Abstract
Introduction
Blood–brain barrier (BBB) remains to be the major obstacle to conquer in treating patients with malignant brain tumors. Radiation therapy (RT), despite being the mainstay adjuvant modality regardless of BBB, the effect of radiation induced cell death is hindered by the hypoxic microenvironment. Focused ultrasound (FUS) combined with systemic microbubbles has been shown not only to open BBB but also potentially increased regional perfusion. However, no clinical study has investigated the combination of RT with FUS-BBB opening (RT-FUS).
Methods
We aimed to provide preclinical evidence of RT-FUS combination in GBM animal model, and to report an interim analysis of an ongoing single arm, prospective, pilot study (NCT04988750) of combining RT-FUS for recurrent malignant high grade glioma patients, of whom re-RT was considered for disease control. In both preclinical and clinical studies, FUS-BBB opening was conducted within 2 h before RT. Treatment responses were evaluated by objective response rate (ORR) using magnetic resonance imaging, progression free survival, and overall survival, and adverse events (AE) in clinical study. Survival analysis was performed in preclinical study and descriptive analysis was performed in clinical study.
Results
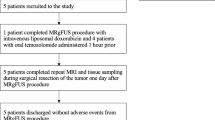
In mouse GBM model, the survival analysis showed RT-FUS (2 Gy) group was significantly longer than RT (2 Gy) group and control, but not RT (5 Gy) group. In the pilot clinical trial, an interim analysis of six recurrent malignant high grade glioma patients underwent a total of 24 RT-FUS treatments was presented. Three patients had rapid disease progression at a mean of 33 days after RT-FUS, while another three patients had at least stable disease (mean 323 days) after RT-FUS with or without salvage chemotherapy or target therapy. One patient had partial response after RT-FUS, making the ORR of 16.7%. There was no FUS-related AEs, but one (16.7%) re-RT-related grade three radiation necrosis.
Conclusion
Reirradiation is becoming an option after disease recurrence for both primary and secondary malignant brain tumors since systemic therapy significantly prolongs survival in cancer patients. The mechanism behind the synergistic effect of RT-FUS in preclinical model needs further study. The clinical evidence from the interim analysis of an ongoing clinical trial (NCT04988750) showed a combination of RT-FUS was safe (no FUS-related adverse effect). A comprehensive analysis of radiation dosimetry and FUS energy distribution is expected after completing the final recruitment.



Similar content being viewed by others
Change history
10 April 2024
A Correction to this paper has been published: https://doi.org/10.1007/s11060-024-04671-w
References
Ostrom QT et al (2022) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2015–2019. Neuro Oncol 24:v1–v95. https://doi.org/10.1093/neuonc/noac202
Tabouret E et al (2012) Recent trends in epidemiology of brain metastases: an overview. Anticancer Res 32:4655–4662
Vogelbaum MA et al (2022) Treatment for brain metastases: ASCO-SNO-ASTRO guideline. J Clin Oncol 40:492–516. https://doi.org/10.1200/JCO.21.02314
Lin X, DeAngelis LM (2015) Treatment of brain metastases. J Clin Oncol 33:3475–3484. https://doi.org/10.1200/JCO.2015.60.9503
Arvanitis CD, Ferraro GB, Jain RK (2020) The blood-brain barrier and blood-tumour barrier in brain tumours and metastases. Nat Rev Cancer 20:26–41. https://doi.org/10.1038/s41568-019-0205-x
van den Bent MJ et al (2023) Primary brain tumours in adults. Lancet. https://doi.org/10.1016/S0140-6736(23)01054-1
Walker MD, Strike TA, Sheline GE (1979) An analysis of dose-effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys 5:1725–1731. https://doi.org/10.1016/0360-3016(79)90553-4
Cabrera AR et al (2016) Radiation therapy for glioblastoma: executive summary of an american society for radiation oncology evidence-based clinical practice guideline. Pract Radiat Oncol 6:217–225. https://doi.org/10.1016/j.prro.2016.03.007
Gondi V et al (2022) Radiation therapy for brain metastases: an ASTRO clinical practice guideline. Pract Radiat Oncol 12:265–282. https://doi.org/10.1016/j.prro.2022.02.003
Minniti G, Niyazi M, Alongi F, Navarria P, Belka C (2021) Current status and recent advances in reirradiation of glioblastoma. Radiat Oncol 16:36. https://doi.org/10.1186/s13014-021-01767-9
