Abstract
Intestinal parasitic infections (IPIs) are still a serious public health problem worldwide, particularly in developing countries. The COVID-19 pandemic has affected people’s lifestyles and quality of life. Besides, the prevalence of IPIs is directly associated with environmental sanitation, overcrowding, and personal hygiene. Therefore, the current study aimed to determine the prevalence of IPIs among patients referred to hospitals affiliated to Shiraz University of Medical Sciences by reviewing the available data of hospital information system database in the pre- and post-COVID-19 pandemic. The total data of 13,686 patients referred to hospitals affiliated to Shiraz University of Medical Sciences, southern Iran were collected from March 2019 to March 2021. The overall prevalence of IPIs was found to be 4.4%, and Blastocystis spp. was the most common parasite. The prevalence of protozoan parasites (4.4%) was significantly higher than helminthic parasites (0.04%, P < 0.001). A significant association was observed between IPIs with age, gender, and year (P < 0.05). The prevalence of IPIs among those referred to hospitals before the COVID-19 pandemic was higher than those referred to hospitals during the COVID-19 pandemic (5.8% vs 2.8%), and the differences were statistically significant (P < 0.001). The odds of infection among people investigated during the COVID-19 pandemic was about 40% lower than those investigated before the COVID-19 pandemic (AOR: 0.60, 95% CI: 0.49–0.73, P < 0.001). Our results showed that the prevalence of IPIs has decreased during the COVID-19 pandemic. Improved sanitation, personal hygiene, and health education can be effective in reducing parasitic infections in the COVID-19 pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intestinal parasitic infections (IPIs) are considered one of the most important socioeconomic and public health problems worldwide, particularly in developing countries (WHO 1987). About one billion people (mostly children) around the world are estimated to be infected with at least one of the common species of intestinal parasites, including Blastocystis spp., Giardia intestinalis, Entamoeba histolytica/dispar/moshkovskii, Enterobius vermicularis, Hymenolepis nana, Ascaris lumbricoides, Trichuris trichiura, and hookworms (De Silva et al. 2003; Duc et al. 2011). Furthermore, studies have shown that IPIs affect over three billion people worldwide, of whom 300 million suffer from associated severe morbidity (Stephenson et al. 2000; Hotez et al. 2009; WHO 2007; Van Lerberghe 2008).
Based on the studies conducted in Iran, a broad range of intestinal parasites have been reported among various populations. Differences in the prevalence rate of IPIs in various studies may be related to diversity in socioeconomic, personal hygiene, environmental sanitation, cultural, and educational status (Nasiri et al. 2009; Daryani et al. 2017). Awareness of the prevalence and distribution pattern of intestinal parasites is an important indicator to set up a prevention and control program to improve the health status (Hatam-Nahavandi et al. 2017; Afshar et al. 2020). Although a study has been carried out on the prevalence of intestinal parasites among food handlers in Shiraz (Motazedian et al. 2015), no study is available on the distribution of intestinal parasites among apparently healthy populations in Shiraz County as a tropical area in the south of Iran.
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first cases of this disease were identified in Wuhan, China, in December 2019. The disease spread rapidly worldwide and was declared a pandemic on 11 March 2020 (Roberts et al. 2021). The COVID-19 pandemic started in Iran on 19 February 2020 and affected people’s lifestyles and quality of life (Sharma et al. 2020). The COVID-19 affects all ages (Liu et al. 2020), and countries have issued policies to prevent this disease, such as social distancing and staying at home (WHO 2020). Since the prevalence of IPIs is directly associated with environmental sanitation, overcrowding, and personal hygiene (Feleke et al. 2019), health education is effective in reducing IPIs. Therefore, due to the observance of personal and social health during the COVID-19 pandemic, the current study aimed to assess the prevalence of IPIs among patients referred to hospitals affiliated to Shiraz University of Medical Sciences by reviewing the available data of hospital information system databases in the pre- and post-COVID-19 pandemic.
Materials and methods
Study area
Shiraz County (latitude 29°36′37.12″N and longitude 52°31′52.07″E) is the capital of Fars province in southern Iran (Fig. 1) with an administrative area of 43,725 ha. Shiraz metropolitan area population, including the city and surrounding rural areas and Sadra town, has 1.557 million residents according to the last national census by the Statistical Center of Iran. With approximately 93% living in the urban area, the annual population growth rate over the past three decades was 2.04. Geographical hallmarks, such as north, south, and west highlands, together with Maharloo Lake in the vicinity of Shiraz, provide unique conditions from a morphological point of view (Azhdari et al. 2018).
