Abstract
Introduction
Longer lifespan and newer imaging protocols have led to more older adults being diagnosed with pituitary adenomas. Herein, we describe outcomes of patients ≥ 65 years undergoing endoscopic adenoma removal. To address selection criteria, we also assess a conservatively managed cohort.
Methods
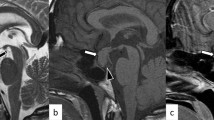
A retrospective analysis of 90-day outcomes of patients undergoing endoscopic pituitary adenomectomy from 2010 to 2019 by a neurosurgical/ENT team was performed. Tumor subtype, cavernous sinus invasion, extent of resection/early remission, endocrinology outcomes, complications, re-operations and readmissions were analyzed. A comparator cohort ≥ 65 years undergoing clinical surveillance without surgery was also analyzed.
Results
Of 468 patients operated on for pituitary adenoma, 123 (26%) were ≥ 65 years (range 65–93 years); 106 (86.2%) had endocrine-inactive adenomas; 18 (14.6%) had prior surgery. Of 106 patients with endocrine-inactive adenomas, GTR was achieved in 70/106 (66%). Of 17 patients with endocrine-active adenomas, early biochemical remission was: Cushing’s 6/8; acromegaly 1/4; prolactinomas 1/5. Gland function recovery occurred in 28/58 (48.3%) patients with various degrees of preoperative hypopituitarism. New anterior hypopituitarism occurred in 3/110 (2.4%) patients; permanent DI in none. Major complications in 123 patients were: CSF leak 2 (1.6%), meningitis 1 (0.8%), vision decline 1 (0.8%). There were no vascular injuries, operative hematomas, anosmia, deaths, MIs, or thromboembolic events. Median length of stay was 2 days. Readmissions occurred in 14/123 (11.3%) patients, 57% for delayed hyponatremia. Intra-cohort analysis by age (65–69, 70–74, 75–79, ≥ 80 years) revealed no outcome differences. Cavernous sinus invasion (OR 7.7, CI 1.37–44.8; p = 0.02) and redo-surgery (OR 8.5, CI 1.7–42.8; p = 0.009) were negative predictors for GTR/NTR. Of 105 patients evaluated for presumed pituitary adenoma beginning in 2015, 72 (69%) underwent surgery, 8 (7%) had prolactinomas treated with cabergoline and 25 (24%) continue clinical surveillance without surgery, including two on new hormone replacement.
Conclusion
This study suggests that elderly patients carefully selected for endoscopic adenoma removal can have excellent short-term outcomes including high resection rates, low complication rates and short length of stay. Our experience supports a multidisciplinary approach and the concept of pituitary centers of excellence. Based on our observations, approximately 25% of elderly patients with pituitary adenomas referred for possible surgery can be monitored closely without surgery.

Similar content being viewed by others
References
Bureau UC Older people projected to outnumber children. In: The United States Census Bureau. https://www.census.gov/newsroom/press-release/2018/cb18-41-population-projections.html. Accessed 18 May 2020
Ostrom QT, Gittleman H, Liao P et al (2017) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol 19:v1–v88. https://doi.org/10.1093/neuonc/nox158
Tjörnstrand A, Gunnarsson K, Evert M et al (2014) The incidence rate of pituitary adenomas in western Sweden for the period 2001–2011. Eur J Endocrinol 171:519–526. https://doi.org/10.1530/EJE-14-0144
Melmed S (2020) Pituitary-tumor endocrinopathies. N Engl J Med 382:937–950. https://doi.org/10.1056/NEJMra1810772
Memel Z, Chesney K, Pangal DJ et al (2019) Outcomes following transsphenoidal pituitary surgery in the elderly: a retrospective single-center review. Oper Neurosurg (Hagerstown) 16:302–309. https://doi.org/10.1093/ons/opy109
Tardivo V, Penner F, Garbossa D et al (2020) Surgical management of pituitary adenomas: does age matter? Pituitary 23:92–102. https://doi.org/10.1007/s11102-019-01014-1
Wilson PJ, Omay SB, Kacker A et al (2017) Endonasal endoscopic pituitary surgery in the elderly. J Neurosurg 128:429–436. https://doi.org/10.3171/2016.11.JNS162286
Dusick JR, Esposito F, Kelly DF et al (2005) The extended direct endonasal transsphenoidal approach for nonadenomatous suprasellar tumors. J Neurosurg 102:832–841. https://doi.org/10.3171/jns.2005.102.5.0832
