Abstract
Introduction
The utility of laparoscopic Nissen fundoplication in the treatment of laryngopharyngeal reflux symptoms remains controversial. We hypothesized that a carefully selected population with these symptoms would benefit from antireflux surgery.
Materials and Methods
Sixty-one consecutive patients have undergone antireflux surgery for laryngopharyngeal reflux at a single institution. Preoperative evaluation including upper endoscopy, laryngoscopy, and 24-h ambulatory pharyngeal pH probe monitoring confirmed the diagnosis. Patients completed two validated symptom assessment instruments preoperatively and at multiple time points postoperatively.
Results
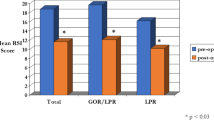
Patients were followed for up to 3 years with a mean follow-up of 15.2 months. A significant improvement in reflux symptom index score (preoperative = 31.5 ± 7.4 vs 3 years = 12.4 ± 10.9, p < 0.01), laryngopharyngeal reflux health-related quality of life overall score (preoperative = 55.0 ± 26.0 vs 3 years = 11.3 ± 13.9, p < 0.01), and symptom domain scores (voice, cough, throat clearing, and swallowing) occured within 1 month of surgery and remained improved over the course ofthe study.
Conclusion
Laparoscopic Nissen fundoplication is effective in relieving the symptoms of laryngopharyngeal reflux in a carefully selected patient population. Benefits are seen within 1 month of surgery and persist for at least 3 years.






Similar content being viewed by others
References
Papasavas PK, Keenan RJ, Yeaney WW, Caushaj PF, Gagné DJ, Landreneau RJ. Effectiveness of laparoscopic fundoplication in relieving the symptoms of gastroesophageal reflux disease (GERD) and eliminating antireflux medical therapy. Surg Endosc 2003;17:1200–1205.
Desai KM, Soper NJ. Laparoscopic Nissen fundoplication. In: In Soper NJ, Swanstrom LL, Eubanks WS, editors. Mastery of Endoscopic and Laparoscopic Surgery. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 193–203.
Ahmad I, Batch AJG. Acid reflux management: ENT perspective. J Laryngology & Otology 2004;118:25–30.
Spivak H, Smith CD, Phichith A, Galloway K, Waring JP, Hunter JG. Asthma and gastroesophageal reflux: Fundoplication decreases need for systemic corticosteriods. J Gastrointest Surg 1999;3:477–482.
Copper MP, Smit CF, Stanojcic LD, Devriese PP, Schouwenburg PF, Mathus-Vliegen LMH. High incidence of laryngopharyngeal reflux in patients with head and neck cancer. Laryngoscope 2000;110:1007–1011.
Carrau RL, Khidr A, Gold KF, Crawley JA, Hillson EM, Koufman JA, Pashos CL. Validation of a quality-of-life instrument for laryngopharyngeal reflux. Arch Otolaryngol Head Neck Surg 2005;131:315–320.
Nord JH. Extraesophageal symptoms: What role for the proton pump inhibitors? Am J Med 2004;117:56S–62S.
Oelschlager BK, Eubanks TR, Oleynikov D, Pope C, Pellegrini CA. Symptomatic and physiologic outcomes after operative treatment for extraesophageal reflux. Surg Endosc. 2002;16:1032–1036.
Duffy JP, Maggard M, Hiyama DT, Atkinson JB, McFadden DW, Ko CY, Hines OJ. Laparoscopic Nissen fundoplication improves quality of life in patients with atypical symptoms of gastroesophageal reflux. Am Surgeon 2003;69:833–838.
Wright RC, Rhodes KP. Improvement of laryngopharyngeal reflux symptoms after laparoscopic Hill repair. Am J Surg. 2003;185:455–461.
Farrell TM, Richardson WS, Trus TL, Smith CD, Hunter JG. Response of atypical symptoms of gastro-oesophageal reflux to antireflux surgery. Br J Surg 2001;88:1649–1652.
Chen RYM, Thomas RJS. Results of laparoscopic fundoplication where atypical symptoms coexist with oesophageal reflux. ANZ J Surg 2000;70:840–842.
Belafsky PC, Postma GN, Koufman JA. Laryngopharyngeal reflux symptoms improve before changes in physical findings. Laryngoscope 2001;111:979–981.
Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the Reflux Symptom Index (RSI). J Voice 2002;16:274–277.
Oelschlager BK, Chang L, Pope CE, Pellegrini CA. Typical GERD symptoms and esophageal pH monitoring are not enough to diagnose pharyngeal reflux. J Surg Res 2005;128:55–60.
Oelschlager BK, Eubanks TR, Maronian N, Hillel A, Oleynikov D, Pope CE, Pellegrini CA. Laryngoscopy and pharyngeal pH are complementary in the diagnosis of gastroesophageal–laryngeal reflux. J Gastrointest Surg 2002;6:189–194.
Dore MP, Pedroni A, Pes GM, Maragkoudakis E, Tadeu V, Pirina P, Realdi G, Delitala G, Malaty HM. Effect of antisecretory therapy on atypical symptoms in gastroesophageal reflux disease. Dig Dis Sci 2007;52:463–468.
So JBY, Zeitels SM, Rattner DW. Outcomes of atypical symptoms attributed to gastroesophageal reflux treated by laparoscopic fundoplication. Surgery 1998;124:28–32.
Belafsky PC, Postma GN, Amin MR, Koufman JA. Symptoms and findings of laryngopharyngeal reflux. Ear Nose Throat J 2002;81(S2):10–13.
Munoz JV, Herreros B, Sanchiz V, Amoros C, Hernandez V, Pascual I, Mora F, Minguez M, Bagan JV, Benages A. Dental and periodontal lesions in patients with gastro-oesophageal reflux disease. Dig Liver Dis 2003;35:461–467.
