Abstract
Introduction
Pancreatic fistula is a major source of morbidity after distal pancreatectomy (DP). We reviewed 462 consecutive patients undergoing DP to determine if the method of stump closure impacted fistula rates.
Methods
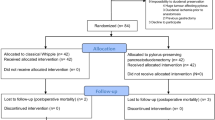
A retrospective review of clinicopatologic variables of patients who underwent DP between February 1994 and February 2008 was performed. The International Study Group classification for pancreatic fistula was utilized (Bassi et al., Surgery, 138(1):8–13, 2005).
Results
The overall pancreatic fistula rate was 29% (133/462). DP with splenectomy was performed in 321 (69%) patients. Additional organs were resected in 116 (25%) patients. The pancreatic stump was closed with a fish-mouth suture closure in 227, of whom 67 (30%) developed a fistula. Pancreatic duct ligation did not decrease the fistula rate (29% vs. 30%). A free falciform patch was used in 108 patients, with a fistula rate of 28% (30/108). Stapled compared to stapled with staple line reinforcement had a fistula rate of 24% (10/41) vs. 33% (15/45). There is no significant difference in the rate of fistula formation between the different stump closures (p = 0.73). On multivariate analysis, BMI > 30 kg/m2, male gender, and an additional procedure were significant predictors of pancreatic fistula.
Conclusions
The pancreatic fistula rate was 29%. Staplers with or without staple line reinforcement do not significantly reduce fistula rates after DP. Reduction of pancreatic fistulas after DP remains an unsolved challenge.

Similar content being viewed by others
References
Grobmyer SR, Pieracci FM, Allen PJ, Brennan MF, Jaques DP. Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg 2007;204(3):356–364. doi:10.1016/j.jamcollsurg.2006.11.017.
Takeuchi K, Tsuzuki Y, Ando T, et al. Distal pancreatectomy: is staple closure beneficial? ANZ J Surg 2003;73(11):922–925. doi:10.1046/j.1445-2197.2003.02821.x.
Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138(1):8–13. doi:10.1016/j.surg.2005.05.001.
Rodriguez JR, Germes SS, Pandharipande PV, et al. Implications and cost of pancreatic leak following distal pancreatic resection. Arch Surg 2006;141(4):361–365. doi:10.1001/archsurg.141.4.361(Discussion 6).
Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg 1999;229(5):693–698. doi:10.1097/00000658-199905000-00012(Discussion 8–700).
Thaker RI, Matthews BD, Linehan DC, Strasberg SM, Eagon JC, Hawkins WG. Absorbable mesh reinforcement of a stapled pancreatic transection line reduces the leak rate with distal pancreatectomy. J Gastrointest Surg 2007;11(1):59–65. doi:10.1007/s11605-006-0042-6.
Jimenez RE, Mavanur A, Macaulay WP. Staple line reinforcement reduces postoperative pancreatic stump leak after distal pancreatectomy. J Gastrointest Surg 2007;11(3):345–349. doi:10.1007/s11605-006-0034-6.
Truty MJSM, Que FG. Decreasing pancreatic leak after distal pancreatectomy:saline-coupled radiofrequency ablation in a porcine model. J Gastrointest Surg 2007;11(8):998–1007. doi:10.1007/s11605-007-0180-5.
Kleeff J, Diener MK, Z’Graggen K, et al. Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 2007;245(4):573–582. doi:10.1097/01.sla.0000251438.43135.fb.
Fahy BN, Frey CF, Ho HS, Beckett L, Bold RJ. Morbidity, mortality, and technical factors of distal pancreatectomy. Am J Surg 2002;183(3):237–241. doi:10.1016/S0002-9610(02)00790-0.
Pannegeon V, Pessaux P, Sauvanet A, Vullierme MP, Kianmanesh R, Belghiti J. Pancreatic fistula after distal pancreatectomy: predictive risk factors and value of conservative treatment. Arch Surg 2006;141(11):1071–1076. doi:10.1001/archsurg.141.11.1071(Discussion 6).
Ridolfini MP, Alfieri S, Gourgiotis S, et al. Risk factors associated with pancreatic fistula after distal pancreatectomy, which technique of pancreatic stump closure is more beneficial? World J Gastroenterol 2007;13(38):5096–5100.
Lorenz U, Maier M, Steger U, Topfer C, Thiede A, Timm S. Analysis of closure of the pancreatic remnant after distal pancreatic resection. HPB Oxf 2007;9(4):302–307. doi:10.1080/13651820701348621.