Dusick JR, Esposito F, Mattozo CA et al (2006) Endonasal transsphenoidal surgery: the patient’s perspective-survey results from 259 patients. Surg Neurol 65:332–341. https://doi.org/10.1016/j.surneu.2005.12.010(discussion 341–342)
Fatemi N, Dusick JR, de Paiva Neto MA, Kelly DF (2008) The endonasal microscopic approach for pituitary adenomas and other parasellar tumors: a 10-year experience. Neurosurgery 63:244–256. https://doi.org/10.1227/01.NEU.0000327025.03975.BA(discussion 256)
Kelly DF (2007) Transsphenoidal surgery for Cushing’s disease: a review of success rates, remission predictors, management of failed surgery, and Nelson’s Syndrome. Neurosurg Focus 23:E5. https://doi.org/10.3171/foc.2007.23.3.7
Kelly DF, Griffiths CF, Takasumi Y et al (2015) Role of endoscopic skull base and keyhole surgery for pituitary and parasellar tumors impacting vision. J Neuroophthalmol 35:335–341. https://doi.org/10.1097/WNO.0000000000000321
McLaughlin N, Eisenberg AA, Cohan P et al (2013) Value of endoscopy for maximizing tumor removal in endonasal transsphenoidal pituitary adenoma surgery. J Neurosurg 118:613–620. https://doi.org/10.3171/2012.11.JNS112020
Karsy M, Bowers CA, Scoville J et al (2019) Evaluation of complications and costs during overlapping transsphenoidal surgery in the treatment of pituitary adenoma. Neurosurgery 84:1104–1111. https://doi.org/10.1093/neuros/nyy269
Micko ASG, Wöhrer A, Wolfsberger S, Knosp E (2015) Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg 122:803–811. https://doi.org/10.3171/2014.12.JNS141083
Fernandez-Miranda JC, Zwagerman NT, Abhinav K et al (2017) Cavernous sinus compartments from the endoscopic endonasal approach: anatomical considerations and surgical relevance to adenoma surgery. J Neurosurg. https://doi.org/10.3171/2017.2.JNS162214
Fatemi N, Dusick JR, Mattozo C et al (2008) Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63:709–718. https://doi.org/10.1227/01.NEU.0000325725.77132.90(discussion 718–719)
Kelly DF, Fatemi N, Dusick J (2010) Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 67:E221. https://doi.org/10.1227/01.neu.0000371145.97148.e5
Lees PD, Pickard JD (1987) Hyperprolactinemia, intrasellar pituitary tissue pressure, and the pituitary stalk compression syndrome. J Neurosurg 67:192–196. https://doi.org/10.3171/jns.1987.67.2.0192
Mooney MA, Sarris CE, Zhou JJ et al (2019) Proposal and Validation of a Simple Grading Scale (TRANSSPHER Grade) for predicting gross total resection of nonfunctioning pituitary macroadenomas after transsphenoidal surgery. Oper Neurosurg (Hagerstown) 17:460–469. https://doi.org/10.1093/ons/opy401
Barkhoudarian G, Cutler AR, Yost S et al (2015) Impact of selective pituitary gland incision or resection on hormonal function after adenoma or cyst resection. Pituitary 18:868–875. https://doi.org/10.1007/s11102-015-0664-3
Griffiths CF, Cutler AR, Duong HT et al (2014) Avoidance of postoperative epistaxis and anosmia in endonasal endoscopic skull base surgery: a technical note. Acta Neurochir (Wien) 156:1393–1401. https://doi.org/10.1007/s00701-014-2107-8
Conger A, Zhao F, Wang X et al (2018) Evolution of the graded repair of CSF leaks and skull base defects in endonasal endoscopic tumor surgery: trends in repair failure and meningitis rates in 509 patients. J Neurosurg 130:861–875. https://doi.org/10.3171/2017.11.JNS172141
Ishii K, Makita T, Yamashita H et al (2016) Total intravenous anesthesia with propofol is associated with a lower rate of postoperative delirium in comparison with sevoflurane anesthesia in elderly patients. J Clin Anesth 33:428–431. https://doi.org/10.1016/j.jclinane.2016.04.043
Miller D, Lewis SR, Pritchard MW et al (2018) Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012317.pub2
Kolia NR, Man L-X (2019) Total intravenous anaesthesia versus inhaled anaesthesia for endoscopic sinus surgery: a meta-analysis of randomized controlled trials. Rhinology 57:402–410. https://doi.org/10.4193/Rhin19.171