Shi W et al (2018) Investigating the effect of reirradiation or systemic therapy in patients with glioblastoma after tumor progression: a secondary analysis of NRG oncology/radiation therapy oncology group trial 0525. Int J Radiat Oncol Biol Phys 100:38–44. https://doi.org/10.1016/j.ijrobp.2017.08.038
Tsien CI et al (2023) NRG Oncology/RTOG1205: a randomized phase II trial of concurrent bevacizumab and reirradiation versus bevacizumab alone as treatment for recurrent glioblastoma. J Clin Oncol 41:1285–1295. https://doi.org/10.1200/JCO.22.00164
Amberger-Murphy V (2009) Hypoxia helps glioma to fight therapy. Curr Cancer Drug Targets 9:381–390. https://doi.org/10.2174/156800909788166637
Kabakov AE, Yakimova AO (2021) Hypoxia-induced cancer cell responses driving radioresistance of hypoxic tumors: approaches to targeting and radiosensitizing. Cancers (Basel) 13(5):1102. https://doi.org/10.3390/cancers13051102
Emami B et al (1991) Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 21:109–122. https://doi.org/10.1016/0360-3016(91)90171-y
Lawrence YR et al (2010) Radiation dose-volume effects in the brain. Int J Radiat Oncol Biol Phys 76:S20–27. https://doi.org/10.1016/j.ijrobp.2009.02.091
Greene-Schloesser D et al (2012) Radiation-induced brain injury: a review. Front Oncol 2:73. https://doi.org/10.3389/fonc.2012.00073
Aryal M, Vykhodtseva N, Zhang YZ, Park J, McDannold N (2013) Multiple treatments with liposomal doxorubicin and ultrasound-induced disruption of blood-tumor and blood-brain barriers improve outcomes in a rat glioma model. J Control Release 169:103–111. https://doi.org/10.1016/j.jconrel.2013.04.007
Kovacs Z et al (2014) Prolonged survival upon ultrasound-enhanced doxorubicin delivery in two syngenic glioblastoma mouse models. J Control Release 187:74–82. https://doi.org/10.1016/j.jconrel.2014.05.033
Park J, Aryal M, Vykhodtseva N, Zhang YZ, McDannold N (2017) Evaluation of permeability, doxorubicin delivery, and drug retention in a rat brain tumor model after ultrasound-induced blood-tumor barrier disruption. J Control Release 250:77–85. https://doi.org/10.1016/j.jconrel.2016.10.011
Treat LH et al (2007) Targeted delivery of doxorubicin to the rat brain at therapeutic levels using MRI-guided focused ultrasound. Int J Cancer 121:901–907. https://doi.org/10.1002/ijc.22732
Treat LH, McDannold N, Zhang Y, Vykhodtseva N, Hynynen K (2012) Improved anti-tumor effect of liposomal doxorubicin after targeted blood-brain barrier disruption by MRI-guided focused ultrasound in rat glioma. Ultrasound Med Biol 38:1716–1725. https://doi.org/10.1016/j.ultrasmedbio.2012.04.015
Wei KC et al (2013) Focused ultrasound-induced blood-brain barrier opening to enhance temozolomide delivery for glioblastoma treatment: a preclinical study. PLoS ONE 8:e58995. https://doi.org/10.1371/journal.pone.0058995
Chen KT et al (2021) Neuronavigation-guided focused ultrasound for transcranial blood-brain barrier opening and immunostimulation in brain tumors. Sci Adv. https://doi.org/10.1126/sciadv.abd0772
Chen KT, Wei KC, Liu HL (2019) Theranostic strategy of focused ultrasound induced blood-brain barrier opening for CNS disease treatment. Front Pharmacol 10:86. https://doi.org/10.3389/fphar.2019.00086
Meng Y, Hynynen K, Lipsman N (2021) Applications of focused ultrasound in the brain: from thermoablation to drug delivery. Nat Rev Neurol 17:7–22. https://doi.org/10.1038/s41582-020-00418-z
Chen KT, Wei KC, Liu HL (2021) Focused ultrasound combined with microbubbles in central nervous system applications. Pharmaceutics 13(7):1084. https://doi.org/10.3390/pharmaceutics13071084
Park SH et al (2020) Safety and feasibility of multiple blood-brain barrier disruptions for the treatment of glioblastoma in patients undergoing standard adjuvant chemotherapy. J Neurosurg 134:475–483. https://doi.org/10.3171/2019.10.JNS192206
Carpentier A et al (2016) Clinical trial of blood-brain barrier disruption by pulsed ultrasound. Sci Transl Med 8:343re342. https://doi.org/10.1126/scitranslmed.aaf6086
Meng Y et al (2021) MR-guided focused ultrasound enhances delivery of trastuzumab to Her2-positive brain metastases. Sci Transl Med 13:eabj4011. https://doi.org/10.1126/scitranslmed.abj4011
Lin WH, Fan CH, Ting CY, Liu HL, Yeh CK (2013) Dynamic perfusion assessment by contrast-enhanced ultrasound in blood-brain barrier disruption. Annu Int Conf IEEE Eng Med Biol Soc 1152–1155:2013. https://doi.org/10.1109/EMBC.2013.6609710
