Abstract
Background
Use of muscle relaxants is rapidly increasing in the USA. Little is understood about the role of drug interactions in the known association between muscle relaxants and unintentional traumatic injury, a clinically important endpoint causing substantial morbidity, disability, and death.
Objective
We examined potential associations between concomitant drugs (i.e., precipitants) taken with muscle relaxants (affected drugs, i.e., objects) and hospital presentation for unintentional traumatic injury.
Methods
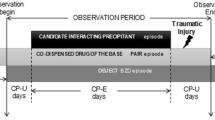
In a series of self-controlled case series studies, we screened to identify drug interaction signals for muscle relaxant + precipitant pairs and unintentional traumatic injury. We used Optum’s de-identified Clinformatics® Data Mart Database, 2000–2019. We included new users of a muscle relaxant, aged 16–90 years, who were dispensed at least one precipitant drug and experienced an unintentional traumatic injury during the observation period. We classified each observation day as precipitant exposed or precipitant unexposed. The outcome was an emergency department or inpatient discharge diagnosis for unintentional traumatic injury. We used conditional Poisson regression to estimate rate ratios adjusting for time-varying confounders and then accounted for multiple estimation via semi-Bayes shrinkage.
Results
We identified 74,657 people who initiated muscle relaxants and experienced an unintentional traumatic injury, in whom we studied concomitant use of 2543 muscle relaxant + precipitant pairs. After adjusting for time-varying confounders, 16 (0.6%) pairs were statistically significantly and positively associated with injury, and therefore deemed signals of a potential drug interaction. Among signals, semi-Bayes shrunk, confounder-adjusted rate ratios ranged from 1.29 (95% confidence interval 1.04–1.62) for baclofen + sertraline to 2.28 (95% confidence interval 1.14–4.55) for methocarbamol + lamotrigine.
Conclusions
Using real-world data, we identified several new signals of potential muscle relaxant drug interactions associated with unintentional traumatic injury. Only one among 16 signals is currently reported in a major drug interaction knowledge base. Future studies should seek to confirm or refute these signals.


Similar content being viewed by others
References
Soprano SE, Hennessy S, Bilker WB, Leonard CE. Assessment of physician prescribing of muscle relaxants in the United States, 2005–2016. JAMA Netw Open. 2020;3(6): e207664. https://doi.org/10.1001/jamanetworkopen.2020.7664.
Spence MM, Shin PJ, Lee EA, Gibbs NE. Risk of injury associated with skeletal muscle relaxant use in older adults. Ann Pharmacother. 2013;47(7–8):993–8. https://doi.org/10.1345/aph.1R735.
Billups SJ, Delate T, Hoover B. Injury in an elderly population before and after initiating a skeletal muscle relaxant. Ann Pharmacother. 2011;45(4):485–91. https://doi.org/10.1345/aph.1P628.
Norton R, Hyder AA, Bishai D, Peden M, et al. Unintentional injuries. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease control priorities in developing countries. 2nd ed. Washington, DC: World Bank; 2006.
See S. Choosing a skeletal muscle relaxant. Am Family Physician. 2008;78(3):365–70.
Zacny JP, Paice JA, Coalson DW. Characterizing the subjective and psychomotor effects of carisoprodol in healthy volunteers. Pharmacol Biochem Behav. 2011;100(1):138–43. https://doi.org/10.1016/j.pbb.2011.08.011.
Alvarez CA, Mortensen EM, Makris UE, et al. Association of skeletal muscle relaxers and antihistamines on mortality, hospitalizations, and emergency department visits in elderly patients: a nationwide retrospective cohort study. BMC Geriatr. 2015;15:2. https://doi.org/10.1186/1471-2318-15-2.
Bramness JG, Skurtveit S, Mørland J, Engeland A. The risk of traffic accidents after prescriptions of carisoprodol. Accid Anal Prev. 2007;39(5):1050–5. https://doi.org/10.1016/j.aap.2007.02.002.
