Abstract
Purpose
Present systematic literature review and dose-response meta-analysis were carried out to evaluate the association between sleep duration and sarcopenia risk.
Methods
Related studies were found by searching ISI Web of science databases, Scopus, and PubMed, up to May, 2019. Data were available from four studies. A total odds ratio of 17551 participants in these studies was pooled for the current study.
Results
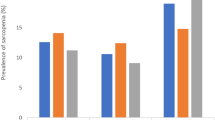
Pooled outcomes from random effects model demonstrated that lowest category of sleep duration (under 6 h) versus reference category (6–8 h) was significantly related with increased risk of sarcopenia (OR: 1.71 95% CI, 1.11, 2.64). Pooled OR also indicated that highest category (more than 8 h) of sleep duration versus reference category (6–8 h) was significantly associated with increased risk of sarcopenia (OR: 1.52 95% CI, 1.23, 1.88). Moreover, subgroup analysis by sex showed that women were affected by both short and long sleep while men were only affected by long sleep duration. The nonlinear dose-response meta-analysis revealed a U-shaped association between sleep duration and the risk of sarcopenia, with a nadir at 8 h per day. The linear dose-response meta-analysis illustrated that the risk of sarcopenia did not change significantly nor for a 0.5-h increment neither for 1-h increment in sleep duration per day.
Conclusion
The outcomes from this meta-analysis indicate that the public should be made aware of the negative consequences of long and short sleep for sarcopenia especially among women. Further studies should now be undertaken to establish possible links between risk of sarcopenia and sleep duration.








Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- GH:
-
Growth hormone
- HPA:
-
Hypothalamo-pituitary-adrenal
- IGF-1:
-
Insulin-like growth factor-1
- OR:
-
Odds ratio
References
Woo J (2017) Sarcopenia. Clin Geriatr Med 33(3):305–314. https://doi.org/10.1016/j.cger.2017.02.003
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127(5):990S–991S
Volpi E, Nazemi R, Fujita S (2004) Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care 7(4):405–410
Grimby G, Saltin B (1983) The ageing muscle. Clin Physiol 3(3):209–218
Rooyackers OE, Adey DB, Ades PA, Nair KS (1996) Effect of age on in vivo rates of mitochondrial protein synthesis in human skeletal muscle. Proc Natl Acad Sci 93(26):15364–15369
Hanna JS (2015) Sarcopenia and critical illness: a deadly combination in the elderly. J Parenter Enteral Nutr 39(3):273–281
Janssen I, Heymsfield SB, Ross R (2002) Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 50(5):889–896
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, van Kan GA, Andrieu S, Bauer J, Breuille D (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12(4):249–256
Carey KA, Farnfield MM, Tarquinio SD, Cameron-Smith D (2007) Impaired expression of Notch signaling genes in aged human skeletal muscle. J Gerontol A Biol Sci Med Sci 62(1):9–17
Schrager MA, Roth SM, Ferrell RE, Metter EJ, Russek-Cohen E, Lynch NA, Lindle RS, Hurley BF (2004) Insulin-like growth factor-2 genotype, fat-free mass, and muscle performance across the adult life span. J Appl Physiol 97(6):2176–2183
Kuh D, Bassey EJ, Butterworth S, Hardy R, Wadsworth ME (2005) Grip strength, postural control, and functional leg power in a representative cohort of British men and women: associations with physical activity, health status, and socioeconomic conditions. J Gerontol A Biol Sci Med Sci 60(2):224–231
Hughes VA, Roubenoff R, Wood M, Frontera WR, Evans WJ, Fiatarone Singh MA (2004) Anthropometric assessment of 10-y changes in body composition in the elderly. Am J Clin Nutr 80(2):475–482
Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ (2007) Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 297(16):1769–1774. https://doi.org/10.1001/jama.297.16.1772-b
Chapman IM, MacIntosh CG, Morley JE, Horowitz M (2002) The anorexia of ageing. Biogerontology 3(1-2):67–71
Volpi E, Sheffield-Moore M, Rasmussen BB, Wolfe RR (2001) Basal muscle amino acid kinetics and protein synthesis in healthy young and older men. Jama 286(10):1206–1212
Katsanos CS, Kobayashi H, Sheffield-Moore M, Aarsland A, Wolfe RR (2005) Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am J Clin Nutr 82(5):1065–1073
