Abstract
Purpose
Obstructive sleep apnea (OSA) is induced by a sleep-related collapse of the upper airway in association with multiple factors. The severity of OSA is determined by the apnea-hypopnea index (AHI). Although obesity and sex differences are common factors in OSA, the level of the AHI varies to the same degree according to the age and sex and degree of obesity. However, only a few studies have evaluated AHI over 100/h, those reports did not describe why they set the AHI cutoff at 100/h. The purpose of this study was to elucidate the pathogenesis of “very” severe OSA, defined as having an AHI > 100/h.
Methods
AHI > 100/h was set as very severe OSA (VS-OSA) in this study. As controls, moderate to severe OSA patients, matched with VS-OSA for age, sex, and body mass index (BMI), were enrolled. The findings of polysomnography and cephalography between VS-OSA and controls were compared.
Results
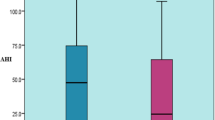
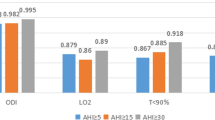
Eleven patients in the VS-OSA group (mean AHI 110.2/h) and 22 patients in the control group (mean AHI 41.6/h) were compared (mean age 50.2 vs 50.6, male:female 5:6 vs 10:12, mean BMI 35.4 kg/m2 vs 34.5 kg/m2). There were no significant differences in the clinical characteristics. In the polysomnographic parameters, the VS-OSA group showed apnea predominance, the mean percutaneous oxygen saturation (SO2) was significantly lower in all sleep stages, and the minimum SO2 was significantly lower (49.0% vs 77.5%, p = 0.002). A similar apnea duration and rather shorter hypopnea duration were shown. The time of apnea-to-arousal was significantly earlier (− 0.1 s vs 0.9 s, p = 0.003). Lung-to-finger circulation time showed no differences. The cephalometric findings showed no significant differences.
Conclusions
VS-OSA patients were more likely to have apnea predominance, desaturation when sleeping despite a similar apnea duration, and rather shorter hypopnea duration, and arousals were evoked significantly earlier.


Similar content being viewed by others
References
American Academy of Sleep Medicine (2014) International classification ofsleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien, IL
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus CL, Vaughn BV (2012) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, Version 2.0. www.aasmnet.org. American Academy of Sleep Medicine, Darien, IL
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 284(23):3015–3021. https://doi.org/10.1001/jama.284.23.3015
Li J, Chen X, Sun J (2014) Is the grading system of the severity of the OSAHS used presently rational or not?: from the view of incidence of hypertension in different severity groups. Eur Arch Otorhinolaryngol 271:2561–2564
Marin JM, Carrizo AJ, Vicente E, Agusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep -disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283(14):1829–1836
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
Davies RJO, Stradling JR (1990) The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep-apnea syndrome. Eur Respir J 3(5):509–514
Katz I, Stradling J, Slutsky AS, Zamel N, Hoffstein V (1990) Do patients with obstructive sleep-apnea have thick necks. Am Rev Respir Dis 141(5):1228–1231. https://doi.org/10.1164/ajrccm/141.5_Pt_1.1228
Rey de Castro J, Huamani C, Escobar-Cordoba F, Liendo C (2015) Clinical factors associated with extreme sleep apnoea [AHI>100 events per hour] in Peruvian patients: a case-control study-a preliminary report. Sleep Sci 8(1):31–35. https://doi.org/10.1016/j.slsci.2015.03.002
Goodday RH, Bourque SE, Edwards PB (2016) Objective and subjective outcomes following maxillomandibular sdvancement aurgery for treatment of patients with extremely severe obstructive sleep apnea (apnea-hypopnea index >100). J Oral Maxillofac Surg 74(3):583–589
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep M (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619. https://doi.org/10.5664/jcsm.2172
Simms T, Brijbassi M, Montemurro LT, Bradley TD (2013) Differential timing of arousals in obstructive and central sleep apnea in patients with heart failure. J Clin Sleep Med 9(8):773–779. https://doi.org/10.5664/jcsm.2918
Yatsu S, Kasai T, Matsumoto H, Murata A, Kato T, Suda S, Hiki M, Shiroshita N, Kato M, Kawana F, Daida H (2017) Change in type of sleep-disordered breathing from predominant central to obstructive sleep apnea following coronary artery bypass grafting. J Cardiol Cases 16(3):93–96. https://doi.org/10.1016/j.jccase.2017.05.009
Partinen M, Guilleminault C, Quera-Salva MA, Jamieson A (1988) Obstructive sleep apnea and cephalometric roentgenograms. The role of anatomic upper airway abnormalities in the definition of abnormal breathing during sleep. Chest 93(6):1199–1205. https://doi.org/10.1378/chest.93.6.1199
Inoshita A, Kasai T, Takahashi M, Inoshita H, Kasagi S, Kawana F, Ishiwata S, Ohno M, Yamaguchi T, Narui K, Ikeda K (2014) Craniofacial anatomical risk factors in men with obstructive sleep apnea and heart failure: a pilot study. Sleep Breath 18(2):439–445. https://doi.org/10.1007/s11325-013-0906-4
