Abstract
Aim
To analyze possible factors associated with the quality of life (QoL) of mothers of preterm infants with very low birth weight (VLBW) during the first 3 years after delivery.
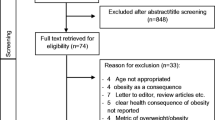
Methods
The World Health Organization Quality of Life (WHOQOL)-bref scores were compared and correlated with maternal and infant-related sociodemographic and clinical variables at maternal discharge (T0) and at 6 (T1), 12 (T2), 24 (T3), and 36 (T4) months after delivery. Multiple linear regression models were fitted to investigate the effect of these variables on the mothers’ QoL.
Results
The WHOQOL-BREF physical domain scores were higher at T1 and T2 compared to T0 (p = 0.013). Maternal variables that contributed to maternal QoL scores (p < 0.05) were stable marital union (b = 13.60; T0), family income (b = −12.75; T3), Evangelical religion (b = 8.11; T4), and beck depression inventory (BDI) score (−1.42 ≤ b ≤ −0.36; T0, T1, T2, T3, and T4). Infants’ variables that most affected maternal QoL (p < 0.05) were posthemorrhagic hydrocephalus (PHH) (−18.84 ≤ b ≤ −10.05; T1, T2, and T4), bronchopulmonary dysplasia (BPD) (b = −7.41; T2), female gender (b = 8.09; T2), and SNAPPE severity score (b = −0.23; T3).
Conclusion
Mothers of preterm infants with VLBW exhibited transient improvements in physical well-being during the first year after delivery. The presence of depressive symptoms in mothers and the diagnosis of PHH or BPD were negatively associated with QoL. Social, religious, and economic aspects were also important factors for the QoL of mothers of preterm infants with VLBW.

Similar content being viewed by others
Abbreviations
- WHOQOL-BREF :
-
World Health Organization quality of life–bref assessment
- BDI:
-
Beck depression inventory
- PHH:
-
Posthemorrhagic hydrocephalus
- BPD:
-
Bronchopulmonary dysplasia
- SNAPPE:
-
Score for neonatal acute physiology with perinatal extension
- VLBW:
-
Very low birth weight
References
Blencowe, H., Cousens S., Chou, D., Oestergaard, M., Says L., Moller A., et al. (2013). Born too soon: The global epidemiology of 15 million preterm births. Reproductive Health. http://www.reproductive-health-journal.com/content/10/S1/S2.
Russell, R. B., Green, N. S., Steiner, C. A., Meikle, S., Howse, J. L., Poschman, K., et al. (2007). Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics, 120, e1–e9.
Behrman R. E., & Butler A. S. (Eds.) (2007). Preterm birth: Causes, consequences, and prevention, Editors Committee on understanding premature birth and assuring healthy outcomes (Chapter 12, pp. 398–429).
Baumgardt, M., Bucher, H. U., Mieth, R. A., & Fauchére, J. C. (2012). Health-related quality of life of former very preterm infants in adulthood. Acta Paediatrica, 101(2), e59–e63.
Van Lunenburg, A., van der Pal, S. M., van Dommelen, P., van der Pal, K. M., Bennebroek, J., & Verrips, G. H. W. (2013). Changes in quality of life into adulthood after very preterm birth and/or very low birth weight in the Netherlands. Health and Quality of Life Outcomes, 11, 51.
Van Lerberghe, W., Manuel, A., Matthews, Z., & Wolfhein, C. (2005). Mothers and children matter so does their health in The World Health Report 2005: Make mother and child count. WHO press, Geneva (Chapter 1, pp. 25–44).
Hill, P. D., & Aldag, J. C. (2007). Maternal perceived quality of life following childbirth. Journal of Obstetrics, Gynecologic and Neonatal Nursing, 36, 328–334.
Darcy, J. M., Grywacz, J. G., Stephens, L. S., Leng, I., Clinch, R., & Arcury, T. A. (2011). Maternal depressive symptomatology: 16-month follow-up of infant and maternal health-related quality of life. Journal of the American Board of Family Medicine, 24(3), 249–257.
Eiser, C., Eiser, J. R., Mayhew, A. G., & Gibson, A. T. (2005). Parenting the premature infant: Balancing vulnerability and quality of life. Journal of Child Psychology and Psychiatry, 46(11), 1169–1177.
Witt, W. P., Litzelman, K., Spear, H. A., Wisk, L. E., Levin, N., McManus, B. M., et al. (2012). Mothers of very low birth weight children at school age: Quality of life outcomes from the Newborn Lung Project Statewide Cohort Study. Quality of Life Research, 21(9), 1565–1576.
Sohi, I., & Sharma, M. (2007). Quality of life of mothers of preterm and term babies. Journal of Neonatology [s.l.], 21(4), 281–284.
