Abstract
Activated astrocytes play a key role in diabetic neuropathic pain and depression. We aimed to assess the protective effects of dihydromyricetin (DHM) on primary hippocampal astrocytes cultured with high glucose (HG), substance P (SP), and corticosterone (CORT). Culturing with HG + SP + CORT resulted in damage to primary hippocampal astrocytes, which simulates the clinical damage caused by comorbidity of diabetic neuropathic pain and depression. Western blot, qPCR, and immunofluorescence analyses revealed that HG + SP + CORT increased P2X7 receptor expression in primary hippocampal astrocytes, which was reversed by DHM treatment. Further, HG + SP + CORT elevated TNF-α, IL-1β, free Ca2+, and ERK1/2 phosphorylation levels, which was inhibited by DHM or P2X7 shRNA treatment. Moreover, DHM significantly reduced the P2X7 agonist-activated currents in HEK293 cells transfected with the P2X7 receptor. These findings suggest that DHM can protect primary hippocampal astrocytes cultured with HG + SP + CORT from P2X7 receptor-mediated damage. Culturing cells with HG + SP + CORT might be a viable cell model for cellular injury exploration of diabetic comorbid pain and depression.









Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Unnikrishnan R, Pradeepa R, Joshi SR, Mohan V (2017) Type 2 diabetes: demystifying the global epidemic. Diabetes 66(6):1432–1442. https://doi.org/10.2337/db16-0766
Naranjo C, Del Reguero L, Moratalla G, Hercberg M, Valenzuela M, Failde I (2019) Anxiety, depression and sleep disorders in patients with diabetic neuropathic pain: a systematic review. Expert Rev Neurother 19(12):1201–1209. https://doi.org/10.1080/14737175.2019.1653760
Galer BS, Gianas A, Jensen MP (2000) Painful diabetic polyneuropathy: epidemiology, pain description, and quality of life. Diabetes Res Clin Pract 47(2):123–128. https://doi.org/10.1016/s0168-8227(99)00112-6
Ren X, Yu S, Dong W, Yin P, Xu X, Zhou M (2020) Burden of depression in China, 1990–2017: findings from the global burden of disease study 2017. J Affect Disord 268:95–101. https://doi.org/10.1016/j.jad.2020.03.011
Moulton CD, Pickup JC, Ismail K (2015) The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol 3(6):461–471. https://doi.org/10.1016/S2213-8587(15)00134-5
Fiore V, Marci M, Poggi A, Giagulli VA, Licchelli B, Iacoviello M, Guastamacchia E, De Pergola G, Triggiani V (2015) The association between diabetes and depression: a very disabling condition. Endocrine. 48(1):14–24. https://doi.org/10.1007/s12020-014-0323-x
Lee GB, Kim HC, Jung SJ (2019) Association between depression and disease-specific treatment. J Affect Disord 260:124–130. https://doi.org/10.1016/j.jad.2019.08.073
Jain R, Jain S, Raison CL, Maletic V (2011) Painful diabetic neuropathy is more than pain alone: examining the role of anxiety and depression as mediators and complicators. Curr Diab Rep 11(4):275–284. https://doi.org/10.1007/s11892-011-0202-2
Severini C, Improta G, Falconieri-Erspamer G, Salvadori S, Erspamer V (2002) The tachykinin peptide family. Pharmacol Rev 54(2):285–322. https://doi.org/10.1124/pr.54.2.285
Mashaghi A, Marmalidou A, Tehrani M, Grace PM, Pothoulakis C, Dana R (2016) Neuropeptide substance P and the immune response. Cell Mol Life Sci 73(22):4249–4264. https://doi.org/10.1007/s00018-016-2293-z
Schmidt MJ, Roth J, Ondreka N, Kramer M, Rummel C (2013) A potential role for substance P and interleukin-6 in the cerebrospinal fluid of Cavalier King Charles Spaniels with neuropathic pain. J Vet Intern Med 27(3):530–535. https://doi.org/10.1111/jvim.12080