Campbell WW, Crim MC, Dallal GE, Young VR, Evans WJ (1994) Increased protein requirements in elderly people: new data and retrospective reassessments. Am J Clin Nutr 60(4):501–509
Campbell WW, Trappe TA, Wolfe RR, Evans WJ (2001) The recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscle. J Gerontol A Biol Sci Med Sci 56(6):M373–M380
Guillet C, Boirie Y (2005) Insulin resistance: a contributing factor to age-related muscle mass loss? Diabetes Metab 31:5S20–25S26
McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, Chan C, Celic L, Pearce WH, Schneider JR (2001) Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA 286(13):1599–1606
Mcdermott MM, Guralnik JM, Albay M, Bandinelli S, Miniati B, Ferrucci L (2004) Impairments of muscles and nerves associated with peripheral arterial disease and their relationship with lower extremity functioning: the InCHIANTI Study. J Am Geriatr Soc 52(3):405–410
McDermott MM, Guralnik JM, Ferrucci L, Tian L, Pearce WH, Hoff F, Liu K, Liao Y, Criqui MH (2007) Physical activity, walking exercise, and calf skeletal muscle characteristics in patients with peripheral arterial disease. J Vasc Surg 46(1):87–93
Park SW, Goodpaster BH, Lee JS, Kuller LH, Boudreau R, De Rekeneire N, Harris TB, Kritchevsky S, Tylavsky FA, Nevitt M (2009) Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care
Park SW, Goodpaster BH, Strotmeyer ES, De Rekeneire N, Harris TB, Schwartz AV, Tylavsky FA, Newman AB (2006) Decreased muscle strength and quality in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes 55(6):1813–1818
Baumgartner RN, Waters DL, Gallagher D, Morley JE, Garry PJ (1999) Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Dev 107(2):123–136
Morley JE (2003) Hormones and the aging process. J Am Geriatr Soc 51(7 s):S333–S337
Ferrucci L, Penninx BW, Volpato S, Harris TB, Bandeen-Roche K, Balfour J, Leveille SG, Fried LP, Md JM (2002) Change in muscle strength explains accelerated decline of physical function in older women with high interleukin-6 serum levels. J Am Geriatr Soc 50(12):1947–1954
Dockray S, Steptoe A (2011) Chronotype and diurnal cortisol profile in working women: differences between work and leisure days. Psychoneuroendocrinology 36(5):649–655. https://doi.org/10.1016/j.psyneuen.2010.09.008
Lucassen EA, Rother KI, Cizza G (2012) Interacting epidemics? Sleep curtailment, insulin resistance, and obesity. Ann N Y Acad Sci 1264(1):110–134. https://doi.org/10.1111/j.1749-6632.2012.06655.x
Neikrug AB, Ancoli-Israel S (2010) Sleep disorders in the older adult – a mini-review. Gerontology 56(2):181–189. https://doi.org/10.1159/000236900
Everitt H, Baldwin DS, Stuart B, Lipinska G, Mayers A, Malizia AL, Manson CC, Wilson S (2018) Antidepressants for insomnia in adults. Cochrane Database Syst Rev 5:CD010753. https://doi.org/10.1002/14651858.CD010753.pub2
Jespersen KV, Koenig J, Jennum P, Vuust P (2015) Music for insomnia in adults. Cochrane Database Syst Rev 8:CD010459. https://doi.org/10.1002/14651858.CD010459.pub2
Specker B, Binkley T, Vukovich M, Beare T (2007) Volumetric bone mineral density and bone size in sleep-deprived individuals. Osteoporos Int 18(1):93–99
Fex A, Barbat-Artigas S, Dupontgand S, Filion M-E, Karelis AD, Aubertin-Leheudre M (2012) Relationship between long sleep duration and functional capacities in postmenopausal women. J Clin Sleep Med 8(03):309–313
Dattilo M, Antunes HKM, Medeiros A, Neto MM, HSD S, Tufik S, De Mello M (2011) Sleep and muscle recovery: endocrinological and molecular basis for a new and promising hypothesis. Med Hypotheses 77(2):220–222
Kalyani RR, Corriere M, Ferrucci L (2014) Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol 2(10):819–829
Lucassen EA, de Mutsert R, le Cessie S, Appelman-Dijkstra NM, Rosendaal FR, van Heemst D, den Heijer M, Biermasz NR, group Ns (2017) Poor sleep quality and later sleep timing are risk factors for osteopenia and sarcopenia in middle-aged men and women: The NEO study. PloS One 12(5):e0176685. https://doi.org/10.1371/journal.pone.0176685
Chien M-Y, Wang L-Y, Chen H-C (2015) The relationship of sleep duration with obesity and sarcopenia in community-dwelling older adults. Gerontology 61(5):399–406
Hu X, Jiang J, Wang H, Zhang L, Dong B, Yang M (2017) Association between sleep duration and sarcopenia among community-dwelling older adults: a cross-sectional study. Medicine 96(10)
Kim RH, Kim KI, Kim JH, Park YS (2018) Association between sleep duration and body composition measures in Korean adults: the Korea National Health and Nutrition Examination Survey 2010. Korean J Fam Med 39(4):219–224
