Abstract
Purpose
Esophageal atresia (EA) is a rare congenital malformation requisite of surgical treatment. Survival rates have significantly increased in recent decades, but treated children are at risk of chronic morbidity. This study aims to review the literature on health-related quality of life (HRQOL) in patients with EA and describe the questionnaires used.
Methods
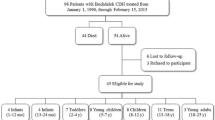
A literature search was conducted in Pubmed, Cinahl and PsycINFO, from inception to January 2015. A meta-analysis of studies investigating HRQOL in patients with EA compared to healthy references was performed. The effect size was calculated as Cohen’s d.
Results
Twelve articles (published 1995–2014) describing HRQOL among children, young people and adults were identified. Only European studies were found, and these had variable sample sizes (8–128). Overall HRQOL was reported to be reduced in five of the seven studies that compared overall HRQOL with a healthy reference population. Impaired physical or general health was described in eight articles. In the meta-analysis, eight eligible studies provided 16 estimates of the effect of EA, six of which reached statistical significance for worse HRQOL (p < 0.05). Using Cohen’s criteria, the pooled estimate of the effect of EA was small for overall and physical HRQOL, and <0.2 for the mental and social HRQOL components. Altogether, 15 different questionnaires were used, and none were condition specific for EA.
Conclusions
Different findings are reported; however, this study suggests that patients with EA may have a reduced HRQOL. Moreover, HRQOL is not adequately measured in this group. Additional research is required.



Similar content being viewed by others
Abbreviations
- EA:
-
Esophageal atresia, an interrupted esophagus without any connection to the stomach
- CHQ:
-
Child Health Questionnaire
- CI:
-
Colon interposition for esophageal replacement
- ES:
-
Effect size
- EORTC:
-
European Organization into Research and Treatment of Cancer
- GER:
-
Gastro-esophageal reflux
- GERD:
-
Gastro-esophageal reflux disease
- GIQLI:
-
Gastro Intestinal Quality of Life Index
- GT:
-
Gastric transposition for esophageal replacement
- HRQOL:
-
Health-related quality of life
- ICQ:
-
Illness Cognition Questionnaire
- KPS:
-
Karnofsky Performance Status
- MCS:
-
Mental component summary
- PEDSQL:
-
Pediatric Quality of Life Inventory
- PCS:
-
Physical component summary
- RSRQLI:
-
Respiratory Symptoms-Related Quality of Life Index
- SAC:
-
Scientific Advisory Committee of the Medical Outcomes Trust
- SAQ:
-
Strategy and Attribution Questionnaire
- SF-36:
-
36-Item Short Form Survey from the RAND Medical Outcomes Study
- Spitzer QL Index:
-
Spitzer Quality of Life Index
- TEF:
-
Tracheoesophageal fistula, a connection between the esophagus and the windpipe
- VAS/Uniscale:
-
Visual Analogue Scale/Uniscale for overall HRQOL
- WHO-5:
-
World Health Organization-5 Well-Being Index
References
Wang, B., Tashiro, J., Allan, B. J., Sola, J. E., Parikh, P. P., Hogan, A. R., et al. (2014). A Nationwide analysis of clinical outcomes among newborns with esophageal atresia and tracheoesophageal fistulas. Journal of Surgical Research, 186(2), 604–612.
Oddsberg, J., Lu, Y., & Lagergren, J. (2012). Aspects of esophageal atresia in a population-based setting: incidence, mortality, and cancer risk. Pediatric Surgery International, 28(3), 249–257.
Sfeir, R., Piolat, C., Lemelle, J. L., Petit, T., Lavrand, F., Becmeur, F., et al. (2013). Esophageal atresia: Data from a national cohort. Journal of Pediatric Surgery, 48(8), 1664–1669.
Gross, R. E. (1953). The surgery of infancy and childhood. Philadelphia: WB Saunders.
Vogt, E. C. (1929). Congenital esophageal atresia. American Journal of Roentgenology, 22, 463–465.
