Abstract
Background
Fractures and dislocations of the proximal interphalangeal (PIP) joint of the fingers are among the most common causes of injury in the hand. Objective assessment of the kinematic alterations occurring when the supporting structures are disrupted is critical to obtain a more accurate indication of joint stability.
Methods
An in vitro cadaver model of the hand was used to evaluate the kinematics of the PIP joint in the finger during active unrestrained flexion and extension. The kinematics of the PIP joint following progressive disruption of the main supporting structures was measured using an optical tracking system and compared with those in the intact joint.
Results
Flexion of the intact PIP joint was associated with joint compression, volar displacement, and rotational movements. Release of the main soft-tissue stabilizers and 30 % of volar lip disruption resulted in substantial alteration of several kinematic variables. The normalized maximum dorsal/volar translation was 0.1 ± 1.3 % in the intact group and 14.4 ± 11.3 % in the injured joint.
Conclusions
In the intact PIP joint, rotations and translation are strongly coupled to the amount of joint flexion. Gross instability of the PIP joint occurs when disruption of the collateral ligaments and volar plate is accompanied by resection of at least 30 % of volar lip of the middle phalanx. Collateral ligament injuries, volar plate injuries alone, and fractures at the volar base of the middle phalanx that involve less than 30 % of the articular surface are unlikely to result in gross instability and may be managed effectively with non-operative treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proximal interphalangeal (PIP) joint is the articulation exhibiting the largest range of motion in the hand [2, 14]. This mobility accounts for 85 % of the grasping capabilities of the fingers, while the distal interphalangeal joint provides for the remaining 15 % [11]. Similar to the knee joint, the PIP joint is bicondylar and its articular surfaces contribute to the stability in the frontal plane while permitting larger and almost unrestricted motion in the sagittal plane. The two collateral ligaments provide most of the support to resist ulnar and radial deviating forces, while a thick fibro-cartilaginous structure, i.e., the volar plate, prevents dorsal subluxation by limiting joint hyperextension [8]. Normal motion of the PIP joint requires intact articular surfaces, unimpeded tendon gliding, and integrity of the collateral ligaments and volar plate. Deficiency in any of these structural requirements can lead to loss of finger joint motion and decreased hand function. PIP joint injuries are the most common ligamentous injury to the hand and if left untreated may lead to substantial pain, stiffness, instability, and eventually, arthritis.
Despite their critical contribution to the prehensile capabilities of the hand, the joints in the fingers are commonly assumed to move as simple hinge joints with limited or absent motion outside the sagittal plane. In fact, the shape of the PIP joint resembles that of the knee, in which rotations and translations are well coupled to the amount of sagittal plane rotation [15, 22]. Disruption of any of the structures in the knee joint capsule weakens this coupling and generates instability, which can demonstrate some “hysteresis” of the kinematic variables between the flexion and extension movement [1]. This is defined as the difference in a kinematic parameter (either translation or rotation) between the flexion and the extension. It has not been previously determined if coupled path of motions between relevant kinematic variables can also be observed in the intact PIP joint, and how these are affected by increasing level of joint disruption.
While stereophotogrammetry applied to the kinematics of the interphalangeal joints in vivo is limited by the size of the fingers and intrinsically biased by motion tissue artifacts [18], in vitro testing on cadaveric specimens allows for a more accurate three-dimensional description of interphalangeal joint motion. A magnetic tracking device has been previously used to measure multi-planar motion at the PIP joint in a cadaver model using disarticulated fingers [15]. This model allowed estimation of the influence of the main soft tissues [15] and of joint replacement [16, 21] on the lateral stability of the PIP joint. More recently, lateral fluoroscopy was used to assess dorsal/volar stability of the PIP joint following incremental injury of the volar articular base of the middle phalanx [20]. No in vitro study has, thus far, been conducted on the three-dimensional motion of the PIP joint in the finger using physiological muscle activation in a whole-hand cadaveric model.