Sierzega M, Niekowal B, Kulig J, Popiela T. Nutritional status affects the rate of pancreatic fistula after distal pancreatectomy: a multivariate analysis of 132 patients. J Am Coll Surg 2007;205(1):52–59. doi:10.1016/j.jamcollsurg.2007.02.077.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussion
Pancreatic Fistula Rates After 462 Distal Pancreatectomies: Staplers Do Not Decrease Fistula Rates
Michael G. Sarr, M.D. (Rochester, MN): Dr. Ferrone, why aren’t we smarter? We ought to be able to solve this problem of leaks, but it is consistent across the board, isn’t it? So I have three questions.
There must be some up front bias in your study. For a thick gland, I doubt that some of your surgeons would be willing to put a stapler across. Why don’t you comment on that. Second, there are some new techniques, such as Tissuelink®, and there is an experimental study that supports that. Is octreotide of any benefit? And third, why did you leave a drain?
Cristina R. Ferrone, M.D. (Boston, MA): To answer your first question, I think that there is definitely a bias, and we have actually only been using the Seamguard for the last two years. So there is some bias there, but most of those numbers are within the last two years. But it is true, when you put the stapler across and the pancreas is very thick and you feel the staples are just going to rip through, we tend to switch over and perform the fishmouth closure technique. We stratified by length, width, and thickness of the pancreas based on the pathologic specimen and weren't able to find any cutoff which predicted an increased risk of pancreatic fistula, which we were very surprised at. We were hoping to find a thickness cutoff that would indicate you should not be doing this or that, but unfortunately, we did not.
In terms of the second point, I think you are absolutely right. I think Dr. Trudy from your institution has a wonderful model within the pig model, and now has some patient data, suggesting that the tissue link actually will be a method which should be prospectively tried to see if that can actually decrease the fistula rate.
In terms of octreotide, I think you probably know better than anyone, having led the pancreatic study group which included a combination of distal pancreatectomies, middle pancreatectomies, and Whipples, and unfortunately octreotide wasn't able to significantly decrease the fistula rates. Based on the data from the trial you led we have not been that aggressive about using it at our institution, at least recently, because of that data.
And your third question?
Dr. Sarr: The drain.
Dr. Ferrone: I think the thought is that just because you don’t know it (the pancreatic fistula) is there doesn’t mean it is not there and therefore leaving a drain we at least consider somewhat safer. You can treat the patient maybe a little bit more aggressively and prevent them from coming back with fevers and abscesses and having to get an interventional radiology drain.
L. William Traverso, M.D. (Seattle, WA): Christina, very clearly presented.
You presented the A leak and B leak rates overall but you didn’t present A and B for each of the types of techniques that you used. I wonder if you did that and found that that wasn’t helpful? In our experience, by providing a wider spectrum of leak severity grades, you can find that the majority of the leaks were the chemical leaks or A’s and not the clinically significant B’s. I wonder if you might have some important information here?
Finally, one comment is that the original International Study Group’s definition of leak, according to Bassi in 2005 published in Surgery, was not the one that you used in your slide. It has been modified since by other groups in Boston but you did not use that one either. You have modified it even further. When you submit the manuscript please use the actual ISGPS definition the way it was written, or maybe you can’t if you don't have a drain in place to measure drain amylase and volume.
Dr. Ferrone: In terms of that first question, we did actually do the subset analysis, and we compared A versus B and C, to compare clinically low impact versus the clinically high impact fistulas for all the different types of stump closure, and unfortunately we weren’t able to find a difference.
I presented the ISGPF classification copied out of the text of the paper in 2005 by Dr. Bassi. Based on the ISGPF classification we utilized the grade A definition, to define a grade A fistula. And so we did not modify that in the sense that the clinical A classification was defined as no change in the managementand so for us the change in management would have been to leave a drain for more than five days.
Dr. Traverso: I like your modification, by the way, but, for the record: if we are all going to use the same definition, we should use it. The ISGPS definition is currently undergoing some clarification.
Roger G. Keith, M.D. (Saskatoon, SK, Canada): Do you have from your database any information on proximal duct status or proximal disease, which will likely contribute to your fistula rate?
Dr. Ferrone: We, unfortunately, do not. Not all of the patients had good MRCP's or CT scans that we could review to be able to evaluate that proximal duct.
Rights and permissions
About this article
Cite this article
Ferrone, C.R., Warshaw, A.L., Rattner, D.W. et al. Pancreatic Fistula Rates After 462 Distal Pancreatectomies: Staplers Do Not Decrease Fistula Rates. J Gastrointest Surg 12, 1691–1698 (2008). https://doi.org/10.1007/s11605-008-0636-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0636-2