Lilja, H. E., & Wester, T. (2008). Outcome in neonates with esophageal atresia treated over the last 20 years. Pediatric Surgery International, 24(5), 531–536.
Tovar, J. A., Diez Pardo, J. A., Murcia, J., Prieto, G., Molina, M., & Polanco, I. (1995). Ambulatory 24-hour manometric and pH metric evidence of permanent impairment of clearance capacity in patients with esophageal atresia. Journal of Pediatric Surgery, 30(8), 1224–1231.
Sistonen, S. J., Koivusalo, A., Nieminen, U., Lindahl, H., Lohi, J., Kero, M., et al. (2010). Esophageal morbidity and function in adults with repaired esophageal atresia with tracheoesophageal fistula: a population-based long-term follow-up. Annals of Surgery, 251(6), 1167–1173.
Koivusalo, A., Pakarinen, M. P., & Rintala, R. J. (2007). The cumulative incidence of significant gastrooesophageal reflux in patients with oesophageal atresia with a distal fistula-a systematic clinical, pH-metric, and endoscopic follow-up study. Journal of Pediatric Surgery, 42(2), 370–374.
Spitz, L. (2006). Esophageal atresia. Lessons I have learned in a 40-year experience. Journal of Pediatric Surgery, 41(10), 1635–1640.
Gottrand, F., Sfeir, R., Coopman, S., Deschildre, A., & Michaud, L. (2008). Outcome of children with repaired oesophageal atresia. Archives de Pediatrie, 15(12), 1837–1842.
Malmstrom, K., Lohi, J., Lindahl, H., Pelkonen, A., Kajosaari, M., Sarna, S., et al. (2008). Longitudinal follow-up of bronchial inflammation, respiratory symptoms, and pulmonary function in adolescents after repair of esophageal atresia with tracheoesophageal fistula. Journal of Pediatrics, 153(3), 396–401.
Sistonen, S., Malmberg, P., Malmstrom, K., Haahtela, T., Sarna, S., Rintala, R. J., & Pakarinen, M. P. (2010). Repaired oesophageal atresia: Respiratory morbidity and pulmonary function in adults. The European Respiratory Journal, 36(5), 1106–1112.
Gatzinsky, V., Wennergren, G., Jönsson, L., Ekerljung, L., Houltz, B., Redfors, S., et al. (2014). Impaired peripheral airway function in adults following repair of esophageal atresia. Journal of Pediatric Surgery, 49(9), 1347–1352.
Chetcuti, P., & Phelan, P. D. (1993). Respiratory morbidity after repair of oesophageal atresia and tracheo-oesophageal fistula. Archives of Disease in Childhood, 68(2), 167–170.
Little, D. C., Rescorla, F. J., Grosfeld, J. L., West, K. W., Scherer, L. R., & Engum, S. A. (2003). Long-term analysis of children with esophageal atresia and tracheoesophageal fistula. Journal of Pediatric Surgery, 38(6), 852–856.
Gatzinsky, V., Jönsson, L., Ekerljung, L., Friberg, L. G., & Wennergren, G. (2011). Long-term respiratory symptoms following oesophageal atresia. Acta Paediatrica, 100(9), 1222–1225.
Stoll, C., Alembik, Y., Dott, B., & Roth, M. P. (2009). Associated malformations in patients with esophageal atresia. European Journal of Medical Genetics, 52(5), 287–290.
Chittmittrapap, S., Spitz, L., Kiely, E. M., & Brereton, R. J. (1989). Oesophageal atresia and associated anomalies. Archives of Disease in Childhood, 64(3), 364–368.
Engum, S. A., Grosfeld, J. L., West, K. W., Rescorla, F. J., & Scherer, L. R. (1995). Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over two decades. Archives of Surgery, 130(5), 502–508.
Seid, M., Varni, J. W., Segall, D., & Kurtin, P. S. (2004). Health-related quality of life as a predictor of pediatric healthcare costs: A two-year prospective cohort analysis. Health and Quality of Life Outcomes,. doi:10.1186/1477-7525-2-48.