Edwards BA, Eckert DJ, McSharry DG, Sands SA, Desai A, Kehlmann G, Bakker JP, Genta PR, Owens RL, White DP, Wellman A, Malhotra A (2014) Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190(11):1293–1300. https://doi.org/10.1164/rccm.201404-0718OC
Dudley KA, Patel SR (2016) Disparities and genetic risk factors in obstructive sleep apnea. Sleep Med 18:96–102. https://doi.org/10.1016/j.sleep.2015.01.015
Mathew R, Castriotta RJ (2014) High hypopnea/apnea ratio (HAR) in extreme obesity. J Clin Sleep Med 10(4):391–396. https://doi.org/10.5664/jcsm.3612
Saboisky JP, Stashuk DW, Hamilton-Wright A, Trinder J, Nandedkar S, Malhotra A (2014) Effects of aging on genioglossus motor units in humans. PLoS One 9(8):e104572. https://doi.org/10.1371/journal.pone.0104572
Cistulli PA (1996) Craniofacial abnormalities in obstructive sleep apnoea: implications for treatment. Respirology 1(3):167–174. https://doi.org/10.1111/j.1440-1843.1996.tb00028.x
Sutherland K, Lee RW, Cistulli PA (2012) Obesity and craniofacial structure as risk factors for obstructive sleep apnoea: impact of ethnicity. Respirology 17(2):213–222. https://doi.org/10.1111/j.1440-1843.2011.02082.x
Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, Lin HM, Kales A, Chrousos GP (2000) Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab 85(3):1151–1158. https://doi.org/10.1210/jcem.85.3.6484
Yu X, Fujimoto K, Urushibata K, Matsuzawa Y, Kubo K (2003) Cephalometric analysis in obese and nonobese patients with obstructive sleep apnea syndrome. Chest 124(1):212–218. https://doi.org/10.1378/chest.124.1.212
Mayer P, Pepin JL, Bettega G, Veale D, Ferretti G, Deschaux C, Levy P (1996) Relationship between body mass index, age and upper airway measurements in snorers and sleep apnoea patients. Eur Respir J 9(9):1801–1809. https://doi.org/10.1183/09031936.96.09091801
Shelton KE, Woodson H, Gay S, Suratt PM (1993) Pharyngeal fat in obstructive sleep apnea. Am Rev Respir Dis 148(2):462–466. https://doi.org/10.1164/ajrccm/148.2.462
Horner RL, Mohiaddin RH, Lowell DG, Shea SA, Burman ED, Longmore DB, Guz A (1989) Sites and sizes of fat deposits around the pharynx in obese patients with obstructive sleep apnoea and weight matched controls. Eur Respir J 2(7):613–622
Kimura Y, Kasai T, Tomita Y, Kasagi S, Takaya H, Kato M, Kawana F, Narui K (2020) Relationship between metabolic syndrome and hypercapnia among obese patients with sleep apnea. World Journal of Respirology 10(1):1–10. https://doi.org/10.5320/wjr.v10.i1.1
Abdeyrim A, Zhang Y, Li N, Zhao M, Wang Y, Yao X, Keyoumu Y, Yin T (2015) Impact of obstructive sleep apnea on lung volumes and mechanical properties of the respiratory system in overweight and obese individuals. BMC Pulm Med 15:76. https://doi.org/10.1186/s12890-015-0063-6
White DP (2005) Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med 172(11):1363–1370. https://doi.org/10.1164/rccm.200412-1631SO
Wellman A, Eckert DJ, Jordan AS, Edwards BA, Passaglia CL, Jackson AC, Gautam S, Owens RL, Malhotra A, White DP (2011) a method for measuring and modeling the physiological traits causing obstructive sleep apnea. J Appl Physiol (1985) 110(6):1627–1637. https://doi.org/10.1152/japplphysiol.00972.2010
Younes M (2004) Role of arousals in the pathogenesis of obstructive sleep apnea. Am J Respir Crit Care Med 169(5):623–633. https://doi.org/10.1164/rccm.200307-1023OC
Dingli K, Fietze I, Assimakopoulos T, Quispe-Bravo S, Witt C, Douglas NJ (2002) Arousability in sleep apnoea/hypopnoea syndrome patients. Eur Respir J 20(3):733–740. https://doi.org/10.1183/09031936.02.00262002
Author information
Authors and Affiliations
Contributions
N.S. and A.I.: Designed and performed experiments, analyzed data, and co-wrote the paper. S. Suda: Performed lung-to-finger circulation time analyses. S. Shiota: Performed respiratory function analyses. N.S. and F.K.: Performed polysomnographic analyses. Y.S. and F.M.: Performed cepharogaphic analyses. K.I.: Supervised the research. T.K.: Supervised the research and co-write the paper. All authors contributed to the writing of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest/
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
Since, in the present study, the sleep study, anthropometric data collection and cephalometric data had already been obtained and analyzed as in a routine clinical checkup, the requirement to obtain informed consent was waived by the ethics committee of Juntendo University Hospital using opt-out methods (#19-273).
Consent for publication
Not applicable.
Code availability
The datasets generated during and/or analyzed during the current study available from the corresponding author on reasonable request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 34 kb)
Rights and permissions
About this article
Cite this article
Sata, N., Inoshita, A., Suda, S. et al. Clinical, polysomnographic, and cephalometric features of obstructive sleep apnea with AHI over 100. Sleep Breath 25, 1379–1387 (2021). https://doi.org/10.1007/s11325-020-02241-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02241-8