Study design
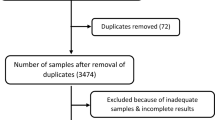
This retrospective study was conducted from March 2019 to March 2021 among patients referred to hospitals affiliated to Shiraz University of Medical Sciences for stool examination. In this cross-sectional study, a retrospective review based on data of the past 2 years in the pre- and post-COVID-19 pandemic was used. The study participants were inpatients and outpatients referred to Namazi and Shahid Faghihi hospitals (Sa’adi hospital), two main teaching hospitals affiliated to Shiraz University of Medical Sciences. All participants gave stool samples for laboratory diagnosis during the study period. Then, the socio-demographic data of participants and laboratory results were collected from the available data of the hospital information system database.
For parasitological analysis, fresh stool samples were collected in the pre-labeled wide-mouth plastic containers. At the time of collection, the date of sampling, the name of the participant, age, and gender were recorded for each subject in a recording format. At the laboratory section of the hospitals, the stool samples were examined macroscopically for determination of consistency and color. Then, the stool specimen was examined microscopically using the direct wet-mount (Garcia et al. 2017).
Statistical analysis
Analytical and descriptive statistics were carried out using Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) version 22 software. Data were described using the calculation of frequencies (%) and 95% confidence intervals (CI). The crude and adjusted associations between IPIs and determinants were assessed using univariate and multiple logistic regressions. In bivariate binary logistic regression analysis, age, year and, gender were the potential associated factors with the presence of IPIs (P < 0.05). Multiple logistic analysis was conducted after adjusting variables which were P < 0.2 in the bivariate binary logistic analysis. The strength of the association between predictor and outcome variables was assessed by using the adjusted odds ratio (AOR) and 95% CI. A P value of < 0.05 was considered to be statistically significant.
Results
Socio-demographic characteristics of study participants
The total data of 13,686 participants referred to hospitals affiliated to Shiraz University of Medical Sciences were included in the present study. The results of socio-demographic characteristics of study participants are summarized in Table 1. Of the total participants, 7421 (54.2%, 95% CI: 53.4–55.1) were males and 6265 (45.8%, 95% CI: 44.9–46.6) were females. The mean age of participants was 44.17 ± 23.99 years. Participants were divided into six major age groups of ≤ 9, 10–19, 20–29, 30–39, 40–49, and ≥ 50. The largest age group was ≥ 50 (43.6%, 95% CI: 42.8–44.5). Among the 13,686 participants, 8928 (65.2%, 95% CI: 64.4–66.0) were inpatient, and 4758 (34.8%, 95% CI: 34.0–35.6) were outpatient. The majority of the samples (7685/13,686) were taken from March 2019 to February 2020 (56.2%, 95% CI: 55.3–57.0) before the COVID-19 pandemic (Table 1).
Macroscopic examination of fecal specimens
Results of macroscopic examination of fecal specimens are summarized in Table 1. The highest frequency of stool color and consistency was brown (78.3%, 95% CI: 77.6–79.0) and soft (54.3%, 95% CI: 53.5–55.2), respectively (Table 1).
Prevalence of intestinal parasitic infections
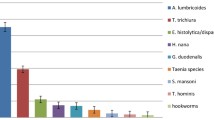
The prevalence of detected intestinal parasites is embedded in Table 2. Intestinal parasites were detected in 609 of 13,686 participants referred to hospitals affiliated to Shiraz University of Medical Sciences (4.4%, 95% CI: 4.1–4.8). The prevalence of protozoan parasites (4.4%) was more than helminthic parasites (0.04%). Blastocystis spp., E. coli, and G. intestinalis were the most common intestinal parasites with a prevalence of 2.8% (95% CI: 2.6–3.1), 0.7% (95% CI: 0.5–0.8), and 0.6% (95% CI: 0.4–0.7), respectively. Chilomastix mesnili, Endolimax nana, E. histolytica/dispar/moshkovskii, Iodamoeba bütschlii, Trichomonas hominis, and Entamoeba hartmanni were other detected protozoan parasites in the study. Furthermore, helminthic infections including H. nana, E. vermicularis, and Strongyloides stercoralis were detected (Table 2). Out of 609 participants infected with intestinal parasites during the period of study, 585 participants (96.06%, 95% CI: 95.6–98.4) were infected with at least one type of the intestinal parasites, and multiple infections constituted 3.94% (95% CI: 2.1–4.8%).
