Abstract
Purpose
The purpose of the study was to compare the artefacts produced by different hip prostheses on magnetic resonance imaging (MRI).
Materials and methods
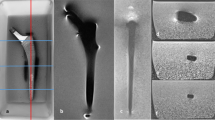
An identical MRI protocol was used to perform a quali-quantitative in vitro evaluation of artefacts caused by different hip prosthetic materials at different field strengths: prosthesis number 1, composed of cobalt–chrome–molybdenum (head and stem); prosthesis number 2, composed of ceramic (head) and titanium (stem); prosthesis number 3, composed of cobalt–chrome (head) and titanium (stem). All prostheses were imaged with both a clinical 1 Tesla (T) (Signa Horizon, General Electrics) and 1.5 T (Achieva, Philips) MRI system, using spin echo (SE) and gradient echo (GRE) sequences: sagittal T1 SE, coronal T2 fast SE (FSE), axial T1 SE, axial T2 FSE, sagittal T2 GRE, axial T2* GRE, coronal T1 GRE, axial T1 GRE. The artefacts produced by each prosthesis were assessed in each sequence at the different field strengths, by measuring the two longest diameters of the artefact in each section and sequence and comparing them to the actual diameters so as to obtain a ratio expressing the effective degree of artefact.
Results
Cobalt–chrome produced the largest artefacts both in SE (1.73 at 1 T and 2.37 at 1.5 T) and GRE sequences (2.8 at 1 T and 3.06 at 1.5 T) followed by titanium (SE, 1.6 at 1 T, 2.13 at 1.5 T; GRE, 2 at 1 T, 2.94 at 1.5 T) and cobalt–chrome–molybdenum (SE, 1.51 at 1 T, 1.67 at 1.5 T; GRE, 2.13 at 1 T and 2.48 at 1.5 T); ceramic produced the smallest artefacts in all sequences (SE, 1.0 at 1 T and 1.18 at 1.5 T; GRE, 1.3 at 1 T and 1.22 at 1.5T). Increasing the magnetic field strength, titanium showed the greatest variations in artefact size, and ceramic the smallest ones.
Conclusions
The composition of prosthetic implants is decisive in determining the quality of MR imaging.







Similar content being viewed by others
References
White LM, Kim JK, Mehta M et al (2000) Complications of total hip arthroplasty: MR imaging—initial experience. Radiology 215:254–262
Manaster BJ (1996) Total hip arthroplasty: radiographic evaluation. Radiographics 16:645–660
Barrett JF, Keat N (2004) Artifacts in CT: recognition and avoidance. Radiographics 24:1679–1691
Aliprandi A, Sconfienza LM, Randelli F et al (2012) Risonanza magnetica dell’anca protesizzata dolorosa: riconoscimento e caratterizzazione delle raccolte fluide periprotesiche e valutazione della riproducibilità interosservatore. Radiol Med 117:85–95
Bakker CJG, Bhagwandien R, Moerland MA et al (1993) Susceptibility artifacts in 2DFT spin-echo imaging: the cylinder model revisited. Magn Reson Imaging 11:539–548
Petersilge CA, Lewin JS, Duerk JL et al (1996) Optimizing imaging parameters for MR evaluation of the spine with titanium pedicle screws. AJR Am J Roentgenol 166:1213–1218
Ebraheim NA, Savolaine ER, Zeiss J et al (1992) Titanium hip implants for improved magnetic resonance and computed tomography examinations. Clin Orthop 275:194–198
Guermazi A, Miaux Y, Zaim S et al (2003) Metallic artefacts in MR imaging: effects of main field orientation and strength. Clin Radiol 58:322–328
Eggers G, Rieker M, Kress B et al (2005) Artefacts in magnetic resonance imaging caused by dental material. MAGMA 18:103–111
Mitchell DG, Cohen MS (2000) Transverse magnetization and T2 contrast. In: Mitchell DG, Cohen MS (eds) MRI principles, 2nd edn. Springer, New York, pp 35–47
Lee MJ, Kim S, Lee SA et al (2007) Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multi-detector CT. Radiographics 27:791–803
Morelli JN, Runge VM, Ai F et al (2011) An image-based approach to understanding the physics of MR artifacts. Radiographics 31:849–866
Tormanen J, Tervonen O, Koivula A et al (1996) Image technique optimization in MR imaging of a titanium alloy joint prosthesis. J Magn Reson Imaging 6:805–811
Suh JS, Jeong EK, Shin KH et al (1998) Minimizing artifacts caused by metallic implants at MR imaging: experimental and clinical studies. AJR Am J Roentgenol 171:1207–1213
Olsen RV, Munk PL, Lee MJ et al (2000) Metal artifact reduction sequence: early clinical applications. Radiographics 20:699–712
Eustace S, Jara H, Goldberg R et al (1998) A comparison of conventional spin-echo and turbo spin-echo imaging of soft tissues adjacent to orthopedic hardware. AJR Am J Roentgenol 170:455–458
Kolind SH, MacKay AL, Munk PL et al (2004) Quantitative evaluation of metal artifact reduction techniques. J Magn Reson Imaging 20:487–495
Cho ZH, Ro YM (1992) Reduction of susceptibility artifact in gradient-echo imaging. Magn Reson Med 23:193–200
Vandevenne JE, Vanhoenacker FM, Parizel PM et al (2007) Reduction of metal artefacts in musculoskeletal MR imaging. JBR-BTR 90:345–349
Ramos-Cabrer P, van Duynhoven JP, Van der Toorn A et al (2004) MRI of hip prostheses using single-point methods: in vitro studies towards the artifact-free imaging of individuals with metal implants. Magn Reson Imaging 22:1097–1103
Jacobs JJ (2012) The utility of MARS MRI in patients with metal-on-metal bearings: commentary on an article by Alister J. Hart, MA, MD, FRCSG (Orth), et al.: “Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional computed tomography and magnetic resonance imaging”. J Bone Joint Surg Am 94(4):e26
Hayter CL, Koff MF, Shah P et al (2011) MRI after arthroplasty: comparison of MAVRIC and conventional fast spin-echo techniques. AJR Am J Roentgenol 197(3):W405–W411
Raphael B, Haims AH, Wu JS et al (2006) MRI comparison of periprosthetic structures around zirconium knee prostheses and cobalt chrome prostheses. AJR Am J Roentgenol 186:1771–1777
Conflict of interest
Elisabetta Panfili, Laura Pierdicca, Luca Salvolini, Luigi Imperiale, Jeffrey Dubbini, Andrea Giovagnoni declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Panfili, E., Pierdicca, L., Salvolini, L. et al. Magnetic resonance imaging (MRI) artefacts in hip prostheses: a comparison of different prosthetic compositions. Radiol med 119, 113–120 (2014). https://doi.org/10.1007/s11547-013-0315-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-013-0315-6