Abstract
Purpose
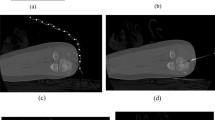
We investigated procedural safety, technical and clinical outcomes of the percutaneous image-guided radiofrequency ablation (PRFA) of intra-articular (IA), intra-articular close to cartilage (IACC), and extra-articular (EA) osteoid osteomas (OO). We proposed a new radiologic classification for osteoid osteoma depending on the degree and location of sclerosis which may correlate with technical failure and/or difficulties.
Material and methods
According to the inclusion criteria, we enrolled consecutive patients who were referred to the investigation center from June 2018 to January 2022. After clinical and CT imaging features were suggestive for the diagnosis of OO, all the patients were treated by percutaneous CT-guided RFA with a standardized technique. Biopsy of the lesion was not performed in all patients. A retrospective analysis was conducted to assess the procedure’s technical, primary clinical, and secondary clinical successes, recurrence rate, and complications. We classified all the OOs according to a new proposed classification of the site and the amount of sclerosis.
Results
A total number of 55 patients were enrolled in our study according to the inclusion criteria. The mean age of the enrolled patients was 24.07 ± 14.71 years (ranges from 7 to 57 years). The M/F ratio was roughly 2:1. The mean follow-up was 20.18 ± 12.60 months (ranges from 2 to 44 months). EA group included 36 patients, IA included 5 and IACC included 14 patients. Technical success was achieved in all cases of IA and IACC groups. Technical success in the EA group was 97.22% (1 technical failure). Primary clinical success was 100%, 92.85%, and 91.66% for IA, IACC, and EA groups, respectively. Accordingly, the recurrence rate was 5.88% in EA, and 7.14% in IACC, while no recurrence occurred in the IA group. No complications occurred. The secondary success rate of the 3 cases of recurrence was 100%.
Conclusions
PRFA proved to be a safe procedure with a high rate of success for OO treatment even in intra-articular lesions in close contact with cartilage. This study showed that the results in terms of technical and clinical success are comparable for IA OO, IACC OO, and EA OO, even if the recurrence rate was higher in EA OO. Our proposed new classification of the degree and location of sclerosis may correlate to technical failure, but further studies with a larger number of patients are needed for validation.





Similar content being viewed by others
Abbreviations
- PRFA:
-
Percutaneous radiofrequency ablation
- CT:
-
Computed tomography
- OO:
-
Osteoid osteoma
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- IA:
-
Intra-articular
- IACC:
-
Intra-articular close to the cartilage
- EA:
-
Extra-articular
References
Noordin S, Allana S, Hilal K, Nadeem N, Lakdawala R, Sadruddin A et al (2018) Osteoid osteoma: contemporary management. Orthop Rev (Pavia) 10(3):108–119
Yuce G, Aytekin N, Eren S, Genç B, Ateş ÖF, Canyiğit M (2020) Is radiofrequency ablation safe and effective in treating osteoid osteomas? A prospective single-center study with atypical cases. J Orthop Surg 28(3):1–7
Bellisari FC, Palumbo P, Masciocchi C, Zoccali C, Barile A, Arrigoni F (2022) Needleless ablation of osteoid osteoma and osteoblastoma: the emergent role of MRgfUS. J Clin Med 11(1):128
Tepelenis K, Skandalakis GP, Papathanakos G, Kefala MA, Kitsouli A, Barbouti A et al (2021) Osteoid osteoma: an updated review of epidemiology, pathogenesis, clinical presentation, radiological features, and treatment option. In Vivo (Brooklyn) 35(4):1929–1938