Kwon Y-J, Jang S-Y, Park E-C, Cho A-R, Shim J-Y, Linton JA (2017) Long sleep duration is associated with sarcopenia in Korean adults based on data from the 2008–2011 KNHANES. J Clin Sleep Med 13(09):1097–1104
Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, Perruolo E, Parati G (2016) Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PloS One 11(1):e0147601
Moradi S, Mirzababaei A, Dadfarma A, Rezaei S, Mohammadi H, Jannat B, Mirzaei K (2019) Food insecurity and adult weight abnormality risk: a systematic review and meta-analysis. Eur J Nutr 58(1):45–61
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135(11):1301–1309
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2011) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175(1):66–73
Hamling J, Lee P, Weitkunat R, Ambühl M (2008) Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med 27(7):954–970
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-response data. Stata J 6(1):40
Harre FE Jr, Lee KL, Pollock BG (1988) Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst 80(15):1198–1202
Jackson D, White IR, Thompson SG (2010) Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med 29(12):1282–1297
Berlin JA, Longnecker MP, Greenland S (1993) Meta-analysis of epidemiologic dose-response data. Epidemiology:218–228
Liu Q, Cook NR, Bergström A, Hsieh C-C (2009) A two-stage hierarchical regression model for meta-analysis of epidemiologic nonlinear dose–response data. Comput Stat Data Anal 53(12):4157–4167
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Denison HJ, Cooper C, Sayer AA, Robinson SM (2015) Prevention and optimal management of sarcopenia: a review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin Interv Aging 10:859
Buchmann N, Spira D, Norman K, Demuth I, Eckardt R, Steinhagen-Thiessen E (2016) Sleep, muscle mass and muscle function in older people. Deutsch Arztebl Int 113(15):253–260. https://doi.org/10.3238/arztebl.2016.0253
Nam GE, Han K, Kim DH, Lee JH, Seo WH (2017) Sleep duration is associated with body fat and muscle mass and waist-to-height ratio beyond conventional obesity parameters in Korean adolescent boys. J Sleep Res 26(4):444–452. https://doi.org/10.1111/jsr.12502
Chen Y, Cui Y, Chen S, Wu Z (2017) Relationship between sleep and muscle strength among Chinese university students: a cross-sectional study. J Musculoskelet Neuronal Interact 17(4):327–333
Knowles OE, Drinkwater EJ, Urwin CS, Lamon S, Aisbett B (2018) Inadequate sleep and muscle strength: Implications for resistance training. J Sci Med Sport
Anderson LJ, Liu H, Garcia JM (2017) Sex differences in muscle wasting. Adv Exp Med Biol 1043:153–197. https://doi.org/10.1007/978-3-319-70178-3_9
Gheller BJ, Riddle ES, Lem MR, Thalacker-Mercer AE (2016) Understanding age-related changes in skeletal muscle metabolism: differences between females and males. Ann Rev Nutr 36:129–156. https://doi.org/10.1146/annurev-nutr-071715-050901
Garatachea N, Lucía A (2013) Genes and the ageing muscle: a review on genetic association studies. Age 35(1):207–233
Naranjo JD, Dziki JL, Badylak SF (2017) Regenerative medicine approaches for age-related muscle loss and sarcopenia: a mini-review. Gerontology 63(6):580–589
Brinkman JE, Sharma S (2018) Physiology, Sleep. In: StatPearls. StatPearls Publishing LLC., Treasure Island
Piovezan RD, Abucham J, dos Santos RVT, Mello MT, Tufik S, Poyares D (2015) The impact of sleep on age-related sarcopenia: possible connections and clinical implications. Ageing Res Rev 23:210–220
Trenell MI, Marshall NS, Rogers NL (2007) Sleep and metabolic control: waking to a problem? Clin Exp Pharmacol Physiol 34(1-2):1–9. https://doi.org/10.1111/j.1440-1681.2007.04541.x
Seelig E, Keller U, Klarhofer M, Scheffler K, Brand S, Holsboer-Trachsler E, Hatzinger M, Bilz S (2013) Neuroendocrine regulation and metabolism of glucose and lipids in primary chronic insomnia: a prospective case-control study. PLoS one 8(4):e61780. https://doi.org/10.1371/journal.pone.0061780
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pourmotabbed, A., Ghaedi, E., Babaei, A. et al. Sleep duration and sarcopenia risk: a systematic review and dose-response meta-analysis. Sleep Breath 24, 1267–1278 (2020). https://doi.org/10.1007/s11325-019-01965-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01965-6