Oelschlager BK, Barreca M, Chang L, Oleynikov D, Pellegrini CA. Clinical and pathologic response of Barrett’s esophagus to laparoscopic antireflux surgery. Ann Surg 2003;238:458–466.
Maldonado A, Diederich L, Castell DO, Gideon RM, Katz PO. Laryngopharyngeal reflux identified using a new catheter design: Defining normal values and excluding artifacts. Laryngoscope 2003;113:349–355.
Westcott CJ, Hopkins MB, Bach K, Postma GN, Belafsky PC, Koufman JA. Fundoplication for laryngopharyngeal reflux disease. J Am Coll Surg 2004;199:23–30.
Novitsky YW, Zawacki JK, Irwin RS, Hussey VM, Callery MP. Chronic cough due to gastroesophageal reflux disease: Efficacy of antireflux surgery. Surg Endosc 2002;16:567–571.
Greason KL, Miller DL, Deschamps C, Allen MS, Nichols FC, Trastek VF, Pairolero PC. Effects of antireflux procedures on respiratory symptoms. Ann Thorac Surg 2002;73:381–385.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussion
C. Daniel Smith, M.D. (Jacksonville, FL): I want to thank the authors for inviting me to comment on this work and providing the manuscript in advance and also congratulate you. This is a difficult patient population; it is a very difficult diagnosis, and probably the hardest of all is drilling down on the outcomes and making sense of outcomes. You have done a good job at trying to achieve that. However, I am going to challenge you on a couple of things, and I have four questions for you.
First relates to the definition of your patient population. Sixty percent of your patients had both LPR and GERD symptoms, which are typical GERD symptoms. My question is, did you look at the outcomes of those with LPR only? You have stated that LPR was the primary indication for surgery, but did you actually isolate out those patients who had only LPR and look at their outcomes, and if not, why not?
The second question is how do you explain or at least offer some comments about the significant improvement at 1 month, because that is surprising. Most of us caution these patients that it is going to take months and months before they are going to achieve any significant change in their symptoms because of the chronic inflammatory changes associated with the larynx and the vocal cords. I was really struck that you had such dramatic and sustained improvement starting as early as 1 month.
Third, are there any data or any thoughts on PPIs? They were sort of absent from your whole talk, and most of us will use response to PPIs as a predictor of outcome, at least for typical GERD symptoms. In addition, what about continued use of PPIs postoperatively. You did not tell us anything about how many of these patients still needed any PPIs at all and if none of them are needing PPIs, which is a pretty remarkable outcome, that should be included.
And finally, what is your definition of success? QoL, quality of life, is a great outcome, but it is very difficult to interpret quality of life without a control group, and you did not provide us a control. Therefore, I am not sure we can rely simply on quality of life. There is another way to interpret your data, and that is that 35% of patients failed to normalize their LPR. They had improvement, but they failed to normalize. This, without any objective data on pH postoperatively or PPI use postoperatively could lead to a completely different conclusion; these patients are not doing as well as you would like with 35% of patients failing this approach and perhaps not such a favorable outcome.
I look forward to your comments, and again, thanks for the chance to comment on this paper.
Robert A. Catania, M.D. (Baltimore, MD): Thank you very much, Dr. Smith. To answer the questions, separation of the pure LPR versus the mixed population, did we perform a statistical analysis of the LPR only group? It could have been done very quickly, but we did not analyze the data that way. To drill down on differences between the two groups, what we did instead was a chi-squared analysis. We did expect that there would be a difference, as it has been suggested in the past that there is a difference. In our study, we found that both groups responded equally well to surgery.
The demonstrated improvement at the 1 month time point, I agree, was also somewhat surprising, particularly with vocal symptoms. Some symptom clusters have been shown in the past to respond quickly, particularly things like coughing and choking episodes, and you would expect that when you stop the reflux that is causing the coughing and choking, the symptoms would similarly stop. Previously, it has been shown that it takes a couple of months for the vocal changes to improve, but we found in our population that that was not the case.
Now, our results may be partially due to a selection bias in that when we designed the study, we wanted to see if this was an intervention that was going to help people early in the diagnosis of LPR to answer the question should we treat them with antireflux surgery early in the course of the disease. We specifically excluded people who had structural damage to their larynx, as we were using symptom scores to quantify success. We excluded people who had previous tracheostomies and people who had previous reconstructive surgery. There were a few people who had had polyps or granulation tissue removed from their vocal cords. I cannot give you a specific number on that. I think that may be why we saw an improvement so much faster than previously reported, because in earlier studies they did not exclude those patients with structural changes. Our thought was if there are already significant structural changes of the larynx, we would not expect them to symptomatically improve, which is why we excluded them from our population.
In terms of PPIs, we have added questions about PPI therapy to our questionnaire that goes out now, but for the first year of collection, we did not have any of that data. It may be a reasonable thing to go back and retrospectively try to collect that, but I do not have that information for the entire population, and therefore I did not include it in the analysis.
Finally, I present the definition of success. I agree that 35% failed to normalize, but the RSI is a dynamic index, and when you look at it, control patients in the early studies do not have a definite score of 0 or 5. Their scores covered a range between 8 and 15. A score below 13 was chosen to be the definition of normal because that score included 75% of normal patients. Some of the patients in our study that fall into the 13 to 19 range I think are probably normal. We just are bound by the definition reported by previous authors.
Rights and permissions
About this article
Cite this article
Catania, R.A., Kavic, S.M., Roth, J.S. et al. Laparoscopic Nissen Fundoplication Effectively Relieves Symptoms in Patients with Laryngopharyngeal Reflux. J Gastrointest Surg 11, 1579–1588 (2007). https://doi.org/10.1007/s11605-007-0318-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0318-5