Griffiths CF, Barkhoudarian G, Cutler A et al (2019) Analysis of olfaction after bilateral nasoseptal rescue flap transsphenoidal approach with olfactory mucosal preservation. Otolaryngol Head Neck Surg 161:881–889. https://doi.org/10.1177/0194599819861340
Dusick JR, Esposito F, Malkasian D, Kelly DF (2007) Avoidance of carotid artery injuries in transsphenoidal surgery with the Doppler probe and micro-hook blades. Neurosurgery 60:322–328. https://doi.org/10.1227/01.NEU.0000255408.84269.A8(discussion 328–329)
Barkhoudarian G, Palejwala SK, Ansari S et al (2019) Rathke’s cleft cysts: a 6-year experience of surgery vs. observation with comparative volumetric analysis. Pituitary 22:362–371. https://doi.org/10.1007/s11102-019-00962-y
Arita K, Tominaga A, Sugiyama K et al (2006) Natural course of incidentally found nonfunctioning pituitary adenoma, with special reference to pituitary apoplexy during follow-up examination. J Neurosurg 104:884–891. https://doi.org/10.3171/jns.2006.104.6.884
Daly AF, Rixhon M, Adam C et al (2006) High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium. J Clin Endocrinol Metab 91:4769–4775. https://doi.org/10.1210/jc.2006-1668
Thomas JG, Gadgil N, Samson SL et al (2014) Prospective trial of a short hospital stay protocol after endoscopic endonasal pituitary adenoma surgery. World Neurosurg 81:576–583. https://doi.org/10.1016/j.wneu.2013.11.014
Tuleasca C, Ducos Y, Leroy H-A et al (2020) Transsphenoidal resection for pituitary adenoma in elderly versus younger patients: a systematic review and meta-analysis. Acta Neurochir 162:1297–1308. https://doi.org/10.1007/s00701-020-04300-1
Ziu M, Dunn IF, Hess C et al (2016) Congress of neurological surgeons systematic review and evidence-based guideline on posttreatment follow-up evaluation of patients with nonfunctioning pituitary adenomas. Neurosurgery 79:E541–543. https://doi.org/10.1227/NEU.0000000000001392
Kelly DF, Laws ER, Fossett D (1995) Delayed hyponatremia after transsphenoidal surgery for pituitary adenoma. Report of nine cases. J Neurosurg 83:363–367. https://doi.org/10.3171/jns.1995.83.2.0363
Burke WT, Cote DJ, Iuliano SI et al (2018) A practical method for prevention of readmission for symptomatic hyponatremia following transsphenoidal surgery. Pituitary 21:25–31. https://doi.org/10.1007/s11102-017-0843-5
Little AS, Chicoine MR, Kelly DF et al (2020) Evaluation of surgical resection goal and its relationship to extent of resection and patient outcomes in a multicenter prospective study of patients with surgically treated, nonfunctioning pituitary adenomas: a case series. Oper Neurosurg (Hagerstown) 18:26–33. https://doi.org/10.1093/ons/opz085
Paluzzi A, Fernandez-Miranda JC, Tonya Stefko S et al (2014) Endoscopic endonasal approach for pituitary adenomas: a series of 555 patients. Pituitary 17:307–319. https://doi.org/10.1007/s11102-013-0502-4
Little AS, Gardner PA, Fernandez-Miranda JC et al (2019) Pituitary gland recovery following fully endoscopic transsphenoidal surgery for nonfunctioning pituitary adenoma: results of a prospective multicenter study. J Neurosurg. https://doi.org/10.3171/2019.8.JNS191012
Stefanska A, Cembrowska P, Kubacka J et al (2019) Gonadotropins and their association with the risk of prediabetes and type 2 diabetes in middle-aged postmenopausal women. Dis Mark 2019:2384069. https://doi.org/10.1155/2019/2384069
Acknowledgements
The authors would like to acknowledge the support of Pacific Neuroscience Institute Foundation and Saint John’s Health Center Foundation for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Kelly receives royalties from Mizuho, Inc. Dr. Barkhoudarian is a consultant for Vascular Technologies Inc. No other authors have financial conflicts of interest to disclose. Dr Araque is a member of the advisory board for Cushing’s Disease at Corcept.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thakur, J.D., Corlin, A., Mallari, R.J. et al. Pituitary adenomas in older adults (≥ 65 years): 90-day outcomes and readmissions: a 10-year endoscopic endonasal surgical experience. Pituitary 24, 14–26 (2021). https://doi.org/10.1007/s11102-020-01081-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-020-01081-9