Ahmed, S., Berzon, R. A., Revicki, D. A., Lenderking, W. R., Moinpour, C. M., Basch, E., et al. (2012). The use of patient-reported outcomes (PRO) within comparative effectiveness research: Implications for clinical practice and health care policy. Medical Care, 50(12), 1060–1070.
Santana, M. J., & Feeny, D. (2014). Framework to assess the effects of using patient-reported outcome measures in chronic care management. Quality of Life Research, 23(5), 1505–1513.
Wilson I. B., & Cleary P. D. (1995). Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. Journal of American Medical Association, 273(1), 59–65.
Guyatt, G. H., Feeny, D. H., & Patrick, D. L. (1993). Measuring health-related quality of life. Annals of Internal Medicine, 15, 118(8), 622–629.
World Health Organization Quality of Life Group. (1997). WHOQOL measuring quality of life. Division of Mental Health and Prevention of Substance Abuse, World Health Organization. http://www.who.int/mental_health/media/68.pdf.
Testa, M. A., & Simonson, D. C. (1996) Assessment of quality-of-life outcomes. The New England Journal of Medicine, 28, 334(13), 835–840.
Aaronson, N., Alonso, J., Burnam, A., Lohr, K. N., Patrick, D. L., Perrin, E., & Stein, R. E. (2002). Assessing health status and quality-of-life instruments: Attributes and review criteria. Quality of Life Research, 11(3), 193–205.
Fayers, P. M., & Machin, D. (2007). Quality of Life: The assessment, analysis and interpretation of patient-reported outcomes. Chichester: Wiley.
Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560.
Landgraf, J. L., Abetz, L., & Ware, J. E. (1996). The CHQ user’s manual. Boston: The Health Institute, New England Medical Center.
Raat, H., Landgraf, J. M., Bonsel, G. J., Gemke, R. J., & Essink-Bot, M. L. (2002). Reliability and validity of the child health questionnaire-child form (CHQ-CF87) in a Dutch adolescent population. Quality of Life Research, 11(6), 575–581.
Raat, H., Bonsel, G. J., Essink-Bot, M. L., Landgraf, J. M., & Gemke, R. J. (2002). Reliability and validity of comprehensive health status measures in children: The Child Health Questionnaire in relation to the Health Utilities Index. Journal of Clinical Epidemiology, 55(1), 67–76.
Landgraf, J. M., Maunsell, E., Nixon, Speechley K., Bullinger, M., Campbell, S., Abetz, L., & Ware, J. E. (1998). Canadian-French, German and UK versions of the Child Health Questionnaire: methodology and preliminary item scaling results. Quality of Life Research, 7(5), 433–445.
Waters, E. B., Salmon, L. A., Wake, M., Wright, M., & Hesketh, K. D. (2001). The health and well-being of adolescents: A school-based population study of the self-report Child Health Questionnaire. The Journal of Adolescent Health, 29(2), 140–149.
Westendorp, T., Verbunt, J. A., Remerie, S. C., & Smeets, R. J. (2014). Responsiveness of the Child Health Questionnaire-Parent Form in adolescents with non-specific chronic pain or fatigue. European Journal of Pain, 18(4), 540–547.
Nixon, Speechley K., Maunsell, E., Desmeules, M., Schanzer, D., Landgraf, J. M., Feeny, D. H., & Barrera, M. E. (1999). Mutual concurrent validity of the Child Health Questionnaire and the Health Utilities Index: An exploratory analysis using survivors of childhood cancer. International Journal of Cancer, 83(12), 95–105.
Ruperto, N., Ravelli, A., Pistorio, A., Malattia, C., Cavuto, S., Gado-West, L., et al. (2001). Cross-cultural adaptation and psychometric evaluation of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) in 32 countries. Review of the general methodology. Clinical and Experimental Rheumatology, 19(4), 1–9.
Ravens-Sieberer, U., Auquier, P., Erhart, M., Gosch, A., Rajmil, L., Bruil, J., et al. (2007). The KIDSCREEN-27 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Quality of Life Research, 16(8), 1347–1356.