Donohue, P. K., Maurin, E., Kimzey, L., Allen, M. C., & Strobino, D. (2008). Quality of life of caregivers of very low-birthweight infants. Birth, 35(3), 212–219.
Stern, C., Trapp, E., Mautner, E., Deustch, M., Lang, U., & Cervar-Zivkovic, M. (2014). The impact of severe preeclampsia on maternal quality of life. Quality of Life Research, 23, 1019–1026.
Luu, T. M., Ment, L. R., Schneider, K. C., Katz, K. H., Allan, W. C., & Vohr, B. R. (2009). Lasting effects of preterm birth and neonatal brain hemorrhage at 12 years of age. Pediatrics, 123, 1037–1044.
McLean, A., Townsend, A., Clark, J., Sawyer, M. G., Baghurst, P., Haslam, R., et al. (2000). Quality of life of mothers and families caring for preterm infants requiring home oxygen therapy: A brief report. Journal of Paediatrics and Child Health, 36, 440–444.
Lee, C. F., Hwang, F. M., Chen, C. J., & Chien, L. Y. (2009). The interrelationships among parenting stress and quality of life of the caregiver and preschool child with very low birth weight. Family and Community Health, 32(3), 228–237.
Gorenstein, C., & Andrade, L. (1996). Validation of a Portuguese version of the beck depression inventory and the state-trait anxiety inventory in Brazilian subjects. Brazilian Journal of Medical and Biological Research, 29, 453–457.
Cunha, J. A. (2001). Manual da versão em português das Escalas Beck. São Paulo: Casa do Psicólogo.
Beck, A. T., Ward, C. H., Mendelson, M., Mick, J., & Erbaugh, G. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571.
Steer, R. A., Beck, A. T., Brown, G., & Berchick, R. J. (1987). Self-reported depressive symptoms that differentiate recurrent episode major depression from dysthymic disorders. Journal of Clinical Psychology, 43(2), 246–250.
Richardson, D. K., Corcoran, J. D., Escobar, G. J., & Lee, S. K. (2001). SNAP-II e SNAPPE-II: simplified newborn illness severity and mortality risk scores- the Canadian NICU network, the kaiser permanent neonatal minimum data set wide area network, and the SNAP-II study group. The Journal of Pediatrics, 138(1), 92–100.
Silveira, R. C., Schelbendorff, M., & Procianoy, R. S. (2001). Valor preditivo dos escores de SNAP e SNAP-PE na mortalidade neonatal. Jornal de Pediatria, 77(6), 455–460.
Capurro, H., Konichezky, S., Fonseca, D., & Caldeyrp-Barcia, R. (1978). A simplified method for diagnosis of gestational age in the newborn infant. Journal of Pediatrics, 93, 120–122.
Ballard, J. L., Khoury, J. C., Wedig, K., Wang, L., Eilers-Walsman, B. L., & Lipp, R. (1991). New Ballard Score, expanded to include extremely premature infants. Journal of Pediatrics, 119, 417–423.
Battaglia, F. C., & Lubchenco, L. O. (1967). A practical classification of newborn infants by weight and gestational age. Journal of Pediatrics, 71, 159–163.
Twickler, D. M., Reichel, T., McIntire, D. D., Magee, K. P., & Ramus, R. M. (2002). Fetal central nervous system and cistern magna measurements by magnetic ressonance imaging. American Journal of Obstetrics and Gynecology, 187, 927–931.
Zin, A., Florêncio, T., Fortes Filho, J. B., Nakanami, C. R., Gianini, N., Graziano, R. M., et al. (2007). Proposta de diretrizes brasileiras do exame e tratamento de retinopatia da prematuridade (ROP). Arquivos Brasileiros de Oftalmologia, 70(5), 875–883.
Jobe, A. H., & Bancalari, E. (2001). Bronchopulmonary dysplasia. American Journal of Respiratory and Critical Care, 163, 1723–1729.
Friedrich, L., Corso, A. L., & Jones, M. H. (2005). Prognóstico pulmonar em prematuros. Jornal de Pediatria, 81(S1), S79–S88.
Frankenburg, W. K., Dodds, J., Archer, P., Shapiro, H., & Bresnick, B. (1992). The Denver II: A major revision and restandardization of the Denver developmental screening test. Pediatrics, 89, 91–97.
Fleck, M. P. A., Fachel, O., Xavier, M., Chachamovich, E., Vieira, G., Santos, L., et al. (1999). Desenvolvimento da versão em português do instrumento de avaliação de qualidade de vida da OMS (WHOQOL-100). Revista Brasileira de Psiquiatria, 21(1), 19–28.