The results of unadjusted and adjusted logistic regression analyses of the variables with IPIs among the participants are embedded in Table 3.
The prevalence rate of IPIs for females and males was 4.0% (248/6265) and 4.9% (361/7421), respectively. The association between prevalence of IPIs and gender was statistically significant (P = 0.013), and the odds of infection in male was about 25% higher than in female (AOR: 1.24, 95% CI: 1.05–1.46).
IPIs were most prevalent among participants aged 30–39 years (5.2%, 95% CI: 4.3–6.3%), and the difference between the age and prevalence of IPIs was significant (P < 0.001). The multivariable logistic regression model estimated that individuals within the age group of 10–19 years were 1.82 times (AOR: 1.82, 95% CI: 1.11–2.99, P = 0.018) more likely to get infected with intestinal parasites than those within the age group of fewer than 10 years. In addition, IPIs were significantly higher in age groups of 30–39 years (AOR: 1.67, 95% CI: 1.11–2.53, P = 0.014), 40–49 years (AOR: 1.68, 95% CI: 1.1–2.56, P = 0.016), and more than 50 years (AOR: 1.64, 95% CI: 1.12–2.39, P = 0.011) than those within the age group of less than 10 years (Table 3).
The prevalence of IPIs among patients referred to hospitals before the COVID-19 pandemic was higher than those referred to hospitals during the COVID-19 pandemic (5.8% vs 2.8%), with statistically significant differences (P < 0.001). The odds of infection among people investigated during the COVID-19 pandemic was about 40% lower than those who investigated before the COVID-19 pandemic (AOR: 0.60, 95% CI: 0.49–0.73).
In this study, 470 of 609 infected cases (77.2%, 95% CI: 73.6–80.5) were the participants referred to Shahid Faghihi hospital and 139 cases (22.8%, 95% CI: 19.5–26.4) to Namazi hospital in Shiraz, Iran. Among the 609 infected participants, 280 (46%) were inpatient, and 329 (54%) were outpatient.
Discussion
Despite the advancement in sanitation infrastructure and hygiene status in today’s societies, there is still a risk of transmission and incidence of parasitic infections. In the current study, the overall prevalence rate of IPIs was estimated to be 4.4% which was approximately similar to prevalence rate of IPIs in Karaj and Qazvin cities (center of Iran) with an overall prevalence of 4.7% and 5.8%, respectively (Nasiri et al. 2009; Sadeghi and Borji 2015). However, the prevalence in the present study was lower than in some previous studies done in various regions of Iran (Haghighi et al. 2009; Vahedi et al. 2012; Jafari et al. 2014, 2016; Kiani et al. 2016; Sarkari et al. 2016). Moreover, this was lower to the findings of previous studies conducted in different areas of the world including Italy (13.24%) (Peruzzi et al. 2006), western India (15.1%) (Shobha et al. 2013), Ethiopia (26.3%) (Alemu and Mama 2017), and Brazil (64.3%) (Barbosa et al. 2018). Differences in the prevalence rate of IPIs in various studies may be due to different factors. The study period, geographic areas, target populations, sanitary/hygiene level, lifestyle and sociodemographic features of the participants, and the methods employed for stool examination can affect the prevalence rate of IPIs.
Blastocystis spp., E. coli, and G. intestinalis were the most prevalent intestinal parasites in the present study. These parasites have been reported almost in most studies on IPIs among different populations in Iran (Nasiri et al. 2009; Barkhori Mahni et al. 2016; Afshar et al. 2020; Teimouri et al. 2020; Abbaszadeh Afshar et al. 2021; Mohebali et al. 2021). The prevalence rate of Blastocystis spp. was reported to be 2.8%, which was lower than the report of Haghighi et al. (2020) in Shiraz (4.86%). Previous studies have reported that the prevalence of Blastocystis spp. was 0.5–54.4% in different parts of Iran (Badparva et al. 2017). E. coli (0.7%) and G. intestinalis (0.6%) were the other common intestinal parasites in this study. G. intestinalis is seen throughout the world and is one of the most frequent protozoa that can lead to diarrhea. Although the overall prevalence of Giardia has been decreased during the past decade in Iran, it is still reported relatively high in some studies due to the target population, especially in children (Afshar et al. 2020). Most people infected with these parasites are asymptomatic and excrete many infectious cysts that survive in the environment for a long time. It seems that the healthy carrier, which enhances the chance of transmission of these parasites to the new host, could explain the high prevalence of these parasites compared with other protozoan parasites (Abbaszadeh Afshar et al. 2021).