Detmar, S. B., Bruil, J., Ravens-Sieberer, U., Gosch, A., Bisegger, C., & European KIDSCREEN group. (2006). The use of focus groups in the development of the KIDSCREEN HRQL questionnaire. Quality of Life Research, 15(8), 1345–1353.
Jafari, P., Bagheri, Z., & Safe, M. (2012). Item and response-category functioning of the Persian version of the KIDSCREEN-27: Rasch partial credit model. Health & Quality of Life Outcomes,. doi:10.1186/1477-7525-10-127.
Bagheri, Z., Jafari, P., Tashakor, E., Kouhpayeh, A., & Riazi, H. (2014). Assessing whether measurement invariance of the KIDSCREEN-27 across child-parent dyad depends on the child gender: A multiple group confirmatory factor analysis. Global Journal of Health Science, 6(5), 142–153.
Robitail, S., Raavens-Sieberer, U., Simeoni, M. C., Rajmil, Bruil, J., Power, M., et al. (2007). Testing the Structural and Cross-Cultural Validity of the KIDSCREEN-27 Quality of Life Questionnaire. Quality of Life Research, 16(8), 1335–1345.
Ravens, Sieberer U., Herdman, M., Devine, J., Otto, C., Bullinger, M., Rose, M., & Klasen, F. (2014). The European KIDSCREEN approach to measure quality of life and well-being in children: Development, current application, and future advances. Quality of Life Research, 23(3), 791–803.
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). PedsQL™ 4.0: Reliability and Validity of the Pediatric Quality of Life Inventory™ Version 4.0 generic core scales in healthy and patient populations. Medical Care, 39(8), 800–812.
Varni, J. W., Seid, M., Knight, T. S., Uzark, K., & Szer, I. S. (2002). The PedsQLTM 4.0 Generic Core Scales: Sensitivity, responsiveness, and impact on clinical decision-making. Journal of Behavioral Medicine, 25(2), 175–193.
Varni, J. W., Seid, M., Smith, Knight T., Burwinkle, T., Brown, J., & Szer, I. S. (2002). The PedsQL in pediatric rheumatology: Reliability, validity, and responsiveness of the Pediatric Quality of Life Inventory Generic Core Scales and rheumatology module. Arthritis and Rheumatism, 46(3), 714–725.
Varni, J. W., Burwinkle, T. M., Seid, M., & Skarr, D. (2003). The PedsQL™ 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambulatory Pediatrics, 3(6), 329–341.
Connelly, M., & Rapoff, M. A. (2006). Assessing health-related quality of life in children with recurrent headache: Reliability and validity of the PedsQLTM 4.0 in a pediatric headache sample. Journal of Pediatric Psychology, 31(7), 698–702.
Petersen, S., Hägglof, B., Stenlund, H., & Bergstrom, E. (2009). Psychometric properties of the Swedish PedsQL, Pediatric Quality of Life Inventory 4.0 generic core scales. Acta Paediatrica, 98(9), 1504–1512.
Varni, J. W. (2014). Available translations of the PedsQLTM Scales and Modules: PedsQL Existing Translations. MAPI Research Trust. http://www.pedsql.org/PedsQL-Translation-Tables.pdf.
Ware, J. E., Jr, Gandek, B., & for the IQOLA Project. (1998). Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. Journal of Clinical Epidemiology, 51(11), 903–991.
Gandek, B., Ware, J. E., Aaronson, N. K., Apolone, G., Bjorner, J. B., Brazier, J. E., et al. (1998). Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. Journal of Clinical Epidemiology, 51(11), 1171–1178.
Ware, J. E., Jr. (2000). SF-36 health survey update. Spine, 25(24), 3130–3139.
Tarlov, A. R., Ware, J. E., Jr., Greenfield, S., Nelson, E. C., Perrin, E., & Zubkoff, M. (1989). The Medical outcomes study. An application of methods for monitoring the results of medical care. Journal of American Medical Association, 262(7), 925–930.
Stewart, A. L., Greenfield, S., Hays, R. D., Wells, K., Rogers, W. H., Berry, S. D., McGlynn, E. A., & Ware, J. E. Jr. (1989). Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. Journal of American Medical Association, 262(7), 907–913.