Fleck, M. P. A., Fachel, O., Xavier, M., Chachamovich, E., Vieira, G., Santos, L., et al. (1999). Aplicação da versão em português do instrument de avaliação de qualidade de vida da organização mundial da saúde (WHOQOL-100). Revista de Saúde Pública, 33, 198–205.
Webster, J., Nicholas, C., Velacortt, C., Cridland, N., & Fawcett, L. (2010). Validation of the WHOQOL-BREF among women following childbirth. Australian and New Zealand Journal of Obstetrics and Gynaecology, 50, 132–137.
Fleck, M. P. A., Louzada, S., Xavier, M., Chachamovich, E., Vieira, G., Santos, et al. (2000). Aplicação da versão em português do instrumento abreviado de avaliação de QV “WHOQOL-bref”. Revista de Saúde Pública, São Paulo, 34(2), 178–183.
Terwee, C. B., Bot, S. D. M., Boer, M. R., van der Windt, D. A. W. M., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60, 34–42.
Cliff, N. (1993). Dominance statistics: Ordinal analyses to answer ordinal questions. Psychological Bulletin, 114, 494–509.
Belsley, D. A., Kuh, E., & Welsch, R. E. (1980). Regression diagnostics., Wiley series in probability and mathematical statistics London: Wiley.
Cheng, C. Y., & Li, Q. (2008). Integrative review of research on general health status and prevalence of common physical health conditions of women after childbirth. Women’s Health, 18(4), 267–280.
Feeley, N., Zelkowitz, P., Cormie, C., Charbonneau, L., Lacroix, A., & Papageorgiou, A. (2011). Posttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal care unit. Applied Nursing Research, 24, 114–117.
Favaro, M. S. F., Peres, R. S., & Santos, M. A. (2012). Avaliação do impacto da prematuridade na saúde mental de puérperas. Psico-USF, 17(3), 457–465.
Webb, D. A., Bloch, J. R., Coyne, J. C., Chung, E. K., Bennett, I. M., & Culhane, J. F. (2008). Postpartum physical symptoms in new mothers: Their relationship to functional limitations and emotional well-being. Birth, 35, 179–187.
Mortazavi, F., Mousavi, S. A., Chaman, R., & Khousravi, A. (2014). Maternal quality of life during the transition to motherhood. Iranian Red Crescent Medicine Journal, 16(5), e8443.
Carvalho, A. E. V., Martinez, F. E., & Linhares, M. B. M. (2008). Maternal anxiety and depression and development of prematurely born infants in the first year of life. The Spanish Journal of Psychology, 11(2), 600–608.
Singer, L. T., Salvator, A., Guo, S., Collin, M., Lilien, L., & Baley, J. (1999). Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. Journal of the American Medical Association, 281(9), 799–805.
Gray, P. H., Edwards, D. M., O’Callaghan, M. J., & Cuskelly, M. (2012). Parenting stress in mothers of preterm infants during early infancy. Early Human Development, 88, 45–49.
Rojas, G., Fristsch, R., Solis, G. J., Gonzalez, M., Guajardo, V., & Araya, R. (2006). Calidad de vida de mujeres deprimidas em el parto. Revista Médica de Chile, 134, 713–720.
Zubaran, C., & Foresti, K. (2011). Investing quality of life and depressive symptoms in the postpartum period. Women and Birth, 24(1), 10–16.
Sadat, S., Abedzadeh-Kalahroudi, M., Atrian, M. K., Karamian, Z., & Sooki, Z. (2014). The impact of postpartum depression on quality of life in women after child’s birth. Iranian Red Crescent Medicine Journal, 16(2), e14995.
Minkovitz, C. S., Stropino, D., Hou, W., Miller, T., Misty, K. B., & Svartz, K. (2005). Maternal depressive symptoms and children’s receipt health care in the first 3 years of life. Pediatrics, 115(2), 1–15.
Robinson, S. (2012). Neonatal posthemorrhagic hydrocephalus from prematurity: Pathophysiology and current treatment concepts: A review. Journal of Neurosurgery Pediatrics. doi:10.3171/2011.12.peds11136.
Radic, J. A. E., Vincer, M., & McNeely, D. (2015). Outcomes of intraventricular hemorrhage and posthemorragic hydrocephalus in a population-based cohort of very preterm infants borns to residents of Nova Scotia from 1993–2010. Journal Neurosurgery Pediatrics, 15, 580–588.
Paulsen, A. H., Lundar, T., & Lindegaard, K. F. (2015). Pediatric hydrocephalus: 40-year outcomes in 128 hydrocephalic patients treated with shunts during childhood. Assessment of surgical outcome, work participation, and health-related quality of life. Journal of Neurosurgery Pediatrics, 16, 633–641.