The current study revealed a low prevalence of helminthic parasites compared to protozoan parasites (0.04% and 4.4%, respectively). These results were consistent with the previous studies that indicated a decreasing trend in intestinal helminth infections, while intestinal protozoa still have a high prevalence in various areas of Iran (Rokni 2008; Teimouri et al. 2020; Abbaszadeh Afshar et al. 2021). The high prevalence of protozoan parasites is possibly due to their high proliferation rate and the simple route of infection via contaminated foods and water (Abera et al. 2010). The results of the current study reported a prevalence of 0.04% for helminthic infection. The prevalence of intestinal helminthiasis in various parts of Iran has been reported 0–5.8% that is consistent with the findings of the present study (Asgari et al. 2003; Rezaiian et al. 2004; Daryani et al. 2012; Gholipoor et al. 2019). H. nana, E. vermicularis, and S. stercoralis were reported as the parasitic helminths in the present study. In line with our findings, A. lumbricoides, E. vermicularis, S. stercoralis, and H. nana were the most predominant helminths reported among food handlers and intellectually disabled individuals in Iran (Teimouri et al. 2020; Abbaszadeh Afshar et al. 2021). Although the prevalence of human helminthic diseases has decreased in recent decades throughout Iran, some of them, particularly those with direct fecal–oral transmissions, such as Enterobius and Hymenolepis, are still common (Rokni 2008; Goudarzi et al. 2021).
In this study, the prevalence rate of IPIs in males was slightly higher than in females, which was similar to the studies conducted in Ethiopia (Endris et al. 2010), in Nepal (Khanal et al. 2011), and in Brazil (Faria et al. 2017). The result of our study was keeping with the study of Daryani et al. (2017), who analyzed 13 studies comprising sex data and showed that the prevalence in males (14.4%) was significantly higher than that in females (8.9%). In contrast to our study, some reports have shown a higher prevalence of infections among females than males (Saab et al. 2004; Okyay et al. 2004; Belete et al. 2021). This difference may be due to the nature of the activities done at home or outside and their lifestyle.
In the present study, IPIs were reported in all age groups, but there was a statistically significant difference in the proportion of parasitic infections in different age groups. The highest IPIs were reported in the age group of 30–39 years. The findings of our study regarding the association between the prevalence of IPIs and age showed that age could be a potential risk factor for the acquisition of IPIs in participants. More outdoor activities and higher exposure to infectious sources are possible explanations for more prevalence of IPIs in older people. Nevertheless, some studies have shown that the prevalence of IPIs was higher in younger people, especially children (Boontanom et al. 2011). It should be noted that the increase in the prevalence of IPIs with age in the current study might be biased due to uneven sampling in age groups.
The results of the current study showed a significant difference between IPIs and the year of study so that the prevalence of IPIs before the COVID-19 pandemic was higher than during the COVID-19 pandemic. The status of parasitic infection in each community is considered an indicator of the health condition of the region. The decreased prevalence rate of IPIs during the COVID-19 pandemic may be due to changes in the lifestyles of people. During the COVID-19 pandemic, hand hygiene, social distancing, and quarantine were performed to reduce the risk of COVID-19 (Güner et al. 2020), which can reduce the number of IPIs as well. The COVID-19 pandemic has also had a considerable effect on the number of people referred to hospitals. The decrease in the number of outpatients is noticeable in many hospitals during the COVID-19 pandemic. The results of this retrospective study during the COVID-19 pandemic showed that most of the inpatients were patients with severe COVID-19, and the number of outpatients was reduced. Wolday et al. (2021) reported that the patients co-infected with parasites had lower odds of developing severe COVID-19. It has been hypothesized that the low incidence rates of COVID-19 could result from increased exposure to parasites in some countries (Głuchowska et al. 2021). It has also been proposed that parasites may cause a better tolerance of COVID-19 (Ssebambulidde et al. 2020; Fonte et al. 2020).