Logan BK, Case GA, Gordon AM. Carisoprodol, meprobamate, and driving impairment. J Forensic Sci. 2000;45(3):619–23.
Golden AG, Ma Q, Nair V, Florez HJ, Roos BA. Risk for fractures with centrally acting muscle relaxants: an analysis of a national medicare advantage claims database. Ann Pharmacother. 2010;44(9):1369–75. https://doi.org/10.1345/aph.1P210.
Moody DE, Fu Y, Fang WB. Inhibition of in vitro metabolism of opioids by skeletal muscle relaxants. Basic Clin Pharmacol Toxicol. 2018;123(3):327–34. https://doi.org/10.1111/bcpt.12999.
LeRoy, Aida A, Morse, M Lee. Multiple medications and vehicle crashes: analysis of databases. Washington DC: U.S. Department of Transportation; 2008.
FDA drug safety communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning. Silver Spring (MD): US Food and Drug Administration; 2016.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain: United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. https://doi.org/10.15585/mmwr.rr6501e1.
Kitzman P, Cecil D, Kolpek JH. The risks of polypharmacy following spinal cord injury. J Spinal Cord Med. 2017;40(2):147–53. https://doi.org/10.1179/2045772314Y.0000000235.
Zhou M, Leonard CE, Brensinger CM, et al. Pharmacoepidemiologic screening of potential oral anticoagulant drug interactions leading to thromboembolic events. Clin Pharmacol Ther. 2020;108(2):377–86. https://doi.org/10.1002/cpt.1845.
Leonard CE, Zhou M, Brensinger CM, et al. Clopidogrel drug interactions and serious bleeding: generating real-world evidence via automated high-throughput pharmacoepidemiologic screening. Clin Pharmacol Ther. 2019;106(5):1067–75. https://doi.org/10.1002/cpt.1507.
Leonard CE, Brensinger CM, Acton EK, et al. Population-based signals of antidepressant drug interactions associated with unintentional traumatic injury. Clin Pharmacol Ther. 2021;110(2):409–23. https://doi.org/10.1002/cpt.2195.
van den Anker J, Reed MD, Allegaert K, Kearns GL. Developmental changes in pharmacokinetics and pharmacodynamics. J Clin Pharmacol. 2018;58(Suppl. 10):S10-25. https://doi.org/10.1002/jcph.1284.
Fernandez E, Perez R, Hernandez A, Tejada P, Arteta M, Ramos JT. Factors and mechanisms for pharmacokinetic differences between pediatric population and adults. Pharmaceutics. 2011;3(1):53–72. https://doi.org/10.3390/pharmaceutics3010053.
Stephenson T. How children’s responses to drugs differ from adults. Br J Clin Pharmacol. 2005;59(6):670–3. https://doi.org/10.1111/j.1365-2125.2005.02445.x.
Sears JM, Bowman SM, Rotert M, Hogg-Johnson S. A new method to classify injury severity by diagnosis: validation using workers’ compensation and trauma registry data. J Occup Rehabil. 2015;25(4):742–51. https://doi.org/10.1007/s10926-015-9582-5.
Greenland S. A semi-Bayes approach to the analysis of correlated multiple associations, with an application to an occupational cancer-mortality study. Stat Med. 1992;11(2):219–30. https://doi.org/10.1002/sim.4780110208.
Strömberg U. Empirical Bayes and semi-Bayes adjustments for a vast number of estimations. Eur J Epidemiol. 2009;24(12):737–41. https://doi.org/10.1007/s10654-009-9393-0.
National Center for Injury Prevention and Control. WISQARS: leading causes of death reports, 1981–2019, United States. https://wisqars.cdc.gov:8443/costT/ProcessPart1FinishOutServlet. Updated 2014 [Accessed 3 Dec 2021].