Suguihara, C., & Lessa, A. C. (2005). Como minimizar a lesão pulmonar no prematuro extremo: propostas. Jornal de Pediatria, 81(1), S69–S78.
Landry, J. S., Chan, T., Lands, L., & Menzies, D. (2011). Long-term impact of bronchopulmonary dysplasia on pulmonar function. Canadian Respiratory Journal, 18(5), 265–270.
Baraldi, E., & Filippone, M. (2007). Chronic lung disease after premature birth. New England Journal Medicine, 357, 1946–1955.
Feeley, C. A., Turner-Henson, A., Christian, B. J., Avis, K. T., Heaton, K., Lozano, D., et al. (2014). Sleep quality, stress, caregivers burden and quality of life in maternal caregivers of young children with Bronchopulmonary Dysplasia. Journal of Pediatrics Nursing, 29, 29–38.
Smith, V. C., Zupancic, J. A. F., McCormick, M. C., Croen, L. A., Greene, J., Escobar, G. J., et al. (2004). Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. The Journal of Pediatrics, 144, 799–803.
Mcgrath-Morrow, S. A., Timothy, R., Rickert, K., Lefton-Greif, M., Eakin, M., & Collaco, J. M. (2012). The impact of bronchopulmonary dysplasia on caregiver health related quality of life during the first 2 years of life. Pediatric Pulmonology. doi:10.1002/ppul.22687wileyonlinelibray.com.
Grouthuis, J. R., & Makari, D. (2012). Definition and outpatient management of the very low-birth-weight infant with bronchopulmonary dysplasia. Advances in therapy. www.advancesintherapy.com. Accessed 16 April 2012. doi 10.1007/s12325-012-0015-y.
Zanardo, V., & Freato, F. (2001). Home oxygen therapy in infants with bronchopulmonary dysplasia: Assessment of parental anxiety. Early Human Development, 65, 39–46.
Cairney, J., Boyle, M., Offord, D. R., & Racine, Y. (2003). Stress, social support and depression in single and married mothers. Social Psychiatry Epidemiology, 38, 442–449.
Copeland, D., & Harbaugh, B. L. (2005). Differences in parenting stress between married and single first time mothers at six to eight weeks after birth. Issues Comprehensive Pediatric Nursing, 28(3), 139–152.
Rani, N. I. (2006). Childcare by poor single mothers: Study of mother-headed families in India. Journal of Comparative Family Studies, 37(1), 75–95.
Edwards, D. M., Gibbons, K., & Gray, P. H. (2016). Relationship quality for mothers of very preterm infants. Early Human Development, 92, 13–18.
Censo. (2010). Número de católicos cai e aumenta o de evangélicos, espíritas e sem religião. http://www.ibge.gov.br/home/presidencia/noticias/noticia_visualiza.php?id_noticia=2170&id_pagina=1&titulo=Censo-2010:-numero-de-catolicos-cai-e-aumenta-o-de-evangelicos,-espiritas-e-sem-religiao. Accessed 09 May 2016.
Sloan, R. P., Bagiella, E., & Powell, T. (1999). Religion, spirituality and medicine. The Lancet, 353, 664–667.
Bertachini, L., & Pessini, L. (2010). A importância da dimensão espiritual na prática dos cuidados paliativos. Revista Bioethikos-Centro Universitário São Camilo, 4(3), 315–323.
Brelsford, G. M., & Doheny, K. K. (2016). Religious and spiritual journeys: Brief reflections from mothers and fathers in a Neonatal Intensive Care Unit (NICU). Pastor Psychology, 63, 76–87. doi:10.1007/s11089-015-0673-1.
De Tycker, C., Briançon, S., Lighezzolo, J., Spitz, E., Kabuth, B., Deluigi, V., et al. (2008). Quality of life, postnatal depression and baby gender. Journal of Clinical Nursing, 17, 312–322.
Leung, S., Arthur, D., & Martison, I. (2005). Stress in women with postpartum depression: Phenomenological study. Journal of Advanced Nursing, 51, 353–360.
Patel, V., Rodrigues, M., & De Souza, N. (2002). Gender, poverty and postnatal depression: A study of mothers in Goa, India. American Journal of Psychiatry, 159, 43–47.
Acknowledgements
We thank the participating mothers, without whom this study could not have been conducted, as well as Celine Vieira, psychologist at the neonatology service at the time of data collection, for her indispensable help in the acquisition of materials and training in the assessment of the Denver II Developmental Test.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Moura, M.R.S., Araújo, C.G.A., Prado, M.M. et al. Factors associated with the quality of life of mothers of preterm infants with very low birth weight: a 3-year follow-up study. Qual Life Res 26, 1349–1360 (2017). https://doi.org/10.1007/s11136-016-1456-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1456-6