Spitzer, W. O., Dobson, A. J., Hall, J., Chesterman, E., Levi, J., Shepherd, R., et al. (1981). Measuring the quality of life of cancer patients: A concise QL-index for use by physicians. Journal of Chronic Diseases, 34(12), 585–597.
Greimel, E., Thiel, I., Peintinger, F., Cegnar, I., & Pongratz, E. (2002). Prospective assessment of quality of life of female cancer patients. Gynecologic Oncology, 85(1), 140–147.
Coates, A., Thomson, D., McLeod, G. R., Hersey, P., Gill, P. G., Olver, I. N., et al. (1993). Prognostic value of quality of life scores in a trial of chemotherapy with or without interferon in patients with metastatic malignant melanoma. European Journal of Cancer, 29(12), 1731–1734.
Selby, P. J., Chapman, J. A., Etazadi-Amoli, J., Dalley, D., & Boyd, N. F. (1984). The development of a method for assessing the quality of life of cancer patients. British Journal of Cancer, 50(1), 13–22.
Ballatori, E., Porzio, G., Roila, F., Ruggeri, B., Mattei, A., & Cortesi, E. (2007). Is there still a role for the uniscale assessment of quality of life? Tumori, 93(1), 78–81.
Sloan, J. A., Loprinzi, C. L., Kuross, S. A., Miser, A. W., O’Fallon, J. R., Mahoney, M. R., et al. (1998). Randomized comparison of four tools measuring overall quality of life in patients with advanced cancer. Journal of Clinical Oncology, 16(11), 3662–3673.
Bradburn, N. M. (1969). The structure of psychological well-being. Chicago: Aldine Publishing Co.
Harding, S. D. (1982). Psychological well-being in Great Britain: An evaluation of the Bradburn Affect Balance Scale. Personality and Individual Differences, 3(2), 167–175.
Kim, K. A., & Mueller, D. J. (2001). To Balance or not to Balance: Confirmatory Factor Analysis of the Affect-Balance Scale. Journal of Happiness Studies, 2(3), 289–306.
Stacey, C. A., & Gatz, M. (1991). Cross-sectional age differences and longitudinal change on the Bradburn Affect Balance Scale. Journal of Gerontology, 46(2), 76–78.
Gerald, M. D., Morton, B., Rene, D., Luc, G. P., & Edwards, R. G. (1997). Cross-cultural measurements of psychological well-being: The psychometric equivalence of Cantonese, Vietnamese, and Laotian translations of the affect balance scale. American Journal of Public Health, 87(5), 794–799.
Koivusalo, A., Pakarinen, M. P., Turunen, P., Saarikoski, H., Lindahl, H., & Rintala, R. J. (2005). Health-related quality of life in adult patients with esophageal atresia—a questionnaire study. Journal of Pediatric Surgery, 40(2), 307–312.
Evers, A. W., Kraaimaat, F. W., van Lankveld, W., Jongen, P. J., Jacobs, J. W., & Bijlsma, J. W. (2001). Beyond unfavorable thinking: The illness cognition questionnaire for chronic diseases. Journal of Consulting and Clinical Psychology, 69(6), 1026–1036.
Lauwerier, E., Crombez, G., Van Damme, S., Goubert, L., Vogelaers, D., & Evers, A. W. (2010). The construct validity of the illness cognition questionnaire: The robustness of the three-factor structure across patients with chronic pain and chronic fatigue. International Journal of Behavioral Medicine, 17(2), 90–96.
Yates, J. W., Chalmer, B., & McKegney, F. P. (1980). Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer, 45(8), 2220–2224.
Schag, C. C., Heinrich, R. L., & Ganz, P. A. (1984). Karnofsky performance status revisited: Reliability, validity, and guidelines. Journal of Clinical Oncology, 2(3), 187–193.
Nurmi, J. E., Salmela-Aro, K., & Haavisto, T. (1995). The Strategy and Attribution Questionnaire: Psychometric properties. European Journal of Psychological Assessment, 11(2), 108–121.
