Abstract
Introduction
Intra-abdominal adhesions are a significant source of postoperative morbidity. Bioresorbable barriers composed of hyaluronic acid and carboxymethylcellulose (HA/CMC) reduce adhesion formation by physically separating injured or healing peritoneal surfaces. To assess whether the efficacy of a physical barrier can extend beyond the site of application, we evaluated the effectiveness of an HA/CMC barrier in preventing adhesions distal to the site of placement.
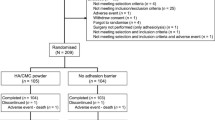
Methods
Adhesions were induced in rats by creating peritoneal ischemic buttons on either side of a midline incision. An HA/CMC barrier (Seprafilm™ Genzyme) was intraoperatively placed either under the midline incision, unilaterally over half the ischemic buttons, or bilaterally over all ischemic buttons. Control buttons received no HA/CMC. On day 7 adhesions were scored. In similar experiments, peritoneal fluid was collected at 24 h to assess the effects of HA/CMC on tissue plasminogen activator activity.
Results
Placement of HA/CMC under the midline incision did not reduce adhesion formation to distal ischemic buttons (72 ± 7%) compared to controls (80 ± 8%). Unilateral placement of HA/CMC significantly (p < 0.05) reduced adhesion formation to those ischemic buttons over which the barrier was applied (35 ± 7%) compared to both contralateral (83 ± 9%) and control (80 ± 8%) ischemic buttons. The bilateral application of HA/CMC also significantly (p < 0.05) reduced adhesion formation to all ischemic buttons compared to controls (22 ± 7% vs. 66 ± 7%, respectively). HA/CMC did not affect peritoneal tPA activity.
Conclusions
Effective adhesion reduction by the physical barrier HA/CMC appears to be limited to the site of application in this rat model. Despite the presence of a bioresorbable membrane at predicted sites of adhesion formation in the peritoneal cavity, adhesions readily form to distal unprotected sites.





Similar content being viewed by others
References
Ellis H. Postoperative intra-abdominal adhesions: a personal view. Colorectal Dis. 2007;9(Suppl 2):3–8. doi:10.1111/j.1463-1318.2007.01344.x.
Parker MC, Wilson MS, van Goor H, Moran BJ, Jeekel J, Duron JJ, et al. Adhesions and colorectal surgery—call for action. Colorectal Dis. 2007;9(Suppl 2):66–72. doi:10.1111/j.1463-1318.2007.01342.x.
Parker MC, Wilson MS, van Goor H, Moran BJ, Jeekel J, Duron JJ, et al. Adhesions and colorectal surgery—call for action. 2007;9:66–72.
Sileri P, Sthory R, McVeigh E, Child T, Cunningham C, Mortensen NJ, et al. Adhesions are common and costly after open pouch surgery. J Gastrointest Surg. 2008;12:1239–1245. doi:10.1007/s11605-008-0481-3.
van Goor H. Consequences and complications of peritoneal adhesions. Colorectal Dis. 2007;9(Suppl 2):25–34. doi:10.1111/j.1463-1318.2007.01358.x.
Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18:260–273. doi:10.1159/000050149.
Fevang BT, Fevang J, Lie SA, Soreide O, Svanes K, Viste A. Long-term prognosis after operation for adhesive small bowel obstruction. Ann Surg. 2004;240:193–201. doi:10.1097/01.sla.0000132988.50122.de.
Menzies D, Parker M, Hoare R, Knight A. Small bowel obstruction due to postoperative adhesions: treatment patterns and associated costs in 110 hospital admissions. Ann R Coll Surg Engl. 2001;83:40–46.
Tingstedt B, Andersson E, Isaksson K, Andersson R. Clinical impact of abdominal adhesions: What is the magnitude of the problem? Scand J Gastroenterol. 2008;43(3):255–261.
Wiseman DM. Adhesion Related Disease—Adhesions Related Deaths. 2003. Available at www.adhesion.org.
Wilson MS. Practicalities and costs of adhesions. Colorectal Dis. 2007;9(Suppl 2):60–65. doi:10.1111/j.1463-1318.2007.01360.x.
Wiseman DM. Adhesion Prevention: Past the Future. In diZerega GS, ed. Peritoneal Surgery. New York: Springer, 2000, pp 401–417.