The aim of this study was to investigate the three-dimensional kinematics of the PIP joint in vitro during active and unrestrained flexion and extension movements of the finger. In particular, the kinematic coupling between flexion motion and rotations/translations in the intact joint was compared to that in different stages of progressive soft tissue and bony injuries. This data has the potential to help correlate instability of the joint with a pattern of injury that may affect clinical decision making.
Materials and Methods
Specimen Preparation
Six fresh-frozen hands (two left, four right) from six cadavers (77 ± 15 years) were thawed for at least 12 h, and ten fingers (five index, five ring) from these hands were used in the study. According to the power analysis performed during study design, 10 samples were sufficient to achieve 90 % statistical power at 0.05 confidence. Radiographic imaging was obtained to exclude specimens with severe arthritic changes or any pathologic bony lesions. In each tested finger, the proximal end of the flexor digitorum sublimis and profundus tendons were each sutured and attached to a metal wire. Similarly, metal wires were sutured to the tendon of the extensor digitorum communis. These wires were used for controlled tension to be applied to the tendons via a custom jig described below.
Each joint was tested in six different configurations:
-
C1
intact;
-
C2
following release of the two collateral ligaments proximally;
-
C3
C2 and release of the volar plate distally;
-
C4
C3 and 20 % of middle phalanx volar lip resection;
-
C5
C3 and 30 % of middle phalanx volar lip resection;
-
C6
C3 and 50 % of middle phalanx volar lip resection.
The bone was resected using a small oscillating saw. A digital caliper was employed to measure the percentage of bone removed with respect to the total length of the intact articular surface. The percentage of bone resected, on average, measured 19 ± 5 %, 31 ± 5 %, and 48 ± 3 % respectively in the C4, C5, and C6 group.
Loading Setup
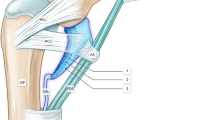
Each hand was clamped to a custom jig and the actuator of a servohydraulic testing machine (MTS 851, MTS Corporation, Minneapolis, MN) was employed to apply tension to the extensor tendons in order to reproduce extension of the PIP joint (Fig. 1, left). The actuator was set to move in displacement control at 0.5 mm/s until maximum extension of the joint was achieved. Data from a load cell (MTS, loading range 0–890 N) in line with the actuator were employed to stop, hold for 3 s, and invert the motion of the actuator when the tension in the wire reached the desired threshold. The latter was determined for each specimen before each testing session and ranged between 15 and 30 N. PIP flexion was achieved by gravity pull of two 5-N passive weights attached to the wires of each flexor tendon accompanied by gradual release of the tension in the extensor tendons [9]. Tension applied to the flexor tendons was consistent with in vivo data on active free flexion of the fingers [3, 9, 17, 19].
On the left cadaveric hand held in the testing jig for application of the flexion/extension movement to the PIP joint of the finger. An upward movement of the actuator of the servohydraulic machine applies tension to the tendon of the extensor muscle. PIP joint flexion is achieved by application of a hanging weight to the flexor tendon(s). A cluster of three active infra-red markers is bone-pinned to the proximal and middle phalanx for motion analysis. On the right rigid pins fixating the clusters of infra-red markers to the phalangeal bones bi-cortically are visible in this fluoroscopic view of one of the specimens
Kinematic Protocol
A rigid plate, fitted with three infra-red sensors, was pinned into the lateral side of the shaft of each proximal and middle phalanx of the tested digit (Fig. 1, right). A motion capture system (Optotrak Certus, Northern Digital Inc, Waterloo, Ontario, Canada) was employed to track the motion of the sensors during full extension/flexion cycles of the joint. Anatomical landmarks were digitized and employed to establish local reference frames on the proximal and middle phalanx [23].
PIP joint rotations and translations (Fig. 2) were calculated according to an established convention [5]. Translations were normalized to the dorsal/volar length of the articular surface at the base of the middle phalanx (8.1 ± 0.6 mm across all specimens) to account for interspecimen dimensional differences. We defined instability as loss of joint concentricity as displayed by translation of the middle phalanx relative to the proximal phalanx (hinging motion) larger than what recorded in the intact joint. For each digit, neutral position of the PIP joint (0 degree of rotation; 0 mm of translation) was assumed to be that of maximum extension achieved in the intact joint. Before each data acquisition, three precondition flexion/extension cycles were conducted on each specimen. Five motion cycles were performed on each specimen in each testing configuration, for a total of 50 acquisitions across all digits.