Li Y, Delcher C, Reisfield GM, Wei YJ, Brown JD, Winterstein AG. Utilization patterns of skeletal muscle relaxants among commercially insured adults in the United States from 2006 to 2018. Pain Med. 2021;22(10):2153–61. https://doi.org/10.1093/pm/pnab088.
Leonard CE, Brensinger CM, Pham Nguyen TP, et al. Screening to identify signals of opioid drug interactions leading to unintentional traumatic injury. Biomed Pharmacother. 2020;130: 110531. https://doi.org/10.1016/j.biopha.2020.110531.
Smith HS. Opioid metabolism. Mayo Clin Proc. 2009;84(7):613–24.
Emeny RT, Chang C, Skinner J, et al. Association of receiving multiple, concurrent fracture-associated drugs with hip fracture risk. JAMA Netw Open. 2019;2(11): e1915348. https://doi.org/10.1001/jamanetworkopen.2019.15348.
Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343: d4551. https://doi.org/10.1136/bmj.d4551.
Marcum ZA, Perera S, Thorpe JM, et al. Antidepressant use and recurrent falls in community-dwelling older adults: findings from the Health ABC Study. Ann Pharmacother. 2016;50(7):525–33. https://doi.org/10.1177/1060028016644466.
Muanda FT, Blake PG, Weir MA, et al. Association of baclofen with falls and fractures in patients with CKD. Am J Kidney Dis. 2021;78(3):470–3.
Pfizer Laboratories Div Pfizer Inc. Chantix: varenicline tartrate tablet, film coated. Updated 2019. http://www.labeling.pfizer.com. Accessed 02 Jan 2022.
Kuehn BM. Varenicline gets stronger warnings about psychiatric problems, vehicle crashes. JAMA. 2009;302(8):834. https://doi.org/10.1001/jama.2009.1153.
Gunnell D, Irvine D, Wise L, Davies C, Martin RM. Varenicline and suicidal behaviour: a cohort study based on data from the general practice research database. BMJ. 2009;339: b3805. https://doi.org/10.1136/bmj.b3805.
Molero Y, Lichtenstein P, Zetterqvist J, Gumpert CH, Fazel S. Varenicline and risk of psychiatric conditions, suicidal behaviour, criminal offending, and transport accidents and offences: population based cohort study. BMJ. 2015;350: h2388. https://doi.org/10.1136/bmj.h2388.
Dalén P, Alvan G, Wakelkamp M, Olsen H. Formation of meprobamate from carisoprodol is catalysed by CYP2C19. Pharmacogenetics. 1996;6(5):387–94. https://doi.org/10.1097/00008571-199610000-00002.
Gonzalez LA, Gatch MB, Taylor CM, Bell-Horner CL, Forster MJ, Dillon GH. Carisoprodol-mediated modulation of GABAA receptors: In vitro and in vivo studies. J Pharmacol Exp Ther. 2009;329(2):827–37. https://doi.org/10.1124/jpet.109.151142.
DuBois DW, Damborsky JC, Fincher AS, Frye GD, Winzer-Serhan UH. Varenicline and nicotine enhance GABAergic synaptic transmission in rat CA1 hippocampal and medial septum/diagonal band neurons. Life Sci. 2013;92(6–7):337–44. https://doi.org/10.1016/j.lfs.2012.12.013.
Ye JH, Ponnudurai R, Schaefer R. Ondansetron: a selective 5-HT(3) receptor antagonist and its applications in CNS-related disorders. CNS Drug Rev. 2001;7(2):199–213. https://doi.org/10.1111/j.1527-3458.2001.tb00195.x.
Patel TK, Patel PB, Tripathi CB. Effect of pantoprazole and its interactions with vecuronium on the neuromuscular junction. Indian J Pharmacol. 2010;42(1):36–9. https://doi.org/10.4103/0253-7613.62410.
Witenko C, Moorman-Li R, Motycka C, et al. Considerations for the appropriate use of skeletal muscle relaxants for the management of acute low back pain. P T. 2014;39(6):427–35.