The current findings should be considered in the context of their strengths and limitations. In this study, the stool samples were examined microscopically using direct wet-mount for the diagnosis of IPIs in participants referred to hospitals affiliated to Shiraz University of Medical Sciences, and the use of one method for diagnosis of IPIs was the limitation of this study. The higher prevalence of IPIs has been reported in the studies which employed two or three diagnosis methods, such as concentration and staining methods besides direct wet-mount method, and the implementation of these methods together increases the sensitivity of IPI detection (Garcia et al. 2017; Teimouri et al. 2020). The main strength of this study is its novelty; to the best of the author’s knowledge, this is the first study on the prevalence of IPIs among outpatients and inpatients referred to hospitals affiliated to Shiraz University of Medical Sciences in the pre- and post-COVID-19 pandemic. Other strengths of this study are the large sample size and coverage of two main hospitals in Shiraz County.
Conclusions
A relatively low prevalence of IPIs was observed among the patients referred to hospitals affiliated to Shiraz University of Medical Sciences in the study period. Blastocystis spp. was the most common intestinal parasite detected, followed by E. coli and G. intestinalis. The IPIs in male were higher than females. Moreover, the 30–39 years age group was more affected by IPIs. Our results showed that the prevalence of IPIs has decreased during the COVID-19 pandemic. Improved sanitation, personal hygiene, and health education can be effective in reducing parasitic infections during the COVID-19 pandemic. However, in recent decades, due to the improvement of the health situation in Iran, the trend of IPIs has decreased. This study has provided baseline information for future studies in the study area. We also found that diagnostic methods that were being used in the hospital at that time were not adequate to detect these infections.
Data Availability
Data generated in this study are included in the published article. Data analyzed during the current study are publicly available via Figshare Repository, https://figshare.com/s/627f36603f1ac0f0da50.
References
Abbaszadeh Afshar MJ, Mohebali M, Mohtasebi S, Teimouri A, Sedaghat B, Saberi R (2021) Intestinal parasites among intellectually disabled individuals in Iran: a systematic review and meta-analysis. Gut Pathog 13:28. https://doi.org/10.1186/s13099-021-00424-6
Abera B, Biadegelgen F, Bezabih B (2010) Prevalence of Salmonella typhi and intestinal parasites among food handlers in Bahir Dar Town, Northwest Ethiopia. Ethiop J Health Sci 24:46–50
Afshar MJA, Mehni MB, Rezaeian M, Mohebali M, Baigi V, Amiri S, Amirshekari MB, Hamidinia R, Samimi M (2020) Prevalence and associated risk factors of human intestinal parasitic infections: a population-based study in the southeast of Kerman province, southeastern Iran. BMC Infect Dis 20:12. https://doi.org/10.1186/s12879-019-4730-8
Alemu G, Mama M (2017) Intestinal helminth co-infection and associated factors among tuberculosis patients in Arba Minch. Ethiopia BMC Infect Dis 17:68. https://doi.org/10.1186/s12879-017-2195-1
Asgari G, Nateghpour M, Rezaian M (2003) Prevalence of intestinal parasites in the inhabitants of Islamshahr district. J Res Health Sci 1:67–74
Azhdari A, Taghvaee AA, Kheyroddin R (2018) Spatiotemporal analysis of Shiraz metropolitan area expansion during 1986–2014: using remote sensing imagery and landscape metrics. Int J Architect Eng Urban Plan 28(2):163–173
Badparva E, Ezatpour B, Mahmoudvand H, Behzadifar M, Behzadifar M, Kheirandish F (2017) Prevalence and genotype analysis of Blastocystis hominis in Iran: a systematic review and meta-analysis. Arch Clin Infect Dis 12:e36648. https://doi.org/10.5812/archcid.36648
Barbosa CV, Barreto MM, Andrade RJ, Sodré F, d’Avila-Levy CM, Peralta JM, Igreja RP, de Macedo HW, Santos HLC (2018) Intestinal parasite infections in a rural community of Rio de Janeiro (Brazil): prevalence and genetic diversity of Blastocystis subtypes. PLoS ONE 13:e0193860. https://doi.org/10.1371/journal.pone.0193860
