Abstract
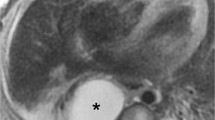
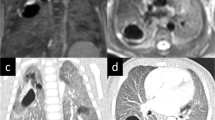
Congenital bronchopulmonary malformations encompass a wide spectrum of pathologies involving the lungs, trachea and bronchi, pulmonary vessels, and oesophagus. These developmental lesions are often isolated, but the association of two or more anomalies is not infrequent. Contrast-enhanced multidetector computed tomography (MDCT), thanks to multiplanar and 3D reconstructions, allows for detailed studies of these malformations, achieving better accuracy compared with conventional techniques such as chest X-ray, fluoroscopy, ventilation and perfusion scintigraphy and ultrasonography. MDCT is characterised by fast data acquisition and does not require sedation in the majority of cases. The main drawbacks of MDCT are the use of ionising radiation and — in many cases —contrast media. Recently, improved CT scanners and optimised CT protocols have made available to children all the benefits of MDCT, thanks to a significant reduction in radiation dose and an improved risk-benefit ratio. The aim of our paper was to evaluate MDCT in children with bronchopulmonary malformations by reporting our experience (about 2,400 studies in 30 months with a 64-slice MDCT scanner) and comparing it with the available literature.
Riassunto
Le malformazioni congenite broncopolmonari rappresentano un ampio spettro di patologie che interessano il parenchima polmonare, il sistema vascolare, le vie aeree centrali e l’esofago. I pazienti affetti presentano quadri malformativi semplici o complessi, rispettivamente caratterizzati da una o più anomalie associate. La tomografia computerizzata (TC) volumetrica multidettetore (MDCT) con mezzo di contrasto permette di analizzare dettagliatamente le strutture toraciche coinvolte nelle malformazioni, con ricostruzioni multiplanari e 3D, con un’accuratezza superiore ad altre indagini tradizionalmente utilizzate tra cui il radiogramma toracico, gli studi fluoroscopici, l’ecografia e la scintigrafia ventilatoria perfusionale. Inoltre la rapidità di acquisizione dei dati consente di evitare nella maggior parte dei casi la sedazione del bambino. Lo svantaggio è rappresentato dall’utilizzo di radiazioni ionizzanti e dalla necessità di somministrare mezzo di contrasto per via endovenosa. Recentemente l’evoluzione tecnologica degli scanner TC e la definizione di protocolli pediatrici dedicati ha permesso una significativa riduzione della dose assorbita, pertanto oggi è possibile usufruire delle potenzialità della MDCT nello studio del torace del bambino con un rapporto rischio-beneficio ragionevolmente vantaggioso. Il nostro articolo si propone di valutare i differenti aspetti dell’impiego della TC sul bambino analizzando la letteratura e confrontandola con l’esperienza personale, unica in Italia: circa 2400 TC del torace in 30 mesi in pazienti compresi tra 1 giorno e 16 anni con un apparecchio a 64 strati.
