Abstract
Purpose
Resource utilization and costs in Cushing’s disease (CD) patients have not been studied extensively. We compared CD patients with diabetes mellitus (DM) patients and population-based controls to characterize differences in utilization and costs.
Methods
Using 2008–2012 MarketScan® database, we identified three patient groups: (1) CD patients; (2) DM patients; and (3) population-based control patients without CD. DM and control patients were matched to CD patients by age, gender, region, and review year in a 2:1 ratio. Outcomes included annual healthcare resource utilization and costs.
Results
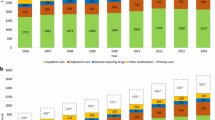
There were 1852 CD patients, 3704 DM patients and 3704 controls. Mean age was 42.9 years; 78.2 % were female. CD patients were hospitalized more frequently (19.3 %) than DM patients (11.0 %, p < .001) or controls (5.6 %, p < .001). CD patients visited the ED more frequently (25.4 %) than DM patients (21.1 %, p < .001) or controls (14.3 %, p < .001). CD patients had more office visits than DM patients (19.1 vs. 10.7, p < .001) or controls (7.1, p < .001). CD patients on average filled more prescriptions than DM patients (51.7 vs. 42.7, p < .001) or controls (20.5, p < .001). Mean total healthcare costs for CD patients were $26,269 versus $12,282 for DM patients (p < .001) and $5869 for controls (p < .001).
Conclusions
CD patients had significantly higher annual rates of healthcare resource utilization compared to matched DM patients and population controls without CD. CD patient costs were double DM costs and quadruple control costs. This study puts into context the additional burdens of CD over DM, a common, chronic endocrine condition affecting multiple organ systems, and population controls.
Similar content being viewed by others
References
Colao A, Boscaro M, Ferone D, Casanueva FF (2014) Managing Cushing’s disease: the state of the art. Endocrine 47(1):9–20
Broder MS, Neary MP, Chang E, Cherepanov D, Ludlam WH (2014) Incidence of Cushing’s syndrome and Cushing’s disease in commercially-insured patients <65 years old in the United States. Pituitary [Epub ahead of print]
Newell-Price J, Bertagna X, Grossman AB, Nieman LK (2006) Cushing’s syndrome. Lancet 367:1605–1617
Dekkers OM, Biermasz NR, Pereira AM, Roelfsema F, van Aken MO, Voormolen JH, Romijn JA (2007) Mortality in patients treated for Cushing’s disease is increased, compared with patients treated for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab 92:976–981
Broder MS, Neary MP, Chang E, Ludlam WH, Cherepanov D (2013) Annual economic burden associated with Cushing’s disease in the United States. Presented at: ENDO 2013, 17 June 2013, San Francisco, CA
Swearingen B, Wu N, Chen SY, Pulgar S, Biller BM (2011) Health care resource use and costs among patients with Cushing disease. Endocr Pract 17:681–690
Burton T, Le Nestour E, Neary M, Ludlam WH (2014) Economic burden of Cushing’s disease in a large US managed care health care plan. Presented at: ENDO 2014, 21–24 June 2014, Chicago, IL
Patil CG, Lad SP, Harsh GR, Laws ER Jr, Boakye M (2007) National trends, complications, and outcomes following transsphenoidal surgery for Cushing’s disease from 1993 to 2002. Neurosurg Focus 23(3):E7
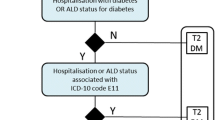
Burton TM, Rey GG, Neary MP, Ludlam WH, Le Nestour E (2013) Development of an algorithm to identify Cushing disease patients in a US administrative claims database. Presented at: 13th International Pituitary Congress, 12–14 June 2013, San Francisco, CA
Bureau of Labor Statistics. Consumer Price Index: Measuring Price Change for Medical Care in the CPI. http://www.bls.gov/cpi/cpifact4.htm. Last updated 12 April 2010. Last Accessed 29 April 2014
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Hwang W, Weller W, Ireys H, Anderson G (2001) Out-of-pocket medical spending for care of chronic conditions. Health Aff 20:267–278
American Diabetes Association (2013) Economic costs of diabetes in the US in 2012. Diabetes Care 36:1033–1046
Brilleman SL, Purdy S, Salisbury C, Windmeijer F, Gravelle H, Hollinghurst S (2013) Implications of comorbidity for primary care costs in the UK: a retrospective observational study. Br J Gen Pract 63:e274–e282
Meyers JL, Parasuraman S, Bell KF, Graham JP, Candrilli SD (2014) The high-cost, type 2 diabetes mellitus patient: an analysis of managed care administrative data. Arch Public Health 72:6
O’Shea M, Teeling M, Bennett K (2013) The prevalence and ingredient cost of chronic comorbidity in the Irish elderly population with medication treated type 2 diabetes: a retrospective cross-sectional study using a national pharmacy claims database. BMC Health Serv Res 13:23
American Diabetes Association (2014) Standards of medical care in diabetes–2014. Diabetes Care 37(Suppl. 1):S14–S80
Buchfelder M, Schlaffer S (2010) Pituitary surgery for Cushing’s disease. Neuroendocrinology 92(Suppl 1):102–106
Loh-Trivedi M (2014) Perioperative management of the diabetic patient. Medscape from WebMD. http://emedicine.medscape.com/article/284451-overview. Last updated June 10, 2013. Accessed 16 Sept 2014
Patel DA, Maldonado M, Stephens JM, Pulgar S, Swearingen B (2011) Cost of second line non-pharmacologic interventions and their related complications in Cushing’s disease: A literature-based economic analysis. Presented at: 12th International Pituitary Congress, June 1–3, 2011, Boston, MA
Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, Hudson M, Mendoza J, Johnson R, Lin E, Umpierrez GE (2010) Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 33:1783–1788
Aron DC (2010) Cushing’s syndrome: why is diagnosis so difficult? Rev Endocr Metab Disord 11:105–116
Bertagna X, Guignat L, Groussin L, Bertherat J (2009) Cushing’s disease. Best Pract Res Clin Endocrinol Metab 23:607–623
Tritos NA, Biller BM, Swearingen B (2011) Management of Cushing disease. Nat Rev Endocrinol 7:279–289
Feelders RA, Pulgar SJ, Kempel A, Pereira AM (2012) The burden of Cushing’s disease: clinical and health-related quality of life aspects. Eur J Endocrinol 167:311–326
Acknowledgments
The authors thank Gordon H. Sun, M.D., and Dasha Cherepanov, Ph.D., for assisting with the manuscript. This study was funded by Novartis Pharmaceuticals Corporation. Financial relationships with the organization that sponsored the research are as follows: Maureen P. Neary and William H. Ludlam are employees of Novartis Pharmaceuticals Corporation; Michael S. Broder and Eunice Chang are employees of Partnership for Health Analytic Research, LLC (PHAR), a health services research company that received funding for this research from Novartis. This study was presented at AMCP Nexus, Boston, MA, October 8–9, 2014.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Broder, M.S., Neary, M.P., Chang, E. et al. Incremental healthcare resource utilization and costs in US patients with Cushing’s disease compared with diabetes mellitus and population controls. Pituitary 18, 796–802 (2015). https://doi.org/10.1007/s11102-015-0654-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-015-0654-5