Barkhori Mahni MB, Rezaeian M, Kia EB, Raeisi A, Khanaliha K, Tarighi F, Kamranrashani B (2016) Prevalence of intestinal parasitic infections in Jiroft, Kerman province. Iran Iran J Parasitol 11:232–238
Belete YA, Kassa TY, Baye MF (2021) Prevalence of intestinal parasite infections and associated risk factors among patients of Jimma health center requested for stool examination, Jimma. Ethiopia Plos ONE 16:e0247063. https://doi.org/10.1371/journal.pone.0247063
Boontanom P, Mungthin M, Tan-Ariya P, Naaglor T, Leelayoova S (2011) Epidemiology of giardiasis and genotypic characterization of Giardia duodenalis in preschool children of a rural community, central Thailand. Trop Biome 28:32–39
Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G (2012) Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg 106:455–459. https://doi.org/10.1016/j.trstmh.2012.05.010
Daryani A, Hosseini-Teshnizi S, Hosseini SA, Ahmadpour E, Sarvi S, Amouei A, Mizani A, Gholami S, Sharif M (2017) Intestinal parasitic infections in Iranian preschool and school children: a systematic review and meta-analysis. Acta Trop 169:69–83. https://doi.org/10.1016/j.actatropica.2017.01.019
De Silva NR, Brooker S, Hotez PJ, Montresor A, Engels D, Savioli L (2003) Soil-transmitted helminth infections: updating the global picture. Trends Parasitol 19:547–551. https://doi.org/10.1016/j.pt.2003.10.002
Duc PP, Nguyen-Viet H, Hattendorf J, Zinsstag J, Cam PD, Odermatt P (2011) Risk factors for Entamoeba histolytica infection in an agricultural community in Hanam province. Vietnam Parasit Vectors 4:102. https://doi.org/10.1186/1756-3305-4-102
Endris M, Lemma W, Belyhun Y, Moges B, Gelaw A, Angaw B, Alemayehu M, Tedla BA, Mahdi JA, Teklu T, Worku L, Aemero M, Taye BW, Wal G (2010) Prevalence of intestinal parasites and associated risk factors among students of Atse Fasil general elementary school Azezo, Northwestern Ethiopia. Ethiop J Health Biomed Sci 3:25–33
Faria CP, Zanini GM, Dias GS, da Silva S, de Freitas MB, Almendra R, Santana P, Sousa MD (2017) Geospatial distribution of intestinal parasitic infections in Rio de Janeiro (Brazil) and its association with social determinants. PLoS Neglected Tropical Diseases, 11(3), p.e0005445. https://doi.org/10.1371/journal.pntd.0005445
Feleke BE, Beyene MB, Feleke TE, Jember TH, Abera B (2019) Intestinal parasitic infection among household contacts of primary cases, a comparative cross-sectional study. PLoS ONE 14(10):e0221190. https://doi.org/10.1371/journal.pone.0221190
Fonte L, Acosta A, Sarmiento ME, Ginori M, García G, Norazmi MN (2020) COVID-19 Lethality in Sub-Saharan Africa and helminth immune modulation. Front Immunol 11:574910. https://doi.org/10.3389/fimmu.2020.574910
Garcia LS, Arrowood M, Kokoskin E, Paltridge GP, Pillai DR, Procop GW, Ryan N, Shimizu RY, Visvesvara G (2017) Laboratory diagnosis of parasites from the gastrointestinal tract. Clin Microbiol Rev 31:e00025-e117. https://doi.org/10.1128/CMR.00025-17
Gholipoor Z, Khazan H, Azargashb E, Youssefi MR, Rostami A (2019) Prevalence and risk factors of intestinal parasite infections in Mazandaran province, North of Iran. Clin Epidemiol Glob Health 8:17–20. https://doi.org/10.1016/j.cegh.2019.03.010
Głuchowska K, Dzieciątkowski T, Sędzikowska A, Zawistowska-Deniziak A, Młocicki D (2021) The new status of parasitic diseases in the COVID-19 pandemic-risk factors or protective agents? J Clin Med 10:2533. https://doi.org/10.3390/jcm10112533
Goudarzi F, Mohtasebi S, Teimouri A, Yimam Y, Heydarian P, Salehi Sangani G, Abbaszadeh Afshar MJ (2021) A systematic review and meta-analysis of Hymenolepis nana in human and rodent hosts in Iran: a remaining public health concern. Comp Immunol Microbiol Infect Dis 74:101580
Güner R, Hasanoğlu I, Aktaş F (2020) COVID-19: Prevention and control measures in community. Turk J Med Sci 50:571–577. https://doi.org/10.3906/sag-2004-146