Similar content being viewed by others
References/Bibliografia
Rydberg J, Buckwalter KA, Caldemeyer KS et al (2000) CT scanning techniques and clinical applications. Radiographics 20:1787–1806
Slovis TL (2000) New horizons in pediatric radiology. Radiology 216:317–320
Brenner D, Elliston C, Hall E, Berdon W (2001) Estimates risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176:289–296
Paterson A, Frush DP, Donnelly LF et al (2001) Helical CT of the body: are settings adjusted for pediatric patients? AJR Am J Roentgenol 176:297–301
Donnelly LF, Emery KH, Brody AS et al (2001) Minimizing radiation dose for pediatric body applications of single-detector helical CT: strategies at a large Children’s Hospital. AJR Am J Roentgenol 176:303–306
FDA (2002) FDA public health notification: reducing radiation risk from computed tomography for pediatric and small adult patients. Pediatr Radiol 32:314–316
Tomà P (2003) Rischio da irradiazione nel bambino: che cosa dobbiamo sapere. Radiol Med 105:83–91
Frush DP (2002) Strategies of dose reduction. Pediatr Radiol 32:293–297
Moore WH, Bonvento M, Olivieri-Fitt R (2006) Comparison of MDCT radiation dose: a phantom study. AJR Am J Roentgenol 187:W498–W502
Brisse H (2006) Guide des procedures radiologiques SFR/INRS. Scanographie Pédiatrique. http://www.sfipradiopediatrie.org. Last access 09/07/2010
Papaioannou G, Young C, Owens CM (2007) Multidetector row CT for imaging the paediatric tracheobronchial tree. Pediatr Radiol 37:515–529
Goske MJ, Applegate KE, Boylan J et al (2008) The ‘Image Gently’ campaign: increasing CT radiation dose awareness through a national education and awareness program. Pediatr Radiol 38:265–269
Boone JM (2006) Multidetector CT: opportunities, challenges, and concerns associated with scanners with 64 or more detector rows. Radiology 241:334–337
Siegel MJ (2003) Multiplanar and three-dimensional multi-detector row CT of thoracic vessels and airways in the pediatric population. Radiology 229:641–650
García-Peña P, Owens CM (2008) Helical multidetector chest CT. In: Lucaya J, Strife JL (eds) Pediatric Chest Imaging. Springer, Berlin Heidelberg New York, pp 47–77
Sena L, Krishnamurthy R, Chung T (2008) Pediatric cardiac CT. In: Lucaya J, Strife JL (eds) Pediatric Chest Imaging. Springer, Berlin Heidelberg New York, pp 361–398
ESUR NSF Guidelines (2007) http://www.esur.org/Nephrogenic_Fibrosis.39.0.html. Last access 09/07/2010
Slovis TL (2003) Children, computed tomography radiation dose, and the as low as reasonably achievable (ALARA) concept. Pediatrics 33:971–972
Kaste SC, Young CW (1995) Safe use of power injectors with central and peripheral venous access devices for pediatric CT. Pediatr Radiol 26:499–501
Ramachandran N, Owens CM (2008) Imaging of the airways with multidetector row computed tomography. Paediatr Respir Rev 9:69–76
Paul JF, Abada HT (2007) Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol 17:2028–2037
Huda W, Scalzetti EM, Levin G (2000) Technique factors and image quality as functions of patient weight at abdominal CT. Radiology 217:430–435
Siegel MJ, Schmidt B, Bradley D et al (2004) Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology 233:515–522
Herzog C, Mulvihill DM, Nguyen SA et al (2008) Pediatric cardiovascular CT angiography: radiation dose reduction using automatic anatomic tube current modulation. AJR Am J Roentgenol 190:1232–1240
Sigal-Cinqualbre AB, Hennequin R, Abada HT et al (2004) Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology 231:169–174
Brody AS, Frush DP, Huda W et al (2007) American Academy of Pediatrics Section on Radiology. Radiation risk to children from computed tomography. Pediatrics 120:677–682
Shrimpton PC, Hillier MC, Lewis MA et al (2005) Doses from computed tomography examinations in the UK: 2003 review. NRPB — W67, NRPB Publications. Available at http://www.hpa.org.uk/radiation/publications/index.html. Last access 09/07/2010
Thomas KE, Wang B (2008) Agespecific effective doses for pediatric MSCT examinations at a large children’s hospital using DLP conversion coefficients: a simple estimation method. Pediatr Radiol 38:645–656
Schertler T, Wildermuth S, Teodorovic N et al (2007) Visualization of congenital thoracic vascular anomalies using multi-detector row computed tomography and two- and three-dimensional post-processing. Eur J Radiol 61:97–119