De Filippo M, Russo U, Papapietro VR, Ceccarelli F, Pogliacomi F, Vaienti E et al (2018) Radiofrequency ablation of osteoid osteoma. Acta Biomed 89:175–185
Arrigoni F, Izzo A, Bruno F, Palumbo P, De Filippo M, Zugaro L et al (2021) Musculoskeletal interventional radiology in the pediatric population: state of the art. Semin Musculoskelet Radiol 25(1):176–183
Arrigoni F, Napoli A, Bazzocchi A, Zugaro L, Scipione R, Bruno F et al (2019) Magnetic-resonance-guided focused ultrasound treatment of non-spinal osteoid osteoma in children: multicentre experience. Pediatr Radiol 49(9):1209–1216
Carneiro BC, Da Cruz IAN, Ormond Filho AG, Silva IP, Guimarães JB, Silva FD et al (2021) Osteoid osteoma: the great mimicker. Insights Imaging [Internet]. https://doi.org/10.1186/s13244-021-00978-8
Singh DK, Katyan A, Kumar N, Nigam K, Jaiswal B, Misra RN (2020) CT-guided radiofrequency ablation of osteoid osteoma: Established concepts and new ideas. Br J Radiol 93(1114):1–12
Filippiadis DK, Velonakis G, Kostantos C, Kouloulias V, Brountzos E, Kelekis N et al (2017) Computed tomography-guided radiofrequency ablation of intra-articular osteoid osteoma: a single centre’s experience. Int J Hyperth 28:670–674
Parmeggiani A, Martella C, Ceccarelli L, Miceli M, Spinnato P, Facchini G (2021) Osteoid osteoma: which is the best mininvasive treatment option? Eur J Orthop Surg Traumatol [Internet]. 31(8):1611–1624. https://doi.org/10.1007/s00590-021-02946-w
Huang AJ (2016) Radiofrequency ablation of osteoid osteoma: difficult-to-reach places. Semin Musculoskelet Radiol 20(5):486–495
Arrigoni F, Bruno F, Gianneramo C, Palumbo P, Zugaro L, Zoccali C et al (2020) Evolution of the imaging features of osteoid osteoma treated with RFA or MRgFUS during a long-term follow-up: a pictorial review with clinical correlations. Radiol Med [Internet]. 125(6):578–584. https://doi.org/10.1007/s11547-020-01134-w
Fiore F, Somma F, D’Angelo R, Tarotto L, Stoia V (2022) Cone beam computed tomography (CBCT) guidance is helpful in reducing dose exposure to pediatric patients undergoing radiofrequency ablation of osteoid osteoma. Radiol Medica [Internet]. 127(2):183–190. https://doi.org/10.1007/s11547-021-01439-4
Esteban Cuesta H, Martel Villagran J, Bueno Horcajadas A, Kassarjian A, Rodriguez CG (2018) Percutaneous radiofrequency ablation in osteoid ostema: Tips and tricks in special scenarios. Eur J Radiol [Internet]. 102(February):169–175. https://doi.org/10.1016/j.ejrad.2018.03.008
Papagelopoulos PJ, Mavrogenis AF, Kyriakopoulos CK, Benetos IS, Kelekis NL, Andreou J et al (2006) Radiofrequency ablation of intra-articular osteoid osteoma of the hip. J Int Med Res 34(5):537–544
Garge S, Keshava SN, Moses V, Chiramel GK, Ahmed M, Mammen S et al (2017) Radiofrequency ablation of osteoid osteoma in common and technically challenging locations in pediatric population. Indian J Radiol Imaging 27(1):88–91
Mylona S, Patsoura S, Galani P, Karapostolakis G, Pomoni A, Thanos L (2010) Osteoid osteomas in common and in technically challenging locations treated with computed tomography-guided percutaneous radiofrequency ablation. Skeletal Radiol 39(5):443–449
Filippiadis D, Gkizas C, Kostantos C, Mazioti A, Reppas L, Brountzos E et al (2016) Percutaneous biopsy and radiofrequency ablation of osteoid osteoma with excess reactive new bone formation and cortical thickening using a battery-powered drill for access: a technical note. Cardiovasc Intervent Radiol 39(10):1499–1505
Arrigoni F, Izzo A, Bruno F, Zugaro L, Arrigoni G, Vacca F et al (2021) Could anaesthesia be a key factor for the good outcome of bone ablation procedures? A retrospective analysis of a musculoskeletal interventional centre. Br J Radiol 94(1118):20200937
