Abstract
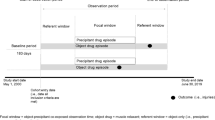
Background Concurrent opioid and benzodiazepine use (“double-threat”) and opioid, benzodiazepine, and muscle relaxant use (“triple-threat”) are linked to increased adverse events compared to opioid use alone. Objectives To assess prevalence of double-threat and triple-threat in the US and to measure association between double- and triple-threat and emergency department visits. Setting Nationally representative, 2-year health database of the United States. Method A retrospective cohort study was conducted using the national medical expenditure panel survey. Two-year prevalence of combination use was measured. Association between 2013–2014 double- and triple-threat exposure and emergency department visit compared to non-users, opioid-users, and all other exposure combinations assessed using logistic regression. Main outcome measures Survey-weighted prevalence of triple-threat and double-threat in 2013 and 2014 was measured. The outcome variable of at least one emergency department visit in a study year was utilized for the logistic regression. Results Opioids, benzodiazepines, and muscle relaxants were used in 11.9% (38.4 million lives), 4.2% (13.5 million), and 3.4% (10.9 million) individuals respectively in 2013, and 12.2% (39.3 million), 4.6% (14.8 million), and 3.6% (11.6 million), respectively in 2014. Prevalence of individuals on double-threat rose from 1.6 to 1.9% from 2013 to 2014. Triple-threat prevalence was unchanged at 0.53% in that interval. Triple-threat patients had increased emergency department visit probability with ORs of 9.19 (95% CI 9.17–9.22) in 2013, 9.82 (95% CI 9.79–9.85) in 2014, and 5.90 (95% CI 5.89–5.92) for longitudinal 2013–2014 analysis compared to non-users. Double-threat patients had increased emergency department visit probability with ORs of 4.57 (95% CI 4.56–4.58) in 2013, 6.66 (95% CI 6.65–6.68) in 2014, and 4.49 (95% CI 4.48–4.50) for 2013–2014 analysis compared to non-users. Conclusions Concurrent opioid and benzodiazepine use and opioid, benzodiazepine, and muscle relaxant use increased probability of emergency department visit. Amplified efforts in surveillance, prescribing, and default follow-up for concurrent opioid, benzodiazepine, muscle relaxant use are needed to reduce this public health concern.
Similar content being viewed by others
References
Abuse NI on D. Overdose death rates. 2019 [cited 2019 Sep 12]. Available from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
Research starters: worldwide deaths in world war II. Natl. WWII Mus. New Orleans. [cited 2019 Sep 12]. Available from: https://www.nationalww2museum.org/students-teachers/student-resources/research-starters/research-starters-worldwide-deaths-world-war.
Vietnam war US. Military fatal casualty statistics. Natl. Arch. 2016 [cited 2019 Sep 12]. Available from: https://www.archives.gov/research/military/vietnam-war/casualty-statistics.
Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(113–130):e22.
Schmitz A. Benzodiazepine use, misuse, and abuse: a review. Ment Health Clin. 2016;6:120–6.
Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. 2016;106:686–8.
Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017;356:j760.
CDC guideline for prescribing opioids for chronic pain-United States, 2016. MMWR Recomm Rep. 2016 [cited 2019 Sep 16];65. Available from: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm..
van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM, Cochrane Back Review Group. Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the cochrane collaboration. Spine. 2003;28:1978–92.
Concerns with concurrent therapy | Express scripts. [cited 2019 Apr 17]. Available from: https://lab.express-scripts.com/lab/insights/workers-compensation/concerns-with-concurrent-therapy.
Horsfall JT, Sprague JE. The pharmacology and toxicology of the ‘holy trinity’. Basic Clin Pharmacol Toxicol. 2017;120:115–9.
Relationship between concomitant benzodiazepine-opioid use and adverse outcomes among US veterans.. [cited 2019 Sep 16]. Available from: https://reference.medscape.com/medline/abstract/29189516.
Day C. Benzodiazepines in combination with opioid pain relievers or alcohol: Greater risk of more serious ED visit outcomes. CBHSQ Rep. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2013 [cited 2019 Sep 16]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384672/.