Diagram of the bones and joints in the finger and convention adopted for direction of rotations and translations at the PIP joint. Anatomical landmarks P1, P2, and P3, and M1, M2, and M3 were used to establish the reference frame, respectively, on the proximal and middle phalanx. MCP, PIP, and DIP are the metacarpo-phalangeal, the proximal interphalangeal and the distal interphalangeal joint, respectively
Data Analysis
In the intact joint configuration, coupled path of motions were investigated by calculating the determination coefficient (R 2) of translations and out-of-sagittal plane rotations with respect to the flexion angle. In the injured configurations, loss of kinematic coupling between sagittal plane and out-of-sagittal plane rotations and translations were estimated by measuring the hysteresis of each kinematic variable during a full flexion/extension cycle. At different flexion angles, hysteresis was determined as the difference in a kinematic parameter (either translation or rotation) between the flexion and the extension movement. The mean and the maximum hysteresis over the whole flexion/extension cycle were recorded and averaged across trials. Mann-Whitney nonparametric test was used to assess differences in the kinematic variables and hysteresis between each injury level group and the intact configuration. In the present paper, differences between groups in the kinematic parameters were considered significant for p < 0.05.
Results
The setup and loading protocol employed allowed for a consistent flexion/extension range of motion. An average ROM of 84° ± 17° was achieved over all specimens and trials. The ROM, minimum, and maximum of the measured kinematic variables in the six PIP joint configuration groups are shown in Table 1.
In the intact PIP joint, coupled path of motions were observed between sagittal plane and out-of-sagittal plane rotations and translations. The median coefficient of determination (R 2) between sagittal-plane and out-of-sagittal plane rotations was 0.84, and 0.91 for radial/ulnar and internal/external rotation. With respect to PIP joint translations, R 2 was 0.61, 0.93, and 0.92 with respect to radial/ulnar, volar/dorsal, and compression/distraction, respectively.
In the index finger, flexion was associated with some degrees of pronation and ulnar deviation whereas radial deviation was observed in the ring finger (Fig. 3). Both index and ring fingers showed volar displacement and compression during flexion (Fig. 4; Table 1).
In the intact PIP joint, translation between middle and proximal phalanx in the three anatomical planes during flexion. The plots show the mean values (±SD) of the radial/ulnar (top), volar/dorsal (middle), and compression/distraction (bottom) translations normalized to the joint dimension, across 50 flexion trials. Positive values are associated to: ulnar translation; dorsal translation, and distraction
The release of the two collateral ligaments (i.e., in C2) did not significantly alter the kinematics of the PIP joint (p < 0.05). The kinematic variables were not statistically different (p > 0.05) from those in the intact joint (Table 1). A small, but significant (p > 0.05) increase of maximum dorsal translation was detected following the release of the volar plate (C3). This increase was even more evident at 20 % disruption of the volar base of the middle phalanx (C4). The maximum dorsal translation was 0.1 ± 1.3 % in the intact joint and 3.8 ± 8.6 % in C4 (p < 0.05). This level of joint disruption was also accompanied by greater ROM in radial/ulnar translation (5.5 ± 2.6 %) compared to that in the intact joint (4.1 ± 1.8 %, p < 0.05). Increased radial/ulnar translation and maximum dorsal translation were also detected after extending the volar base disruption to 30 % of the articular surface (C5). At 50 % of joint disruption (C6) the kinematic variables were very different from those in the intact joint, with significantly (p > 0.05) greater rotations and translations in the frontal and horizontal plane. Moreover, joint instability was detected in 7 out of the 10 specimens, with abrupt modification of the kinematic trajectories at an average of 38° ± 17° of PIP joint flexion. This coincided with gross subluxation of the joints on macroscopic observation.