Burns JW, Colt MJ, Burgees LS, Skinner KC. Preclinical evaluation of Seprafilm bioresorbable membrane. Eur J Surg Suppl. 1997;577:40–8.
Becker JM, Dayton MT, Fazio VW, Beck DE, Stryker SJ, Wexner SD, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg. 1996;183:297–306. see comments.
Vrijland WW, Tseng LN, Eijkman HJ, Hop WC, Jakimowicz JJ, Leguit P, et al. Fewer intraperitoneal adhesions with use of hyaluronic acid-carboxymethylcellulose membrane: a randomized clinical trial. Ann Surg. 2002;235:193–199. doi:10.1097/00000658-200202000-00006.
Hayashi S, Takayama T, Masuda H, Kochi M, Ishii Y, Matsuda M, et al. Bioresorbable membrane to reduce postoperative small bowel obstruction in patients with gastric cancer: a randomized clinical trial. Ann Surg. 2008;247:766–770. doi:10.1097/SLA.0b013e3181656d4e.
McLeod R. Does Seprafilm really reduce adhesive small bowel obstructions? Dis Colon Rectum. 2006;49:1234. author reply 1235–1236. doi:10.1007/s10350-006-0621-3.
diZerega GS, Campeau JD. Peritoneal repair and post-surgical adhesion formation. Hum Reprod Update. 2001;7:547–555. doi:10.1093/humupd/7.6.547.
Thompson J. Pathogenesis and prevention of adhesion formation. Dig Surg. 1998;15:153–157. doi:10.1159/000018610.
Holmdahl L.. The role of fibrinolysis in adhesion formation. Eur J Surg Suppl 1997;577:24–31.
Sikkink CJ, Reijnen MM, Falk P, van Goor H, Holmdahl L. Influence of monocyte-like cells on the fibrinolytic activity of peritoneal mesothelial cells and the effect of sodium hyaluronate. Fertil Steril. 2005;84(Suppl 2):1072–1077. doi:10.1016/j.fertnstert.2005.03.078.
Binnebosel M, Rosch R, Junge K, Lynen-Jansen P, Schumpelick V, Klinge U. Macrophage and T-lymphocyte infiltrates in human peritoneal adhesions indicate a chronic inflammatory disease. World J Surg. 2008;32:296–304. doi:10.1007/s00268-007-9330-x.
van der Wal JB, Jeekel J. Biology of the peritoneum in normal homeostasis and after surgical trauma. Colorectal Dis. 2007;9(Suppl 2):9–13. doi:10.1111/j.1463-1318.2007.01345.x.
Holmdahl L, Eriksson E, Eriksson BI, Risberg B. Depression of peritoneal fibrinolysis during operation is a local response to trauma. Surgery. 1998;123:539–544. doi:10.1067/msy.1998.86984.
Reed KL, Fruin AB, Bishop-Bartolomei KK, Gower AC, Nicolaou M, Stucchi AF, et al. Neurokinin-1 receptor and substance P messenger RNA levels increase during intraabdominal adhesion formation. J Surg Res. 2002;108:165–172. doi:10.1006/jsre.2002.6533.
Cohen PA, Aarons CB, Gower AC, Stucchi AF, Leeman SE, Becker JM, et al. The effectiveness of a single intraperitoneal infusion of a neurokinin-1 receptor antagonist in reducing postoperative adhesion formation is time dependent. Surgery. 2007;141:368–375. doi:10.1016/j.surg.2006.09.007.
Maetani S, Tobe T, Kashiwara S. Neglected role of torsion and constriction in pathogenesis of simple adhesive bowel obstruction. Br J Surg. 1984;71:127–130. doi:10.1002/bjs.1800710217.
Fazio VW, Cohen Z, Fleshman JW, van Goor H, Bauer JJ, Wolff BG, et al. Reduction in adhesive small-bowel obstruction by Seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum. 2006;49:1–11. doi:10.1007/s10350-005-0268-5.
Reed KL, Fruin AB, Gower AC, Stucchi AF, Leeman SE, Becker JM. A neurokinin 1 receptor antagonist decreases postoperative peritoneal adhesion formation and increases peritoneal fibrinolytic activity. Proc Natl Acad Sci U S A. 2004;101:9115–9120. doi:10.1073/pnas.0403210101.