State of Missouri Department of Social Services. Authorization Form for Anti-Anxiety Benzodiazepine usage. https://dss.mo.gov/mhd/cs/pharmacy/pdf/AntianxietyBenzodiazepines.pdf.
Medical expenditure panel survey home. [cited 2018 Oct 3]. Available from: https://meps.ahrq.gov/mepsweb/index.jsp.
Medical expenditure panel survey background. [cited 2019 Sep 22]. Available from: https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.
Research C for DE and. New safety measures announced for opioid analgesics, prescription opioid cough products, and benzodiazepines. FDA. 2019 [cited 2019 Sep 20]; Available from: https://www.fda.gov/drugs/information-drug-class/new-safety-measures-announced-opioid-analgesics-prescription-opioid-cough-products-and.
McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13:988–96.
Controlled substance utilization review and evaluation system. State Calif.-Dep. Justice-Off. Atty. Gen. 2016 [cited 2019 Sep 18]. Available from: https://oag.ca.gov/cures.
Munzing T. Physician guide to appropriate opioid prescribing for noncancer pain. Perm J. 2017 [cited 2019 Sep 18];21. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424587/.
2017pdmpannualreport.pdf. [cited 2019 Sep 19]. Available from: https://www.floridahealth.gov/statistics-and-data/e-forcse/funding/2017pdmpannualreport.pdf.
Illinois-opioid-action-plan-Sept-6-2017-FINAL.pdf. [cited 2019 Sep 19]. Available from: https://dph.illinois.gov/sites/default/files/publications/Illinois-Opioid-Action-Plan-Sept-6-2017-FINAL.pdf.
Model-prescription-monitoring-program-PMP-Act.pdf. [cited 2019 Sep 18]. Available from: https://namsdl.org/wp-content/uploads/Model-Prescription-Monitoring-Program-PMP-Act.pdf.
United States Department of Health and Human Services. Center for Medicaid and CHIP Services Informational Bulletin. Best Practices for Addressing Opioid Overdoses, Misuse, and Addiction. https://www.medicaid.gov/sites/default/files/Federal-Policy-Guidance/Downloads/cib-02-02-16.pdf.
Theriault BM, Burger CF, Schlesinger JJ. EMR implementation of default opioid prescription quantities. J Gen Intern Med. 2018;33:1827.
Malte CA, Berger D, Saxon AJ, Hagedorn HJ, Achtmeyer CE, Mariano AJ, et al. Electronic medical record alert associated with reduced opioid and benzodiazepine coprescribing in high-risk veteran patients. 2018 [cited 2019 Sep 19]. Available from: https://www.ingentaconnect.com/content/wk/mcar/2018/00000056/00000002/art00010.
2019 Medicare advantage and part D rate announcement and call letter | CMS. [cited 2019 Sep 20]. Available from: https://www.cms.gov/newsroom/fact-sheets/2019-medicare-advantage-and-part-d-rate-announcement-and-call-letter.
Cohen SB, Cohen JW. The capacity of the medical expenditure panel survey to inform the affordable care act. Inq J Health Care Organ Provis Financing. 2013;50:124–34.
Acknowledgements
Dr. Watanabe receives support from the Health Resources and Services Administration (HRSA) of the US. Department of Health and Human Services (HHS) under Grant U1WQHP28726, “Geriatrics Workforce Enhancement Program.” Dr. Watanabe receives research support from the State of California Tobacco-Related Disease Research Program Award No. 588100 and from the National Academy of Medicine Anniversary Pharmacy Fellowship Program. He also receives support from the National Academy of Medicine Emerging Leaders in Health and Medicine Scholars program. This information, content, and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the US. government, the state of California, or the National Academies of Sciences, Engineering, and Medicine.
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watanabe, J.H., Yang, J. Association of combination opioid, benzodiazepine, and muscle relaxant usage with emergency department visits in a nationwide cohort in the United States. Int J Clin Pharm 43, 358–364 (2021). https://doi.org/10.1007/s11096-020-01012-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01012-5