Ahmed M (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria-A 10-year update. Radiology 273(1):241–260
Sacks D, McClenny TE, Cardella JF, Lewis CA (2003) Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol 14(9):S199-202
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL (2017) Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol 40(8):1141–1146
Germann T, Weber MA, Lehner B, Kintzele L, Burkholder I, Kauczor HU et al (2020) Das intraartikuläre osteoidosteom: mrt-charakteristik und klinisches erscheinungsbild vor und nach radiofrequenzablation im vergleich zum extraartikulären osteoidosteom. Rofo 192(12):1190–1199
Arrigoni F, Spiliopoulos S, de Cataldo C, Reppas L, Palumbo P, Mazioti A et al (2021) A bicentric propensity score matched study comparing percutaneous computed tomography-guided radiofrequency ablation to magnetic resonance-guided focused ultrasound for the treatment of osteoid osteoma. J Vasc Interv Radiol [Internet]. 32(7):1044–1051. https://doi.org/10.1016/j.jvir.2021.03.528
Barile A, Arrigoni F, Bruno F, Palumbo P, Floridi C, Cazzato RL et al (2018) Present role and future perspectives of interventional radiology in the treatment of painful bone lesions. Fut Oncol 14(28):2945–2955
Sgalambro F, Zugaro L, Bruno F, Palumbo P, Salducca N, Zoccali C et al (2022) Interventional radiology in the management of metastases and bone tumors. J Clin Med 11(12):3265
Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ (2003) Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology 229(1):171–175
Irastorza RM, Trujillo M, Martel Villagrán J, Berjano E (2016) Computer modelling of RF ablation in cortical osteoid osteoma: Assessment of the insulating effect of the reactive zone. Int J Hyperth 32(3):221–230
Rosenthal D, Callstrom MR (2012) Critical review and state of the art in interventional oncology: Benign and metastatic disease involving bone. Radiology 262(3):765–780
Filippiadis DK, Velonakis G, Kostantos C, Kouloulias V, Brountzos E, Kelekis N et al (2017) Computed tomography-guided radiofrequency ablation of intra-articular osteoid osteoma: a single centre’s experience. Int J Hyperth 33(6):670–674
Mahnken AH, Tacke JA, Wildberger JE, Günther RW (2006) Radiofrequency ablation of osteoid osteoma: Initial results with a bipolar ablation device. J Vasc Interv Radiol 17(9):1465–1470
Kuhaimi TA, Alenezi G, Alawaji A, Alshaikh M, Bauones S (2021) Intra-articular hip joint osteoid osteoma: Challenging diagnosis and percutaneous radiofrequency ablation treatment. Radiol Case Reports [Internet] 16(11):3315–3320. https://doi.org/10.1016/j.radcr.2021.07.072
Acknowledgements
The researcher (Mostafa Farouk Balbaa) is funded by a full scholarship (mission 2019/2020) from the Ministry of Higher Education of Egypt. The current research work is not funded by the mentioned ministry of Egypt or any other foundation or organization. Authors would like to acknowledge Roberta Aronica for English editing support.
Funding
This study has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest.
Ethical standards
This study was designed as a retrospetive study. Research involving human participants. Institutional Review Board approval was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Spinelli, M.S., Balbaa, M.F., Gallazzi, M.B. et al. Role of percutaneous CT–guided radiofrequency ablation in treatment of intra-articular, in close contact with cartilage and extra-articular osteoid osteomas: comparative analysis and new classification system. Radiol med 127, 1142–1150 (2022). https://doi.org/10.1007/s11547-022-01542-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01542-0