Holmdahl L, Eriksson E, al-Jabreen M, Risberg B. Fibrinolysis in human peritoneum during operation. Surgery. 1996;119:701–705. doi:10.1016/S0039-6060(96)80196-6.
Tarhan OR, Eroglu A, Cetin RAYN, Bulbul M, Altuntas YR. Effects of seprafilm on peritoneal fibrinolytic system. ANZ J Surg. 2005;75:690–692. doi:10.1111/j.1445-2197.2005.03483.x.
Aarons CB, Cohen PA, Gower A, Reed KL, Leeman SE, Stucchi AF, et al. Statins (HMG-CoA reductase inhibitors) decrease postoperative adhesions by increasing peritoneal fibrinolytic activity. Ann Surg. 2007;245:176–184. doi:10.1097/01.sla.0000236627.07927.7c.
Heydrick SJ, Reed KL, Cohen PA, Aarons CB, Gower AC, Becker JM, et al. Intraperitoneal administration of methylene blue attenuates oxidative stress, increases peritoneal fibrinolysis, and inhibits intraabdominal adhesion formation. J Surg Res. 2007;143:311–319. doi:10.1016/j.jss.2006.11.012.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussion
Margo Shoup, M.D. (Maywood, IL): I would like to congratulate the authors for trying to tackle a difficult problem that we all face with our patients with adhesion formation in a small bowel obstruction, and we really haven't made much headway in this in the last couple of decades. The authors in this paper attempt to study the effects of HA/CMC, or seprafilm, and neurokinin-1 receptor antagonist. The adhesions were measured at seven days postoperatively and placement of the buttons, and the Tpa was measured 24 hours after laparotomy. And we know that the synergistic effects of NK1RA and seprafilm is evident, but we are not really sure what is going on with the Tpa during all that. So I have a few questions for you.
Have you first looked at dose escalation studies with increasing NK1 receptor antagonists to evaluate the effects on Tpa, because this would clarify whether this is truly the mechanisms through which this is working. Also, you checked the Tpa levels 24 hours after surgery and, like I said, the adhesions at seven days. Have you looked at different time frames for both of these to see if there is more of a correlation? And at this point do you have any information on the status of the soluble seprafilm that is available in Europe, and if so, where do you think this may impact your study?
Thank you.
Rizal Lim, M.D. (Boston, MA): In terms of dose escalation of our antagonist, going back to the original parent compound, it is actually based off of a drug called ezlopitant. When we received this compound as a gift, the doses were actually based on the then maximum recommended dose of 25 mg/kg, which we used. But in earlier studies, as we started off with 5 mg/kg and then went to 10 mg/kg, we saw a progressive increase in adhesion prevention from those two doses.
In terms of the different time frames, looking at adhesions with this model specifically, our personal experience and data we have collected in the past have shown that when we look at adhesion formation beyond 7 days, we haven't really seen much of a difference in terms of severity. The same is true for tPA. In fact, what we have seen in previous studies is that tPA immediately post-op, at least within the rat, drops significantly and hits its nadir at approximately 24 hours and following that period of time begins to slowly rise back towards normal levels. So we chose that simply because it gives us a general idea of what the fibrinolytic activity within the abdomen is doing at its worst case scenario. We have also shown that giving the drug at 24 hours, we can alter that fibrinolytic activity.
And the final question, in terms of the soluble and gel forms of various barrier compounds, I am not firmly sure as to how far the various companies have progressed in terms of getting that approved within the U.S. But some of the implications which it may convey are that currently some of the biggest limitations of using HA/CMC barriers involve its actual application. It is a brittle, stiff material. It is difficult to use in certain cases such as laparoscopy, and I think that progressing to more of a gel type of device would improve its utility.
This work was supported in part, by the Smithwick Endowment Fund to the Department of Surgery at Boston University School of Medicine.
Rights and permissions
About this article
Cite this article
Lim, R., Morrill, J.M., Lynch, R.C. et al. Practical Limitations of Bioresorbable Membranes in the Prevention of Intra-Abdominal Adhesions. J Gastrointest Surg 13, 35–42 (2009). https://doi.org/10.1007/s11605-008-0724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0724-3