Haghighi A, Khorashad AS, Mojarad EN, Kazemi B, Nejad MR, Rasti S (2009) Frequency of enteric protozoan parasites among patients with gastrointestinal complaints in medical centers of Zahedan, Iran. Trans R Soc Trop Med Hyg 103:452–454. https://doi.org/10.1016/j.trstmh.2008.11.004
Haghighi L, Talebnia SM, Mikaeili F, Asgari Q, Gholizadeh F, Zomorodian K (2020) Prevalence and subtype identification of Blastocystis isolated from human in Shiraz city, southern Iran. Clin Epidemiol Glob Health 8:840–844
Hatam-Nahavandi K, Mohebali M, Mahvi AH, Keshavarz H, Mirjalali H, Rezaei S, Meamar AR, Rezaeian M (2017) Subtype analysis of Giardia duodenalis isolates from municipal and domestic raw wastewaters in Iran. Environ Sci Pollut Res Int 24:12740–12747. https://doi.org/10.1007/s11356-016-6316-y
Hotez HP, Fenwick A, Savioli L, Molyneux DH (2009) Rescuing the bottom billion through control of neglected tropical diseases. Lancet 373:1570–1575. https://doi.org/10.1016/S0140-6736(09)60233-6
Jafari R, Fallah M, Yousofi Darani H, Yousefi H, Mohaghegh MA, Latifi M, Sadaghian M, Maghsood AH (2014) Prevalence of intestinal parasitic infections among rural inhabitants of Hamadan city, Iran, 2012. Avicenna J Clin Microbiol Infect 1:e21445. https://doi.org/10.17795/ajcmi-21445
Jafari R, Sharifi F, Bagherpour B, Safari M (2016) Prevalence of intestinal parasites in Isfahan city, central Iran, 2014. J Parasit Dis 40:679–682. https://doi.org/10.1007/s12639-014-0557-9
Khanal L, Choudhury D, Rai S, Sapkota J, Barakoti A, Amatya R, Hada S (2011) Prevalence of intestinal worm infestations among school children in Kathmandu. Nepal 13:272–274
Kiani H, Haghighi A, Rostami A, Azargashb E, Tabaei SJ, Solgi A, Zebardast N (2016) Prevalence, risk factors and symptoms associated to intestinal parasite infections among patients with gastrointestinal disorders in Nahavand, Western Iran. Rev Do Inst Med Trop São Paulo 58:42. https://doi.org/10.1590/S1678-9946201658042
Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S, Chen L, Liang L, Zhou J, You L, Wu P, Zhang B, Lu Y, Xia L, Huang L, Yang Y, Liu F, Semple MG, Cowling BJ, Lan K, Sun Z, Yu H, Liu Y (2020) Detection of COVID-19 in children in early January 2020 in Wuhan. China N Engl J Med 382(14):1370–1371. https://doi.org/10.1056/NEJMc2003717
Mohebali M, Keshavarz H, Abbaszadeh Afshar MJ, Hanafi-Bojd AA, Hassanpour GH (2021) Spatial distribution of common pathogenic human intestinal protozoa in Iran: a systematic review article. Iran J Public Health 50:69–82. https://doi.org/10.18502/ijph.v50i1.5073
Motazedian MH, Najjari M, Ebrahimipour M, Asgari Q, Mojtabavi S, Mansouri M (2015) Prevalence of intestinal parasites among food-handlers in Shiraz. Iran Iran J Parasitol 10:652–657
Nasiri V, Esmailnia K, Karim G, Nasir M, Akhavan O (2009) Intestinal parasitic infections among inhabitants of Karaj City, Tehran province, Iran in 2006–2008. Kor J Parasitol 47(3):265–268. https://doi.org/10.3347/kjp.2009.47.3.265
Okyay P, Ertug S, Gultekin B, Onen O, Beser E (2004) Intestinal parasites prevalence and related factors in school children, a western city sample-Turkey. BMC Public Health 4:64. https://doi.org/10.1186/1471-2458-4-64
Peruzzi S, Gorrini C, Piccolo G, Calderaro A, Dettori G, Chezzi C (2006) Prevalence of intestinal parasites in the area of Parma during the year 2005. Acta Biomed 77:147–151
Rezaiian M, Jalalian M, Kia EB, Massoud J, Mahdavi M, Rokni MB (2004) Relationship between serum Ige and intestinal parasites. Iran J Public Health 33:18–21
Roberts DL, Rossman JS, Jarić I (2021) Dating first cases of COVID-19. PLoS Pathog 17:e1009620. https://doi.org/10.1371/journal.ppat.1009620
Rokni M (2008) The present status of human helminthic diseases in Iran. Ann Trop Med PH 102:283–295. https://doi.org/10.1179/136485908X300805
Saab BR, Musharrafieh U, Nassar NT, Khogali M, Araj GF (2004) Intestinal parasites among presumably healthy individuals in Lebanon. Saudi Med J 25:34–37