Morishita K et al (2014) Effects of therapeutic ultrasound on intramuscular blood circulation and oxygen dynamics. J Jpn Phys Ther Assoc 17:1–7. https://doi.org/10.1298/jjpta.Vol17_001
Wen PY et al (2023) RANO 2.0: update to the response assessment in neuro-oncology criteria for high- and low-grade gliomas in adults. J Clin Oncol. https://doi.org/10.1200/JCO.23.01059
Wen PY et al (2020) Glioblastoma in adults: a society for neuro-oncology (SNO) and European Society of Neuro-Oncology (EANO) consensus review on current management and future directions. Neuro Oncol 22:1073–1113. https://doi.org/10.1093/neuonc/noaa106
Bentzen SM et al (2010) Quantitative analyses of normal tissue effects in the clinic (QUANTEC): an introduction to the scientific issues. Int J Radiat Oncol Biol Phys 76:S3–9. https://doi.org/10.1016/j.ijrobp.2009.09.040
Marks LB et al (2010) Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys 76:S10–S19. https://doi.org/10.1016/j.ijrobp.2009.07.1754
Blethen KE et al (2023) Effects of whole-brain radiation therapy on the blood-brain barrier in immunocompetent and immunocompromised mouse models. Radiat Oncol 18:22. https://doi.org/10.1186/s13014-023-02215-6
Qin DX, Zheng R, Tang J, Li JX, Hu YH (1990) Influence of radiation on the blood-brain barrier and optimum time of chemotherapy. Int J Radiat Oncol Biol Phys 19:1507–1510. https://doi.org/10.1016/0360-3016(90)90364-p
Adair JC, Baldwin N, Kornfeld M, Rosenberg GA (1999) Radiation-induced blood-brain barrier damage in astrocytoma: relation to elevated gelatinase B and urokinase. J Neurooncol 44:283–289. https://doi.org/10.1023/a:1006337912345
Fauquette W, Amourette C, Dehouck MP, Diserbo M (2012) Radiation-induced blood-brain barrier damages: an in vitro study. Brain Res 1433:114–126. https://doi.org/10.1016/j.brainres.2011.11.022
Li PJ et al (2023) Radiotherapy opens the blood-brain barrier and synergizes with anlotinib in treating glioblastoma. Radiother Oncol 183:109633. https://doi.org/10.1016/j.radonc.2023.109633
White PJ, Zhang YZ, Power C, Vykhodtseva N, McDannold N (2020) Observed effects of whole-brain radiation therapy on focused ultrasound blood-brain barrier disruption. Ultrasound Med Biol 46:1998–2006. https://doi.org/10.1016/j.ultrasmedbio.2020.04.013
Tsai PF et al (2015) Hippocampal dosimetry correlates with the change in neurocognitive function after hippocampal sparing during whole brain radiotherapy: a prospective study. Radiat Oncol 10:253. https://doi.org/10.1186/s13014-015-0562-x
Yang WC et al (2021) Hippocampal avoidance whole-brain radiotherapy without memantine in preserving neurocognitive function for brain metastases: a phase II blinded randomized trial. Neuro Oncol 23:478–486. https://doi.org/10.1093/neuonc/noaa193
Funding
This study was supported by Chang Gung Medical Research Foundation: CRRPVVK0013, and National Science and Technology Council, Taiwan: MOST 110-2314-B-182A-154-MY3.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article has been revised: The clinical trial number has been corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
11060_2023_4517_MOESM1_ESM.tif
Supplementary Figure 1. Illustration of preclinical FUS model. (A) The hind view showing the head of the mouse fixed on the stereotactic frame. A reverse pyramid design of water tank transmitted ultrasound waves was mounted on the top of the head with jelly filled between transducer contact and the scalp (arrow). (B) The front view showing the inhaled anesthetic agent coming from the tube and the water tank coming from top (arrow). (C) A schematic illustration of the time points in the preclinical study. GL261 tumor suspensions were implanted transcranially on D0. On D5, every mouse was sent to FUS-RT treatment, during which a 120-second pulsed FUS was given after systemic microbubbles injection. Radiation therapy was followed within 2 hours after sonication. Then the mouse was monitored with weekly MRIs. Supplementary file1 (TIF 1829 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, KT., Huang, CY., Pai, PC. et al. Focused ultrasound combined with radiotherapy for malignant brain tumor: a preclinical and clinical study. J Neurooncol 165, 535–545 (2023). https://doi.org/10.1007/s11060-023-04517-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04517-x