Abstract
Objective
Fluid balance is important in patients undergoing hemodialysis. “Dry” weight is usually estimated clinically, and also, bioimpedance is considered reliable. Ultrasonography of inferior vena cava (IVC) estimates central venous pressure, and lung ultrasound evaluates extravascular (counting B-lines artifact) lung water. Our study was aimed to clarify their usefulness in the assessment of volume status during hemodialysis.
Methods
A total of 71 consecutive patients undergoing hemodialysis underwent lung and IVC ultrasound and bioimpedance spectroscopy immediately before and after dialysis.
Results
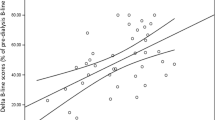
There was a significant reduction in the number of B-lines (3.13 vs 1.41) and in IVC diameters (end-expiratory diameter 1.71 vs 1.37; end-inspiratory diameter 1.19 vs 0.95) during dialysis. The reduction in B-lines correlated with weight reduction during dialysis (p 0.007); none of the parameters concerning the IVC correlated with fluid removal. At the end of the dialysis session, the total number of B-lines correlated with bioimpedance residual weight (p 0.002).
Discussion
The reduction in B-lines correlated with fluid loss due to hemodialysis, despite the small pre-dialysis number, confirming that lung ultrasound can identify even modest variations in extravascular lung water. IVC ultrasound, which reflects the intravascular filling grade, might not be sensitive enough to detect rapid volume decrease. Clinically estimated dry weight had a poor correlation with both bioimpedance and ultrasound techniques. Post-dialysis B-lines number correlates with residual weight assessed with bioimpedance, suggesting a role for ultrasound in managing hemodialysis patients.
Similar content being viewed by others
References
Jaeger JQ, Mehta RL (1999) Assessment of dry weight in hemodialysis: an overview. J Am Soc Nephrol 10(2):392–403
Goldberg AP, Tindira C, Harter HR (1982) Coronary risk in patients with endstage renal disease: interaction of hypertension with hyperlipidemia. J Cardiovasc Pharmacol 4(Suppl 2):S257–S261
Kalantar-Zadeh K, Regidor DL, Kovesdy CP et al (2009) Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation 119(5):671–679 (Epub 2009 Jan 26)
Kooman JP, van der Sande FM, Leunissen KM (2009) Wet or dry in dialysis—can new technologies help? Semin Dial 22(1):9–12 (Review)
Kotanko P, Levin NW, Zhu F (2008) Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant 23(3):808–812. (Epub 2008 Jan 8) (Review)
Cheriex EC, Leunissen KM, Janssen JH et al (1989) Echography of the inferior vena cava is a simple and reliable tool for estimation of ‘dry weight’ in haemodialysis patients. Nephrol Dial Transplant 4(6):563–568
Kouw PM, Kooman JP, Cheriex EC et al (1993) Assessment of postdialysis dry weight: a comparison of techniques. J Am Soc Nephrol 4(1):98–104
Leunissen KM, Kouw P, Kooman JP et al (1993) New techniques to determine fluid status in hemodialyzed patients. Kidney Int Suppl 41:S50–S56 (Review)
Brennan JM, Ronan A, Goonewardena S et al (2006) Handcarried ultrasound measurement of the inferior vena cava for assessment of intravascular volume status in the outpatient hemodialysis clinic. Clin J Am Soc Nephrol 1(4):749–753 (Epub 2006 May 24)
Katzarski KS, Nisell J, Randmaa I et al (1997) A critical evaluation of ultrasound measurement of inferior vena cava diameter in assessing dry weight in normotensive and hypertensive hemodialysis patients. Am J Kidney Dis 30(4):459–465
Agarwal R, Bouldin JM, Light RP et al (2011) Inferior vena cava diameter and left atrial diameter measure volume but not dry weight. Clin J Am Soc Nephrol 6(5):1066–1072 (Epub 2011 Feb 17)
Noble VE, Murray AF, Capp R et al (2009) Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest 135(6):1433–1439 (Epub 2009 Feb 2)
Mallamaci F, Benedetto FA, Tripepi R et al (2010) Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging 3(6):586–594
Trezzi M, Torzillo D, Ceriani E et al (2011) Lung ultrasonography for the assessment of rapid extravascular water variation: evidence from hemodialysis patients. Intern Emerg Med
Lichtenstein D, Mézière G, Biderman P et al (1997) The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 156(5):1640–1646
Soldati G, Copetti R, Sher S (2009) Sonographic interstitial syndrome: the sound of lung water. J Ultrasound Med 28(2):163–174
Agricola E, Bove T, Oppizzi M et al (2005) “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127(5):1690–1695
Jambrik Z, Monti S, Coppola V et al (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 93(10):1265–1270
Lichtenstein DA, Mezière GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134(1):117–125 (Epub 2008 Apr 10)
Picano E, Gargani L, Gheorghiade M (2010) Why, when, and how to assess pulmonary congestion in heart failure: pathophysiological, clinical, and methodological implications. Heart Fail Rev 15(1):63–72 (Review)
Vitturi N, Soattin M, Allemand E et al (2011) Thoracic ultrasonography: a new method for the work-up of patients with dyspnea. J Ultrasound 14(3):147–151
Passauer J, Petrov H, Schleser A et al (2010) Evaluation of clinical dry weight assessment in haemodialysis patients using bioimpedance spectroscopy: a cross-sectional study. Nephrol Dial Transplant 25:545–551
Katzarski K, Charra B, Laurent G et al (1996) Multifrequency bioimpedance in assessment of dry weight in haemodialysis. Nephrol Dial Transplant 11(Suppl 2):20–23
Dou Y, Zhu F, Kotanko P (2012) Assessment of extracellular fluid volume and fluid status in hemodialysis patients: current status and technical advances. Semin Dial 25:377–387
Sperandeo M, Varriale A, Sperandeo G et al (2012) Assessment of ultrasound acoustic artifacts in patients with acute dyspnea: a multicenter study. Acta Radiol 53(8):885–892
Soldati G, Copetti R, Sher S (2011) Can lung comets be counted as “objects”? JACC Cardiovasc Imaging 4(4):438–439
Barbier C, Loubières Y, Schmit C et al (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30:1740–1746
Feissel M, Michard F, Faller JP et al (2004) The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30:1834–1837
Acknowledgments
All authors have contributed significantly, and all authors are in agreement with the content of the manuscript. MS, FS and LM performed the ultrasound examinations; NV reviewed all the examinations and analyzed the data; MD, RZ and MCM performed the bioimpedance analysis.
Conflict of interest
The authors declare that they have no relevant financial interests nor conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vitturi, N., Dugo, M., Soattin, M. et al. Lung ultrasound during hemodialysis: the role in the assessment of volume status. Int Urol Nephrol 46, 169–174 (2014). https://doi.org/10.1007/s11255-013-0500-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-013-0500-5