Abstract
Purpose
To assess the impact of the number of lymph nodes removed and of the template of dissection during radical cystectomy for bladder cancer on patients’ survival rates.
Materials and methods
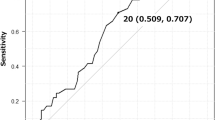
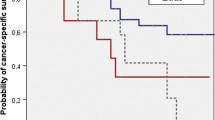
We evaluated 282 consecutive patients who underwent radical cystectomy for muscle-invasive or high-grade superficial bladder cancer between 1995 and 2011. Exclusion criteria were incomplete follow-up data and neo-adjuvant or adjuvant treatments. Patients were divided into groups according to the most informative cut-point of number of lymph nodes retrieved and of the template of dissection. The cancer-specific survival rates were estimated by the Kaplan–Meier method. The univariate and multivariable forward-stepwise Cox proportional hazards regression were applied to analyze the survival outcomes.
Results
The mean (SD) follow-up was 59.2 ± 44.3 months, and the mean (SD) age of the entire cohort population was 68.3 ± 8.3 years. The cancer-specific survival rates were 58.7 and 47.7 % at 5 and 10 years, respectively. Considering both node-positive and node-negative patients, those with at least 14 LNs removed and those submitted to extended or super-extended PLND experienced significantly higher cancer-specific survival at both univariate and multivariable analysis.
Conclusions
Patients undergoing a more extended pelvic lymph node dissection, both in terms of number of LN removed and in terms of template of dissection, will experience a better cancer-specific survival. Our data support a potential role of lymphadenectomy on cancer outcome.


Similar content being viewed by others
References
Kondo T, Tanabe K (2012) Role of lymphadenectomy in the management of urothelial carcinoma of the bladder and the upper urinary tract. Int J Urol 19(8):710–721
Herr HW, Bochner BH, Dalbagni G et al (2002) Impact of the number of lymph nodes retrieved on outcome in patients with muscle invasive bladder cancer. J Urol 167:1295–1298
Brunocilla E, Pernetti R, Martorana G (2011) The role of pelvic lymph node dissection during radical cystectomy for bladder cancer. Anticancer Res 31(1):271–275
Jensen TK, Holt P, Gerke O et al (2011) Preoperative lymph node staging of invasive urothelial bladder cancer with 18F- fluorodeoxyglucose positron emission tomography/computed axial tomography and magnetic resonance imaging: correlation with histopathology. Scand J Urol Nephrol 45:122–128
Maurer T, Souvatzoglou M, Kübler H et al (2012) Diagnostic efficacy of [11C]choline positron emission tomography/computed tomography compared with conventional computed tomography in lymph node staging of patients with bladder cancer prior to radical cystectomy. Eur Urol 61(5):1031–1038
Leissner J, Ghoneim MA, bol-Enein H et al (2004) Extended radical lymphadenectomy in patients with urothelial bladder cancer: results of a prospective multicenter study. J Urol 171:139–144
Wiesner C, Salzer A, Thomas C et al (2009) Cancer-specific survival after radical cystectomy and standardized extended lymphadenectomy for node-positive bladder cancer: prediction by lymph node positivity and density. BJU Int 104:331–335
Holmer M, Bendahl PO, Davidsson T et al (2009) Extended lymph node dissection in patients with urothelial cell carcinoma of the bladder: can it make a difference? World J Urol 27:521–526
Dhar NB, Klein EA, Reuther AM et al (2008) Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. J Urol 179:873–878
bol-Enein H, Tilki D, Mosbah A et al (2011) Does the extent of lymphadenectomy in radical cystectomy for bladder cancer influence disease-free survival? A prospective single-center study. Eur Urol 60:572–577
Wright JL, Lin DW, Porter MP (2008) The association between extent of lymphadenectomy and survival among patients with lymph node metastases undergoing radical cystectomy. Cancer 112:2401–2408
Honma I, Masumori N, Sato E et al (2006) Removal of more lymph nodes may provide better outcome, as well as more accurate pathologic findings, in patients with bladder cancer–analysis of role of pelvic lymph node dissection. Urology 68:543–548
Stenzl A, Cowan NC, De SM et al (2011) Treatment of muscle-invasive and metastatic bladder cancer: update of the EAU guide- lines. Eur Urol 59:1009–1018
Svatek R, Zehnder P (2012) Role and extent of lymphadenectomy during radical cystectomy for invasive bladder cancer. Curr Urol Rep 13(2):115–121
Morgan TM, Barocas DA, Penson DF et al (2012) Lymph node yield at radical cystectomy predicts mortality in node-negative and not node-positive patients. Urology 80(3):632–640. doi:10.1016/j.urology.2012.03.070
Brunocilla E, Pernetti R, Martorana G (2011) The prognostic role of lymphovascular invasion in urothelial-cell carcinoma of upper and lower urinary tract. Anticancer Res 31(10):3503–3506
Palmieri F, Brunocilla E, Bertaccini A et al (2010) Prognostic value of lymphovascular invasion in bladder cancer in patients treated with radical cystectomy. Anticancer Res 30:2973–2976
Sobin LH, Gospodariwicz M, Wittekind C (eds) (2009) TNM classification of malignant tumors. UICC international union against cancer, 7th edn. Wiley, Hoboken, pp 262–265
Schiavina R, Borghesi M, Guidi M et al (2013) Perioperative complications and mortality after radical cystectomy when using a standardized reporting methodology. Clin Genitourin Cancer. doi:10.1016/j.clgc.2012.12.003
Park J, Kim S, Jeong IG et al (2011) Does the greater number of lymph nodes removed during standard lymph node dissection predict better patient survival following radical cystectomy? World J Urol 29(4):443–449
Zehnder P, Studer UE, Skinner EC et al (2011) Super extended versus extended pelvic lymph node dissection in patients undergoing radical cystectomy for bladder cancer: a comparative study. J Urol 186(4):1261–1268
Dorin RP, Daneshmand S, Eisenberg MS et al (2011) Lymph Node dissection technique is more important than lymph node count in identifying nodal metastases in radical cystectomy patients: a comparative mapping study. Eur Urol 60(5):946–952
Stein JP, Penson DF, Cai J et al (2007) Radical cystectomy with extended lymphadenectomy: evaluating separate package versus en bloc submission for node positive bladder cancer. J Urol 177:876–881
Jensen JB, Ulhøi BP, Jensen KM (2012) Extended versus limited lymph node dissection in radical cystectomy: impact on recurrence pattern and survival. Int J Urol 19(1):39–47
Morgan TM, Kaffenberger SD, Cookson MS (2012) Surgical and chemotherapeutic management of regional lymph nodes in bladder cancer. J Urol 188(4):1081–1088
Feinstein AR, Sosin DM, Wells CK (1985) The Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med 312:1604–1608
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brunocilla, E., Pernetti, R., Schiavina, R. et al. The number of nodes removed as well as the template of the dissection is independently correlated to cancer-specific survival after radical cystectomy for muscle-invasive bladder cancer. Int Urol Nephrol 45, 711–719 (2013). https://doi.org/10.1007/s11255-013-0461-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-013-0461-8