Kaddar N, Vigneault P, Pilote S, Patoine D, Simard C, Drolet B. Tizanidine (Zanaflex): a muscle relaxant that may prolong the QT interval by blocking IKr. J Cardiovasc Pharmacol Ther. 2012;17(1):102–9. https://doi.org/10.1177/1074248410395020.
McDonald MG, Au NT, Rettie AE. P450-based drug-drug interactions of amiodarone and its metabolites: diversity of inhibitory mechanisms. Drug Metab Dispos. 2015;43(11):1661–9. https://doi.org/10.1124/dmd.115.065623.
de Vries M, Seppala LJ, Daams JG, van de Glind EMM, Masud T, van der Velde N. Fall-risk-increasing drugs: a systematic review and meta-analysis: I cardiovascular drugs. J Am Med Dir Assoc. 2018;19(4):371.e1-371.e9. https://doi.org/10.1016/j.jamda.2017.12.013.
Sill JC, Schumacher K, Southorn PA, Reuter J, Yaksh TL. Bradycardia and hypotension associated with baclofen used during general anesthesia. Anesthesiology. 1986;64(2):255–8. https://doi.org/10.1097/00000542-198602000-00022.
Ogawa S, Ishiki M, Nako K, et al. Sitagliptin, a dipeptidyl peptidase-4 inhibitor, decreases systolic blood pressure in Japanese hypertensive patients with type 2 diabetes. Tohoku J Exp Med. 2011;223(2):133–5. https://doi.org/10.1620/tjem.223.133.
Moga DC, Carnahan RM, Lund BC, et al. Risks and benefits of bladder antimuscarinics among elderly residents of veterans affairs community living centers. J Am Med Dir Assoc. 2013;14(10):749–60. https://doi.org/10.1016/j.jamda.2013.03.008.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The US National Institutes of Health supported this work (R01AG060975, R01DA048001, R01AG064589, and R01AG025152).
Conflict of interest
GKD receives funding from the American Society of Hematology and the National Institutes of Health. CEL is an Executive Committee Member of the University of Pennsylvania’s Center for Pharmacoepidemiology Research and Training. The Center receives funds from Pfizer and Sanofi to support pharmacoepidemiology education. CEL recently received honoraria from the American College of Clinical Pharmacy Foundation and the University of Florida College of Pharmacy. CEL receives travel support from John Wiley and Sons. CEL is a Special Government Employee of the US Food and Drug Administration; he consults for their Reagan-Udall Foundation. CEL’s spouse is employed by Merck; neither she nor CEL holds stock in the company. JRH is a coauthor and publisher of The Top 100 Drug Interactions: A Guide to Patient Management and a consultant to Urovant Sciences and Seegnal US. WBB serves on multiple data safety monitoring boards for Genentech. SD has research funding from GlaxoSmithKline. SH has consulted for multiple pharmaceutical companies, and directs the University of Pennsylvania’s Center for Pharmacoepidemiology Research and Training. CMB, EKA, SC, MMM, TAM, DWO, TPPN, SES, and DJW declare no competing interests for this work.
Data availability
Data are not publicly available.
Code availability
Codes are available upon request from the corresponding author.
Author contributions
GKD wrote the manuscript. CEL, SH, and WBB designed the research. GKD, SH, CMB, EKA, WBB, SC, SD, JRH, MMM, TAM, DWO, TPPN, SES, DJW, and CEL performed the research. CMB and WBB analyzed the data. CMB and WBB contributed analytic tools. All authors approve the final version of the manuscript and agree to be accountable for the work.
Ethics approval
At the University of Pennsylvania, studies using Optum are deemed exempt by the Institutional Review Board (protocol #819924).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dawwas, G.K., Hennessy, S., Brensinger, C.M. et al. Signals of Muscle Relaxant Drug Interactions Associated with Unintentional Traumatic Injury: A Population-Based Screening Study. CNS Drugs 36, 389–400 (2022). https://doi.org/10.1007/s40263-022-00909-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00909-1