Zieglgansberger W (2019) Substance P and pain chronicity. Cell Tissue Res 375(1):227–241. https://doi.org/10.1007/s00441-018-2922-y
Won E, Kang J, Choi S, Kim A, Han KM, Yoon HK, Cho SH, Tae WS, Lee MS, Joe SH, Kim YK, Ham BJ (2017) The association between substance P and white matter integrity in medication-naive patients with major depressive disorder. Sci Rep 7(1):9707. https://doi.org/10.1038/s41598-017-10100-y
Holsboer F (2001) Stress, hypercortisolism and corticosteroid receptors in depression: implications for therapy. J Affect Disord 62(1–2):77–91. https://doi.org/10.1016/S0165-0327(00)00352-9
Feng S, Liu J, Cheng B, Deng A, Zhang H (2018) (−)-Epigallocatechin-3-gallate protects PC12 cells against corticosterone-induced neurotoxicity via the hedgehog signaling pathway. Exp Ther Med 15(5):4284–4290. https://doi.org/10.3892/etm.2018.5936
Shi X, Zhou N, Cheng J, Shi X, Huang H, Zhou M, Zhu H (2019) Chlorogenic acid protects PC12 cells against corticosterone-induced neurotoxicity related to inhibition of autophagy and apoptosis. BMC Pharmacol Toxicol 20(1):56. https://doi.org/10.1186/s40360-019-0336-4
Sterner EY, Kalynchuk LE (2010) Behavioral and neurobiological consequences of prolonged glucocorticoid exposure in rats: relevance to depression. Prog Neuropsychopharmacol Biol Psychiatry 34(5):777–790. https://doi.org/10.1016/j.pnpbp.2010.03.005
Rajkowska G, Stockmeier CA (2013) Astrocyte pathology in major depressive disorder: insights from human postmortem brain tissue. Curr Drug Targets 14(11):1225–1236. https://doi.org/10.2174/13894501113149990156
Zhao Y, Pu D, Sun Y, Chen J, Luo C, Wang M, Zhou J, Lv A, Zhu S, Liao Z, Zhao K, Xiao Q (2018) High glucose-induced defective thrombospondin-1 release from astrocytes via TLR9 activation contributes to the synaptic protein loss. Exp Cell Res 363(2):171–178. https://doi.org/10.1016/j.yexcr.2017.12.030
Inoue K, Tsuda M, Tozaki-Saitoh H (2012) Role of the glia in neuropathic pain caused by peripheral nerve injury. Brain Nerve 64(11):1233–1239. https://doi.org/10.11477/mf.1416101336
Liao YH, Zhang GH, Jia D, Wang P, Qian NS, He F, Zeng XT, He Y, Yang YL, Cao DY, Zhang Y, Wang DS, Tao KS, Gao CJ, Dou KF (2011) Spinal astrocytic activation contributes to mechanical allodynia in a mouse model of type 2 diabetes. Brain Res 1368:324–335. https://doi.org/10.1016/j.brainres.2010.10.044
Czeh B, Di Benedetto B (2013) Antidepressants act directly on astrocytes: evidences and functional consequences. Eur Neuropsychopharmacol 23(3):171–185. https://doi.org/10.1016/j.euroneuro.2012.04.017
Zhao YA, Lin ZX, Chen L, Ouyang LF, Gu L, Chen FY, Zhang Q (2018) Hippocampal astrocyte atrophy in a mouse depression model induced by corticosterone is reversed by fluoxetine instead of benzodiazepine diazepam. Prog Neuro-Psychopharmacol Biol Psychiatry 83:99–109. https://doi.org/10.1016/j.pnpbp.2018.01.011
Wang Q, Verweij EWE, Krugers HJ, Joels M, Swaab DF, Lucassen PJ (2018) Distribution of the glucocorticoid receptor in the human amygdala; changes in mood disorder patients. Brain Struct Funct 19(5):1615–1626. https://doi.org/10.1007/s00429-013-0589-4
Miras-Portugal MT, Sebastian-Serrano A, Garcia LD, Diaz-Hernandez M (2017) Neuronal P2X7 receptor: involvement in neuronal physiology and pathology. J Neurosci 37(30):7063–7072. https://doi.org/10.1523/Jneurosci.3104-16.2017
