia in Intraductal Papillary Mucinous Neoplasms of the Pancreas. Annals of Surgical Oncology, 2011. 18(1): p. 199–206.
Conflict of interest
There authors have no disclosures or conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Carlos Fernandez del Castillo (Boston, MA): Congratulations on a well-presented paper. This study, derived from a very large cohort of patients with IPMN, shows that at the time of diagnosis, only a third of patients undergo surgery. You have focused on the other two thirds. The majority of these patients, which were 244 in number, were deemed to have a very low risk of malignancy and were put under surveillance. Within a median follow-up of almost 3 years, two patients developed pancreatic cancer (less than 1%) and did not undergo surgery, and an additional 28 patients (11%) underwent resection for a variety of reasons, and none had invasive IPMN on pathology. These data are an important contribution to the field and are mostly in agreement with other studies that have followed up such patients. Although reassuring to the safety of follow-up of presumed branch duct IPMNs, we are all fully aware that much longer follow-up will be needed before we know the full story of this condition.
You also tell us about 48 patients who were deemed to have a high risk of harboring cancer within their IPMNs, but mostly because of advanced age or serious comorbidities did not undergo surgery but were still followed up. These comprise about 10% of the cohort. To my knowledge, no other series has focused on this subgroup. You had a mean follow-up of 42 months in them and show us that 15% of them died of pancreatic cancer, but that 5-year survival was 62%. This is very useful data for clinicians taking care of these patients.
I have two questions for you:
1. The average size of these asymptomatic cysts was 1.6 cm, which is quite small. Did all of these patients undergo EUS at the time of diagnosis, and if so, what kind of information did you obtain from this study?
2. Follow-up of this increasingly larger cohort of patients is a huge challenge. In what percent of them did you lose follow-up?
Closing Discussant
Dr. Christy E. Cauley: Thank you for your insightful comments and questions. As clinicians continue to accrue experience with these relatively uncommon pancreatic lesions, a number of questions have been answered, but still more remain unclear. Although the outcome of patients undergoing resection for IPMN has been well documented in the literature, those patients who undergo primary surveillance remain a largely unstudied group. With this substantial collection of low- and high-risk surveillance patients, we feel some remaining questions regarding the natural history of IPMN can be addressed. The findings in this study must be viewed in light of the indolent nature of IPMN and the relatively short median surveillance period. Given this limitation, we feel that your questions can be addressed with the following response.
Although the overall size of IPMN within the low-risk surveillance group was less than 2 cm, several patients were followed up with lesions measuring over 3 cm. Additionally, no relationship was revealed between the size or change in size of these lesions and the risk of malignancy. An important element of our risk stratification algorithm involves performing EUS to assess the lesion for high-risk features. Clearly, FNA may be difficult to perform for very small cysts; however, 83% of low-risk patients undergoing surveillance in this study underwent both EUS and FNA.
Within any study, particularly one focusing on surveillance, patient retention, and follow-up can be a challenge. This can be magnified in elderly patients who may be less interested in intense surveillance strategies. In our experience, 18% of low-risk patients and 21% of high-risk patients had three or more years with no recorded visits with gastroenterology or surgery and were considered lost to follow-up. It is feasible that some patients within this group may have developed undocumented disease progression.
Rights and permissions
About this article
Cite this article
Cauley, C.E., Waters, J.A., Dumas, R.P. et al. Outcomes of Primary Surveillance for Intraductal Papillary Mucinous Neoplasm. J Gastrointest Surg 16, 258–266 (2012). https://doi.org/10.1007/s11605-011-1757-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1757-6