With the exception of the supination/pronation trajectories in C2, no significant (p < 0.05) increment of the hysteresis was detected until 30 % of joint disruption (Table 2). In C5, the hysteresis of many of the kinematic variables was significantly larger (p > 0.05) than what recorded in the intact joint. For example, the maximum hysteresis of the supination/pronation trajectories was 1.3° ± 0.5° in the intact joint and 3.5° ± 4.2° in C5 (p < 0.05). In C6, all kinematic variables showed larger hysteresis compared to the intact configuration. The maximum hysteresis of the dorsal/volar trajectories was 4.4 ± 2.0 % in the intact joint and 26.8 ± 19.2 % in C6 (p < 0.05; see Fig. 5 for a representative specimen).
Flexion (solid) and extension trajectories (dash) of the dorsal/volar translations in the intact and in the injured PIP joint (C6, 50 % of joint disruption), from a representative specimen. Mean (±SD) curves were determined across five flexion/extension cycles. Increased hysteresis, i.e., distance between flexion and extension trajectories, is evident with increased level of joint disruption
Discussion
A cadaver model of the entire hand was used to get a better insight of the kinematics of the PIP joint in the finger. While this articulation is commonly assumed to move as a simple hinge joint, more complex multi-planar rotations have been shown to occur during flexion/extension motion. However, the relationship between sagittal plane rotation and frontal/transverse plane rotations and translations has never been investigated. Moreover, the extent to which this kinematic coupling is affected by disrupting the main stabilizing structures could provide valuable information in the diagnosis of PIP joint injuries.
In the intact configuration, and in accordance with clinical observations, all fingers showed small but consistent amount of compression and volar translation with flexion of the PIP joint. Strong correlations were found between flexion/extension movement and rotations/translations in three anatomical planes, with exception of the radial/ulnar translation. Despite the complex three-dimensional motion occurring during unrestrained active flexion/extension, the PIP joint showed a single degree-of-freedom, in that the extent and direction of the rotations and translations are strongly related to the sagittal plane rotation.
Additionally, while the small sample size does not allow us to draw any strong conclusions on digit-specific kinematic patterns, this study supports the previously reported association between finger flexion and ulnar deviation in the index finger [15], whereas radial deviation was observed in the ring. These small angulations bring the digits toward the middle finger and support the visual observation of all digits aligning with the scaphoid tuberosity in composite flexion. Differences in the geometry of the condyles between radial and ulnar sides [4, 10] may account for the opposite frontal plane rotation observed in our study between index and ring finger.
We chose to release the collateral ligaments proximally and the volar plate distally in order to mimic their typical avulsion sites in the clinical setting. According to our results, the kinematics of the PIP joint during unrestrained active flexion is not significantly affected by the release of the collateral ligaments (p < 0.05). Similarly, the kinematic patterns in flexion were analogous to those in extension, i.e., the hysteresis parameters were not significantly different from those recorded in the intact joint (p < 0.05). This is consistent with the clinical practice of collateral ligament excision in the setting of contracture being well tolerated. It has been previously shown that the collateral ligaments and the volar plate tighten to resist varus/valgus moments and dorsal dislocation forces [15]. Such loading configurations were not tested in this investigation; rather, focus was given to providing an accurate description of the PIP joint kinematics during physiologic free flexion/extension motion in a functional arch. Nonetheless, a small incremental increase of dorsal translation (1.0 ± 1.8 %) following the release of the volar plate was confirmed by the present study. However, this was not clinically notable and did not result in joint subluxation.
Increased dorsal translation was evident following the resection of 20 % of the articular surface, which was also associated with greater motion in the radial/ulnar direction. This trend for kinematic alteration of PIP joint motion continued after resecting 30 % of articular surface, and was also associated with larger hysteresis of many of the kinematic trajectories. The increase of dorsal translation was progressively more evident at 50 % of joint disruption. This pattern is consistent with the in vivo common scenario of a PIP dorsal subluxation following injury to the bony buttress of the volar lip in the middle phalanx [7]. Moreover, this in vitro study appears to support those clinical findings reporting onset of PIP joint instability to occur when approximately 30 % of the volar base is involved [6].