Chrovian CC, Rech JC, Bhattacharya A, Letavic MA (2014) P2X7 antagonists as potential therapeutic agents for the treatment of CNS disorders. Prog Med Chem 53:65–100. https://doi.org/10.1016/B978-0-444-63380-4.00002-0
Shen YL, Guan S, Ge HX, Xiong W, He LK, Liu LJ, Yin CC, Liu H, Li GL, Xu CS, Xu H, Liu SM, Li GD, Liang SD, Gao Y (2018) Effects of palmatine on rats with comorbidity of diabetic neuropathic pain and depression. Brain Res Bull 139:56–66. https://doi.org/10.1016/j.brainresbull.2018.02.005
Zhang K, Liu JY, You XT, Kong P, Song YC, Cao L, Yang S, Wang WB, Fu Q, Ma ZQ (2016) P2X7 as a new target for chrysophanol to treat lipopolysaccharide-induced depression in mice. Neurosci Lett 613:60–65. https://doi.org/10.1016/j.neulet.2015.12.043
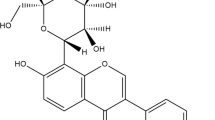
Jia L, Zhao W, Sang J, Wang W, Wei W, Wang Y, Zhao F, Lu F, Liu F (2019) Inhibitory effect of a flavonoid dihydromyricetin against Aβ40 amyloidogenesis and its associated cytotoxicity. ACS Chem Neurosci 10(11):4696–4703. https://doi.org/10.1021/acschemneuro.9b00480
Lin Y, Fan J, Ruan L, Bi J, Yan Y, Wang T, Gao H, Yao X, Cheng K, Zhang W (2019) Semi-preparative separation of dihydromyricetin enantiomers by supercritical fluid chromatography and determination of anti-inflammatory activities. J Chromatogr A1606:460386. https://doi.org/10.1016/j.chroma.2019.460386
Xie K, He X, Chen KY, Chen JH, Sakao K, Hou DX (2019) Antioxidant properties of a traditional vine tea, Ampelopsis grossedentata. Antioxidants (Basel) 8(8):295. https://doi.org/10.3390/antiox8080295
Feng QW, Cui ZG, Jin YJ, Sun L, Li ML, Zakki SA, Zhou DJ, Inadera H (2019) Protective effect of dihydromyricetin on hyperthermia-induced apoptosis in human myelomonocytic lymphoma cells. Apoptosis 24(3–4):290–300. https://doi.org/10.1007/s10495-019-01518-y
Zhang J, Chen Y, Luo H, Sun L, Xu M, Yu J, Zhou Q, Meng G, Yang S (2018) Recent update on the pharmacological effects and mechanisms of dihydromyricetin. Front Pharmacol 9:1204. https://doi.org/10.3389/fphar.2018.01204
Salzer I, Gantumur E, Yousuf A, Boehm S (2016) Control of sensory neuron excitability by serotonin involves 5HT2C receptors and Ca(2+)-activated chloride channels. Neuropharmacology 110(Pt A):277–286. https://doi.org/10.1016/j.neuropharm.2016.08.006
Zhao S, Zhou Y, Fan Y, Gong Y, Yang J, Yang R, Li L, Zou L, Xu X, Li G, Liu S, Zhang C, Li G, Liang S (2019) Involvement of P2X4 receptor in gp120-induced pyroptosis in dorsal root ganglia. J Neurochem 151(5):584–594. https://doi.org/10.1111/jnc.14850
Gubba EM, Fawcett JW, Herbert J (2004) The effects of corticosterone and dehydroepiandrosterone on neurotrophic factor mRNA expression in primary hippocampal and astrocyte cultures. Mol Brain Res 127(1–2):48–59. https://doi.org/10.1016/j.molbrainres.2004.05.004
Lim D, Mapelli L, Canonico PL, Moccia F, Genazzani AA (2018) Neuronal activity-dependent activation of astroglial calcineurin in mouse primary hippocampal cultures. Int J Mol Sci 19(10):2997. https://doi.org/10.3390/ijms19102997
Chen Q, Wu H, Tao J, Liu C, Deng Z, Liu Y, Chen G, Liu B, Xu C (2017) Effect of naringin on gp120-induced injury mediated by P2X7 receptors in rat primary cultured microglia. PLoS One 12(8):e0183688. https://doi.org/10.1371/journal.pone.0183688
Zhang C, Deng Y, Dai H, Zhou W, Tian J, Bing G, Zhao L (2017) Effects of dimethyl sulfoxide on the morphology and viability of primary cultured neurons and astrocytes. Brain Res Bull 128:34–39. https://doi.org/10.1016/j.brainresbull.2016.11.004