Panicek DM, Heitzman ER, Randall PA et al (1987) The continuum of pulmonary developmental anomalies. Radiographics 7:747–772
Lee ML, Tsao LY, Chaou WT et al (2002) Revisit on congenital bronchopulmonary vascular malformations: a haphazard branching theory of malinosculations and its clinical classification and implication. Pediatr Pulmonol 33:1–11
Newman B (2006) Congenital bronchopulmonary foregut malformations: concepts and controversies. Pediatr Radiol 36:773–791
Bush A (2001) Congenital lung disease: a plea for clear thinking and clear nomenclature. Pediatr Pulmonol 32:328–337
Yedururi S, Guillerman RP, Chung T et al (2008) Multimodality imaging of tracheobronchial disorders in children. Radiographics 28:e29 DOI 10.1148/rg.e29
Berdon WE (2000) Ring, sling, and other things: vascular compression of the infant trachea updated from the mid century to the millennium—the legacy of Robert E. Gross, MD, and Edward B. D. Neuchauser, MD. Radiology 216:624–632
Lee EY, Boiselle PM, Cleveland RH (2008) Multidetector CT evaluation of congenital lung anomalies. Radiology 247:632–648
Doolittle AM, Mair EA (2002) Tracheal bronchus: Classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg 126:240–243
Panigada S, Sacco O, Girosi D et al (2009) Recurrent severe lower respiratory tract infections in a child with abnormal tracheal morphology. Pediatr Pulmonol 44:192–194
Beigelman C, Howarth NR, Chartrand-Lefebvre C et al (1998) Congenital anomalies of tracheobronchial branching patterns: spiral CT aspects in adults. Eur Radiol 8:79–85
Cardinale L, Ardissone F, Cataldi A et al (2008) Bronchogenic cysts in the adult: diagnostic criteria derived from the correct use of standard radiography and computed tomography. Radiol Med 113:385–394
Berrocal T, Madrid C, Novo S et al (2004) Congenital anomalies of the tracheobronchial tree, lung, and mediastinum: embryology, radiology, and pathology. Radiographics 24:e17 DOI 10.1148/rg.e17
Currarino G, Williams B (1985) Causes of congenital unilateral pulmonary hypoplasia: a study of 33 cases. Pediatr Radiol 15:15–24
Ellis K (1991) Developmental abnormalities in the systemic blood supply to the lungs. AJR Am J Roentgenol 156:669–679
Beerman LB, Oh KS, Park SC (1983) Unilateral pulmonary vein atresia: clinical and radiographic spectrum. Pediatr Cardiol 4:105–112
Stocker JT, Madewell JE, Drake RM (1977) Congenital cystic adenomatoid malformation of the lung. Hum Pathol 8:155–171
MacSweeney F, Papagiannopoulos K, Goldstraw P (2003) An assessment of the expanded classification of congenital cystic adenomatoid malformations and their relationship to malignant transformation. Am J Surg Pathol 27:1139–1146
Laberge CJM, Bratu I, Flageole H (2004) The management of asymptomatic congenital lung malformations. Paediatr Respir Rev 5:S305–S312
Orazi C, Inserra A, Schingo PM et al (2007) Pleuropulmonary blastoma, a distinctive neoplasm of childhood: report of three cases. Pediatr Radiol 37:337–344
Granata C, Gambini C, Balducci T et al (1998) Bronchioloalveolar carcinoma arising in congenital cystic adenomatoid malformation in a child: a case report and review on malignancies originating in congenital cystic adenomatoid malformation. Pediatr Pulmonol 25:62–66
Lanza C, Bolli V, Galeazzi V et al (2007) Cystic adenomatoid malformation in children: CT histopathological correlation. Radiol Med 112:612–619
Stocker JT, Malczak HT (1984) A study of pulmonary ligament arteries. Relationship to intralobar pulmonary sequestration. Chest 86:611–615
Cleveland RH, Weber B (1993) Retained fetal lung liquid in congenital lobar emphysema: a possible predictor of polyalveolar lobe. Pediatr Radiol 23:291–295
Gardella C, Tomà P, Sacco O et al (2009) Intermittent gaseous bowel distention: atypical sign of congenital tracheoesophageal fistula. Pediatr Pulmonol 44:244–248
Oddone M, Granata C, Vercellino N et al (2005) Multi-modality evaluation of the abnormalities of the aortic arches in children: techniques and imaging spectrum with emphasis on MRI. Pediatr Radiol 35:947–960
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tomà, P., Rizzo, F., Stagnaro, N. et al. Multislice CT in congenital bronchopulmonary malformations in children. Radiol med 116, 133–151 (2011). https://doi.org/10.1007/s11547-010-0582-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-010-0582-4