Zukauskiene, R., & Sondaite, J. (2004). The Strategy and Attribution Questionnaire: Psychometric properties of a Lithuanian translation in an adolescent sample. Scandinavian Journal of Psychology, 45(2), 157–162.
Bech, P. (2004). Measuring the dimension of psychological general well-being by the WHO-5. Quality of Life Newsletter, 32, 15–16.
Bonsignore, M., Barkow, K., Jessen, F., & Heun, R. (2001). Validity of the five-item WHO Well-Being Index (WHO-5) in an elderly population. European Archives of Psychiatry and Clinical Neuroscience, 251(2), 27–31.
Newnham, E. A., Hooke, G. R., & Page, A. C. (2010). Monitoring treatment response and outcomes using the World Health Organization’s Wellbeing Index in psychiatric care. Journal of Affective Disorders, 122(1–2), 133–138.
Blazeby, J. M., Williams, M. H., Brookes, S. T., Alderson, D., & Farndon, J. R. (1995). Quality of life measurement in patients with oesophageal cancer. Gut, 37(4), 505–508.
Blazeby, J. M, Alderson, D., Winstone, K., Steyn, R., Hammerlid, E., Arraras, J., & Farndon, J. R., on behalf of the EORTC Quality of Life Study Group. (1996). Development of an EORTC questionnaire module to be used in quality of life assessment for patients with oesophageal cancer. European Journal of Cancer, 32(11), 1912–1917.
Blazeby, J. M., Conroy, T., Hammerlid, E., Fayers, P., Sezer, O., Koller, M., Arraras, J., Bottomley, A., Vickery, C. W., Etienne, P. L., & Alderson, D. on behalf of the European Organisation for Research and Treatment of Cancer Gastrointestinal and Quality of Life Groups. (2003). Clinical and psychometric validation of an EORTC questionnaire module, the EORTC QLQ-OES18, to assess quality of life in patients with oesophageal cancer. European Journal of Cancer, 39(10), 1384–1394.
Eypasch, E., Wood-Dauphinee, S., Williams, J. I., Reinecke, K., Ure, B., & Neugebauer, E. (1990). Quality of life and gastrointestinal surgery—a clinimetric approach to developing an instrument for its measurement. Theoretical Surgery, 5(1–2), 3–10.
Eypasch, E., Williams, J. I., Wood-Dauphinee, S., Ure, B. M., Schmulling, C., Neugebauer, E., & Troidl, H. (1995). Gastrointestinal Quality of Life Index: Development, validation and application of a new instrument. The British Journal of Surgery, 82(2), 216–222.
Kamolz, T., Wykypiel, H., Bammer, T., & Pointner, R. (1998). Quality of life after laparoscopic antireflux surgery-Nissen fundoplication. Chirurg, 69(9), 947–950.
Sandblom, G., Videhult, P., Karlson, B. M., Wollert, S., Ljungdahl, M., Darkahi, B., et al. (2009). Validation of Gastrointestinal Quality of Life Index in Swedish for assessing the impact of gallstones on health-related quality of life. Value in Health, 12(1), 181–184.
Quintana, J. M., Cabriada, J., Lopez de Tejada, I., Varona, M., Oribe, V., Barrios, B., et al. (2001). Translation and validation of the gastrointestinal Quality of Life Index (GIQLI). Revista Espanola de Enfermedades Digestivas, 93(11), 693–706.
Ludman, L., & Spitz, L. (2003). Quality of life after gastric transposition for oesophageal atresia. Journal of Pediatric Surgery, 38(1), 53–57.
Peetsold, M. G., Heij, H. A., Deurloo, J. A., & Gemke, R. J. (2010). Health-related quality of life and its determinants in children and adolescents born with oesophageal atresia. Acta Paediatria, 99(3), 411–417.
Legrand, C., Michaud, L., Salleron, J., Neut, D., Sfeir, R., Thumerelle, C., et al. (2012). Long-term outcome of children with oesophageal atresia type III. Archives of Disease in Childhood, 97(9), 808–811.