Yi Y, Shen Y, Wu Q, Rao J, Guan S, Rao S, Huang L, Tan M, He L, Liu L, Li G, Liang S, Xiong W, Gao Y (2018) Protective effects of oxymatrine on vascular endothelial cells from high-glucose-induced cytotoxicity by inhibiting the expression of A2B receptor. Cell Physiol Biochem 45(2):558–571. https://doi.org/10.1159/000487033
Liu S, Zou L, Xie J, Xie W, Wen S, Xie Q, Gao Y, Li G, Zhang C, Xu C, Xu H, Wu B, Lv Q, Zhang X, Wang S, Xue Y, Liang S (2016) LncRNA NONRATT021972 siRNA regulates neuropathic pain behaviors in type 2 diabetic rats through the P2X7 receptor in dorsal root ganglia. Mol Brain 9:44. https://doi.org/10.1186/s13041-016-0226-2
Yang R, Li L, Yuan H, Liu H, Gong Y, Zou L, Li S, Wang Z, Shi L, Jia T, Zhao S, Wu B, Yi Z, Gao Y, Li G, Xu H, Liu S, Zhang C, Li G, Liang S (2019) Quercetin relieved diabetic neuropathic pain by inhibiting upregulated P2X4 receptor in dorsal root ganglia. J Cell Physiol 234(3):2756–2764. https://doi.org/10.1002/jcp.27091
Wu M, Xu L, Teng C, Xiao X, Hu W, Chen J, Tu W (2019) Involvement of oxidative stress in di-2-ethylhexyl phthalate (DEHP)-induced apoptosis of mouse NE-4C neural stem cells. Neurotoxicology 70:41–47. https://doi.org/10.1016/j.neuro.2018.10.013
Guo C, Wang J, Jing L, Ma R, Liu X, Gao L, Cao L, Duan J, Zhou X, Li Y, Sun Z (2018) Mitochondrial dysfunction, perturbations of mitochondrial dynamics and biogenesis involved in endothelial injury induced by silica nanoparticles. Environ Pollut 236:926–936. https://doi.org/10.1016/j.envpol.2017.10.060
Tang Y, Li GD (2004) Chronic exposure to high glucose impairs bradykinin-stimulated nitric oxide production by interfering with the phospholipase-C-implicated signalling pathway in endothelial cells: evidence for the involvement of protein kinase C. Diabetologia 47(12):2093–2104. https://doi.org/10.1007/s00125-004-1589-y
Bahniwal M, Little JP, Klegeris A (2017) High glucose enhances neurotoxicity and inflammatory cytokine secretion by stimulated human astrocytes. Curr Alzheimer Res 14(7):731–741. https://doi.org/10.2174/1567205014666170117104053
D'Amato C, Morganti R, Greco C, Di Gennaro F, Cacciotti L, Longo S, Mataluni G, Lauro D, Marfia GA, Spallone V (2016) Diabetic peripheral neuropathic pain is a stronger predictor of depression than other diabetic complications and comorbidities. Diab Vasc Dis Res 13(6):418–428. https://doi.org/10.1177/1479164116653240
Duan-Porter W, Goldstein KM, McDuffie JR, Hughes JM, Clowse ME, Klap RS, Masilamani V, Allen LaPointe NM, Nagi A, Gierisch JM, Williams JW Jr (2016) Reporting of sex effects by systematic reviews on interventions for depression, diabetes, and chronic pain. Ann Intern Med 165(3):184–193. https://doi.org/10.7326/M15-2877
Cherif F, Zouari HG, Cherif W, Hadded M, Cheour M, Damak R (2020) Depression prevalence in neuropathic pain and its impact on the quality of life. Pain Res Manag 2020:7408508–7408508. https://doi.org/10.1155/2020/7408508
Norenberg W, Schunk J, Fischer W, Sobottka H, Riedel T, Oliveira JF, Franke H, Illes P (2010) Electrophysiological classification of P2X7 receptors in rat cultured neocortical astroglia. Brit J Pharmacol 160(8):1941–1952. https://doi.org/10.1111/j.1476-5381.2010.00736.x
Ballerini P, Ciccarelli R, Caciagli F, Rathbone MP, Werstiuk ES, Traversa U, Buccella S, Giuliani P, Jang S, Nargi E, Visini D, Santavenere C, Di Iorio P (2005) P2X7 receptor activation in rat brain cultured astrocytes increases the biosynthetic release of cysteinyl leukotrienes. Int J Immunopathol Pharmacol 18(3):417–430. https://doi.org/10.1177/039463200501800303