Sadeghi H, Borji H (2015) A survey of intestinal parasites in a population in Qazvin, north of Iran. Asian Pac J Trop Dis 5:231–233. https://doi.org/10.1016/s2222-1808(14)60659-9
Sarkari B, Hosseini G, Motazedian MH, Fararouei M, Moshfe A (2016) Prevalence and risk factors of intestinal protozoan infections: a population-based study in rural areas of Boyer-Ahmad district. Southwestern Iran BMC Infect Dis 16(1):703. https://doi.org/10.1186/s12879-016-2047-4
Sharma A, Tiwari S, Deb MK, Marty JL (2020) Severe acute respiratory syndrome coronavirus -2 (SARS-CoV-2): a global pandemic and treatments strategies. Int J Antimicrob Agents 56:106054. https://doi.org/10.1016/j.ijantimicag.2020.106054
Shobha M, Bithika D, Bhavesh S (2013) The prevalence of intestinal parasitic infections in the urban slums of a city in Western India. J Infect Public Health 6:142–149. https://doi.org/10.1016/j.jiph.2012.11.004
Ssebambulidde K, Segawa I, Abuga KM, Nakate V, Kayiira A, Ellis J, Tugume L, Kiragga AN, Meya DB (2020) Parasites and their protection against COVID-19—ecology or immunology? MedRxiv.
Stephenson LS, Latham MC, Ottesen EA (2000) Malnutrition and parasitic helminthes infections. Parasitol Res 121:S23-38. https://doi.org/10.1017/s0031182000006491
Teimouri A, Keshavarz H, Mohtasebi S, Goudarzi F, Mikaeili F, Borjian A, Allahmoradi M, Yimam Y, Abbaszadeh Afshar MJ (2020) Intestinal parasites among food handlers in Iran: a systematic review and meta-analysis. Food Microbiol 95:103703. https://doi.org/10.1016/j.fm.2020.103703
Vahedi M, Gohardehi S, Sharif M, Daryani A (2012) Prevalence of parasites in patients with gastroenteritis at East of Mazandaran Province, Northern Iran. Trop Biomed 29:568–574
Van Lerberghe W (2008) The world health report 2008: primary health care: now more than ever. World Health Organization.
Wolday D, Gebrecherkos T, Arefaine ZG, Kiros YK, Gebreegzabher A, Tasew G, Abdulkader M, Abraha HE, Desta AA, Hailu A, Tollera G, Abdella S, Tesema M, Abate E, Endarge KL, Hundie TG, Miteku FK, Urban BC, Schallig HHDF, Harris VC, de Wit TFR (2021) Effect of co-infection with intestinal parasites on COVID-19 severity: a prospective observational cohort study. EClinicalMedicine 39:101054.
World Health Organization (1987) Prevention and control of intestinal parasitic infections: report of a WHO Expert Committee [meeting held in Geneva from 3 to 7 March 1986].
World Health Organization (2007) Partners for parasite control: geographical distribution and useful facts and stats. WHO, Geneva.
World Health Organization (2020) Coronavirus disease 2019 (COVID-19): situation report, 73.
Acknowledgements
We would like to acknowledge all laboratory staff from Namazi and Shahid Faghihi hospitals, Shiraz, Iran for their useful collaboration.
Funding
This research was financially supported by the office of the Vice-chancellor for research at Shiraz University of Medical Sciences with grant no: 99–01-01–23015.
Vice-Chancellor for Research,Shiraz University of Medical Sciences,99–01-01–23015,Fattaneh Mikaeili
Author information
Authors and Affiliations
Contributions
FM designed the study; SF collected the data from the hospital information system database; FM, AT, and RA conceived, analyzed, and interpreted the data. AT and FM drafted the manuscript; all authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out based on the ethical standards by institutional and/or national research committees and Helsinki Declaration, 1964. This study was approved by the research ethics committee of Shiraz University of Medical Sciences with an ethical code: IR.SUMS.MED.REC.1399.581. Information collected from the study participants was kept confidential.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teimouri, A., Alimi, R., Farsi, S. et al. Intestinal parasitic infections among patients referred to hospitals affiliated to Shiraz University of Medical Sciences, southern Iran: a retrospective study in pre- and post-COVID-19 pandemic. Environ Sci Pollut Res 29, 36911–36919 (2022). https://doi.org/10.1007/s11356-021-18192-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-18192-w