Lepeytre, C., De Lagausie, P., Merrot, T., Baumstarck, K., Oudyi, M., & Dubus, J. C. (2013). Medium-term outcome, follow-up, and quality of life in children treated for type III esophageal atresia. Archives de Pédiatrie, 20(10), 1096–1104.
Dingemann, C., Meyer, A., Kircher, G., Boemers, T. M., Vaske, B., Till, H., & UreB, M. (2014). Long-term health-related quality of life after complex and/or complicated esophageal atresia in adults and children registered in a German patient support group. Journal of Pediatric Surgery, 49(4), 631–638.
Gatzinsky, V., Jonsson, L., Johansson, C., Gothberg, G., Sillen, U., & Friberg, L. G. (2011). Dysphagia in adults operated on for esophageal atresia-use of a symptom score to evaluate correlated factors. European Journal of Pediatric Surgery, 21(2), 94–98.
Deurloo, J. A., Ekkelkamp, S., Hartman, E. E., Sprangers, M. A., & Aronson, D. C. (2005). Quality of life in adult survivors of correction of esophageal atresia. Archives of Surgery, 140(10), 976–980.
Deurloo, J. A., Klinkenberg, E. C., Ekkelkamp, S., Heij, H. A., & Aronson, D. C. (2008). Adults with corrected oesophageal atresia: Is oesophageal function associated with complaints and/or quality of life? Pediatric Surgery International, 24(5), 537–541.
Ure, B. M., Slany, E., Eypasch, E. P., Weiler, K., Troidl, H., & Holschneider, A. M. (1998). Quality of life more than 20 years after repair of esophageal atresia. Journal of Pediatric Surgery, 33(3), 511–515.
Ure, B. M., Slany, E., Eypasch, E. P., Gharib, M., Holschneider, A. M., & Troidl, H. (1995). Long-term functional results and quality of life after colon interposition for long-gap oesophageal atresia. European Journal of Pediatric Surgery, 5(4), 206–210.
Burgos, L., Barrena, S., Andres, A. M., Martinez, L., Hernandez, F., Olivares, P., et al. (2010). Colonic interposition for esophageal replacement in children remains a good choice: 33-year median follow-up of 65 patients. Journal of Pediatric Surgery, 45(2), 341–345.
Bullinger, M. (1997). The challenge of cross-cultural quality of life assessment. Psychology & Health, 12(6), 815–825.
U.S. Department of Health and Human Services Food and Drug Administration. (2009). Guidance for industry: Patient-reported outcome measures: use in medical product development to support labeling claims: Draft guidance. Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) Center for Devices and Radiological Health (CDRH) http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf.
Wiebe, S., Guyatt, G., Weaver, B., Matijevic, S., & Sidwell, C. (2003). Comparative responsiveness of generic and specific quality-of-life instruments. Journal of Clinical Epidemiology, 56(1), 52–60.
Schmidt, S., & Bullinger, M. (2003). Current issues in cross-cultural quality of life instrument development. Archives of Physical Medicine and Rehabilitation, 84(4), 29–34.
Eiser, C., & Morse, R. (2001). Can parents rate their child’s health-related quality of life? Results of a systematic review. Quality of Life Research, 10(4), 347–357.
Eiser, C., & Jenney, M. (2007). Measuring quality of life. Archives of Disease in Childhood, 92(4), 348–350.
Matza, L. S., Swensen, A. R., Flood, E. M., Secnik, K., & Leidy, N. K. (2004). Assessment of health-related quality of life in children: A review of conceptual, methodological, and regulatory issues. Value in Health, 7(1), 79–92.
Acknowledgments
The study was funded by The Queen Silvia Children’s Foundation, The Mayflower Charity Foundation for Children, the Petter Silfverskiöld Memory Foundation and the Mary von Sydow Foundation.
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dellenmark-Blom, M., Chaplin, J.E., Gatzinsky, V. et al. Health-related quality of life among children, young people and adults with esophageal atresia: a review of the literature and recommendations for future research. Qual Life Res 24, 2433–2445 (2015). https://doi.org/10.1007/s11136-015-0975-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-0975-x