Xiong Y, Sun S, Teng S, Jin M, Zhou Z (2018) Ca(2+)-dependent and Ca(2+)-independent ATP release in astrocytes. Front Mol Neurosci 11:224. https://doi.org/10.3389/fnmol.2018.00224
Gelin CF, Bhattacharya A, Letavic MA (2020) P2X7 receptor antagonists for the treatment of systemic inflammatory disorders. Prog Med Chem59:63–99. doi:https://doi.org/10.1016/bs.pmch.2019.11.002
Zhang W, Zhu Z, Liu Z (2020) The role and pharmacological properties of the P2X7 receptor in neuropathic pain.Brain Res Bull155:19–28. doi:https://doi.org/10.1016/j.brainresbull.2019.11.006
Li H, Li Q, Liu Z, Yang K, Chen Z, Cheng Q, Wu L (2017) The versatile effects of dihydromyricetin in health. Evid Based Complement Alternat Med 2017:1053617–1053610. https://doi.org/10.1155/2017/1053617
Murakami T, Miyakoshi M, Araho D, Mizutani K, Kambara T, Ikeda T, Chou WH, Inukai M, Takenaka A, Igarashi K (2004) Hepatoprotective activity of tocha, the stems and leaves of Ampelopsis grossedentata, and ampelopsin. Biofactors 21(1–4):175–178. https://doi.org/10.1002/biof.552210136
Sheng W, Zong Y, Mohammad A, Ajit D, Cui J, Han D, Hamilton JL, Simonyi A, Sun AY, Gu Z, Hong JS, Weisman GA, Sun GY (2011) Pro-inflammatory cytokines and lipopolysaccharide induce changes in cell morphology, and upregulation of ERK1/2, iNOS and sPLA(2)-IIA expression in astrocytes and microglia. J Neuroinflammation 8:121. https://doi.org/10.1186/1742-2094-8-121
Kim SK, Nabekura J, Koizumi S (2017) Astrocyte-mediated synapse remodeling in the pathological brain. Glia 65(11):1719–1727. https://doi.org/10.1002/glia.23169
Wu B, Peng L, Xie J, Zou L, Zhu Q, Jiang H, Yi Z, Wang S, Xue Y, Gao Y, Li G, Liu S, Zhang C, Li G, Liang S, Xiong H (2017) The P2X7 receptor in dorsal root ganglia is involved in HIV gp120-associated neuropathic pain. Brain Res Bull 135:25–32. https://doi.org/10.1016/j.brainresbull.2017.09.006
Donnelly-Roberts DL, Jarvis MF (2007) Discovery of P2X7 receptor-selective antagonists offers new insights into P2X7 receptor function and indicates a role in chronic pain states. Br J Pharmacol 151(5):571–579. https://doi.org/10.1038/sj.bjp.0707265
Acknowledgments
We thank Prof. Shangdong Liang and Prof. Guodong Li for assisting us in the experimental design.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 81760152).
Author information
Authors and Affiliations
Contributions
Y.G. designed the study; H.G. and M.S. carried out the experiments; X. W., M. Z., H.T., Y. H., R.C., and M.Y. assisted H.G to carry out the findings; H.G. drafted the manuscript and all authors reviewed the manuscript and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no financial or other conflicts of interest in association with this work.
Ethical approval
This study was approved by the Animal Care and Ethics Committee of Nanchang University. We performed the experiments in accordance with the guidelines of the National Institutes of Health on Laboratory Animal Care and Use (NIH Publication No. 8023, Rev. 1978).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Huixiang Ge, Mengyun Sun, and Xingyu Wei Joint first authors
Rights and permissions
About this article
Cite this article
Ge, H., Sun, M., Wei, X. et al. Protective effects of dihydromyricetin on primary hippocampal astrocytes from cytotoxicity induced by comorbid diabetic neuropathic pain and depression. Purinergic Signalling 16, 585–599 (2020). https://doi.org/10.1007/s11302-020-09752-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-020-09752-9