With sectioning of the volar plate, all of the kinematic variables were statistically unchanged, except for subtle instability represented by a small increase of dorsal translation. It is generally thought that when the volar fragment of the base of the middle phalanx comprises less than 40 % of the joint surface, the collateral ligaments attach to the dorsal, rather than the volar fragment, which renders the joint stable after reduction. The number 40 % is a rough estimate based on clinical experience and anatomic study of collateral ligament insertion, and actual stability may vary. In our model, the disruption occurred through both the volar base and the collateral ligaments, and yet minimal translation occurred when the volar base fragment was 20 % of the articular surface (C4), and instability was evident with fragment size of 30 % and above (C5, C6). Therefore, it appears that the amount of bony congruence provided by the buttressing effect of the volar margin of the middle phalanx that partially covers the proximal phalangeal condyles is key to PIP joint stability. The soft-tissue stabilizers have less importance in maintaining joint stability, even if the ligament-box complex is disrupted in two planes (C3).
An in vitro biomechanical investigation of PIP joint stability, based on fluoroscopic imaging, reported mean dorsal translation of the middle phalanx in relation to the proximal of 0.2, 0.8, and 3.2 mm, respectively, at 20, 40, and 60 % of volar bony defect [20]. This is consistent with the pattern of dorsal translation recorded here of 0.3 (i.e., 3.8 % of 8.1 mm), 0.6, and 1.2 mm at 20, 30, and 50 % of volar defect, respectively. Additionally, the average subluxation angle of 38° ± 17° detected in the 50 % group is within the values reported by Tyser et al. (14° in the 40 % group, and 67° in the 60 % group), thus further supporting the hypothesis that dorsal instability would be apparent at a higher degree of PIP joint extension as the volar middle phalanx articular fragment size increases [20].
The present study has some limitations. We elected to use the serial sectioning method, in which release of the volar plate was followed by progressive osteotomy whereas in vivo fractures of the middle phalanx base are usually attached proximally to the volar plate and some amount of the collateral ligamentous complex. Additionally, our loading setup aimed at mimicking PIP joint kinematics but could only partially simulate the joint physiological loading. The flexion and extension pull exerted by the main hand extrinsic muscles was replicated here, along with some physiological co-contraction occurring during flexion. However, while it has been shown that intrinsic muscles contribution to PIP joint motion is negligible at least during flexion [12, 13], their action could not be replicated by the current setup.
In conclusion, the release of the collateral ligaments, volar plate, and disruption of 20 % of the articular surface induced subtle joint instability in the dorsal/volar direction during unrestrained flexion/extension, without gross kinematic instability. Further bony resection of the volar base of the middle phalanx resulted in large instability in the PIP joint in multiple planes. While care should be taken in translating the present results into clinical practice, this study has shown that several kinematic parameters were affected by PIP joint disruption. However, the dorsal/volar displacement of the middle phalanx showed the largest correlation to sagittal plane motion and appears to be the best indicator of joint instability.
References
Berdia S, Short WH, Werner FW, Green JK, Panjabi M. The hysteresis effect in carpal kinematics. J Hand Surg [Am]. 2006;31(4):594–600. doi:10.1016/j.jhsa.2005.12.028.
Chiu HY, Su FC, Wang ST, Hsu HY. The motion analysis system and goniometry of the finger joints. J Hand Surg (Br). 1998;23(6):788–91.
Dennerlein JT, Diao E, Mote Jr CD, Rempel DM. Tensions of the flexor digitorum superficialis are higher than a current model predicts. J Biomech. 1998;31(4):295–301.
Dumont C, Albus G, Kubein-Meesenburg D, Fanghanel J, Sturmer KM, Nagerl H. Morphology of the interphalangeal joint surface and its functional relevance. J Hand Surg [Am]. 2008;33(1):9–18. doi:10.1016/j.jhsa.2007.09.001.
Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–44.
Isani A. Small joint injuries requiring surgical treatment. Orthop Clin North Am. 1986;17(3):407–19.
Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg. 1998;23(3):368–80.
Kiefhaber TR, Stern PJ, Grood ES. Lateral stability of the proximal interphalangeal joint. J Hand Surg [Am]. 1986;11(5):661–9.
Kursa K, Lattanza L, Diao E, Rempel D. In vivo flexor tendon forces increase with finger and wrist flexion during active finger flexion and extension. J Orthop Res. 2006;24(4):763–9. doi:10.1002/jor.20110.
Lawrence T, Trail IA, Noble J. Morphological measurements of the proximal interphalangeal joint. J Hand Surg (Br). 2004;29(3):244–9. doi:10.1016/j.jhsb.2004.01.010.
Leibovic SJ, Bowers WH. Anatomy of the proximal interphalangeal joint. Hand Clin. 1994;10(2):169–78.
Long 2nd C. Intrinsic-extrinsic muscle control of the fingers. Electromyographic studies. J Bone Joint Surg Am. 1968;50(5):973–84.
Long C. Intrinsic-extrinsic muscle control of the fingers. Plast Reconstr Surg. 1969;44(1):93.
Mallon WJ, Brown HR, Nunley JA. Digital ranges of motion: normal values in young adults. J Hand Surg. 1991;16(5):882–7.
Minamikawa Y, Horii E, Amadio PC, Cooney WP, Linscheid RL, An KN. Stability and constraint of the proximal interphalangeal joint. J Hand Surg. 1993;18(2):198–204.
Minamikawa Y, Imaeda T, Amadio PC, Linscheid RL, Cooney WP, An K-N. Lateral stability of proximal interphalangeal joint replacement. J Hand Surg. 1994;19(6):1050–4.
Nikanjam M, Kursa K, Lehman S, Lattanza L, Diao E, Rempel D. Finger flexor motor control patterns during active flexion: an in vivo tendon force study. Hum Mov Sci. 2007;26(1):1–10.
Ryu JH, Miyata N, Kouchi M, Mochimaru M, Lee KH. Analysis of skin movement with respect to flexional bone motion using MR images of a hand. J Biomech. 2006;39(5):844–52. doi:10.1016/j.jbiomech.2005.02.001.
Schuind F, Garcia-Elias M, Cooney Iii WP, An K-N. Flexor tendon forces: in vivo measurements. J Hand Surg. 1992;17(2):291–8.
Tyser AR, Tsai MA, Parks BG, Means Jr KR. Stability of acute dorsal fracture dislocations of the proximal interphalangeal joint: a biomechanical study. J Hand Surg [Am]. 2014;39(1):13–8. doi:10.1016/j.jhsa.2013.09.025.
Uchiyama S, Cooney WP, Linscheid RL, Niebur G, An KN. Kinematics of the proximal interphalangeal joint of the finger after surface replacement. J Hand Surg [Am]. 2000;25(2):305–12. doi:10.1067/jhsu.2000.jhsu25a0305.
Wilson DR, Feikes JD, Zavatsky AB, O’Connor JJ. The components of passive knee movement are coupled to flexion angle. J Biomech. 2000;33(4):465–73.
Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–92.
Conflict of Interest
Paolo Caravaggi declares that he has no conflict of interest.
Benhoor Shamian declares that he has no conflict of interest.
Linda Chen declares that she has no conflict of interest.
Linda Uko declares that she has no conflict of interest.
Eitan Melamed declares that he has no conflict of interest.
John T. Capo declares that he has received research support and is a consultant for Synthes Corporation and Wright Medical Technology. He is also a consultant and member of Speakers Panel Integra Life Sciences.
Statement of Human and Animal Rights
This article does not contain any studies with human or animal subjects.
Statement of Informed Consent
This article does not contain any studies with human or animal subjects. No informed consent was needed inthis study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Caravaggi, P., Shamian, B., Uko, L. et al. In vitro kinematics of the proximal interphalangeal joint in the finger after progressive disruption of the main supporting structures. HAND 10, 425–432 (2015). https://doi.org/10.1007/s11552-015-9739-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-015-9739-x