Abstract
Purpose
Fractionated stereotactic radiotherapy (FSRT) using gamma knife is useful for brain metastases. However, several uncertainties derived from fractionation pose issues for maintaining high-level accuracy. This study analyzed interfractional tumor change by performing radiological reassessment at the midterm of FSRT with ≥ 10 fractions, and the significance of replanning was evaluated.
Methods
Data of FSRT using gamma knife with ≥ 10 fractions were retrospectively collected. Interfractional volume changes in MRI at the midterm of the irradiation period were analyzed. Radiological changes after FSRT and final outcomes were also investigated.
Results
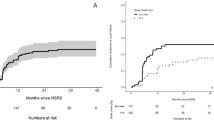
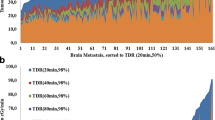
Overall, 114 lesions in 74 treatments from 66 patients were included, with previously irradiated lesions accounting for 46%. The median interval between planning and the interfractional MRI was 7 days. The interfractional change rates of tumor volume ranged from − 48 to + 72%. Significant interfractional enlargement was observed in 16 lesions (14%); evident regression was confirmed in 17 lesions (15%). Predictive factors for interfractional enlargement were small tumor and cystic lesion; high biologically effective dose was associated with regression. After FSRT, most lesions regressed within 6 months despite interfractional change type. The incidences of tumor control and radiation necrosis indicated no differences between interfractionally-regressed lesions and others.
Conclusion
This is the first study to evaluate interfractional tumor change in FSRT using gamma knife with ≥ 10 fractions, indicating significant volume changes in 29% of the lesions. These preliminary results suggest that interfractional reassessment of a treatment plan in FSRT with irradiation periods exceeding a week is necessary for more adaptive treatment.


Similar content being viewed by others
Data availability
Research data are stored in an institutional repository and will be shared upon request to the corresponding author.
References
Soffietti R, Abacioglu U, Baumert B et al (2017) Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-Oncology (EANO). Neuro Oncol 19:162–174. https://doi.org/10.1093/neuonc/now241
Yamamoto M, Serizawa T, Shuto T et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15:387–395. https://doi.org/10.1016/s1470-2045(14)70061-0
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409. https://doi.org/10.1001/jama.2016.9839
Kann BH, Park HS, Johnson SB, Chiang VL, Yu JB (2017) Radiosurgery for brain metastases: changing practice patterns and disparities in the United States. J Natl Compr Canc Netw 15:1494–1502. https://doi.org/10.6004/jnccn.2017.7003
Minniti G, Scaringi C, Paolini S et al (2016) Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (>2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys 95:1142–1148. https://doi.org/10.1016/j.ijrobp.2016.03.013
Lehrer EJ, Peterson JL, Zaorsky NG et al (2019) Single versus multifraction stereotactic radiosurgery for large brain metastases: an international meta-analysis of 24 trials. Int J Radiat Oncol Biol Phys 103:618–630. https://doi.org/10.1016/j.ijrobp.2018.10.038
Ogura K, Mizowaki T, Ogura M et al (2012) Outcomes of hypofractionated stereotactic radiotherapy for metastatic brain tumors with high risk factors. J Neurooncol 109:425–432. https://doi.org/10.1007/s11060-012-0912-6
Redmond KJ, Gui C, Benedict S et al (2021) Tumor control probability of radiosurgery and fractionated stereotactic radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 110:53–67. https://doi.org/10.1016/j.ijrobp.2020.10.034
Milano MT, Grimm J, Niemierko A et al (2021) Single- and multifraction stereotactic radiosurgery dose/volume tolerances of the brain. Int J Radiat Oncol Biol Phys 110:68–86. https://doi.org/10.1016/j.ijrobp.2020.08.013
Gondi V, Bauman G, Bradfield L et al (2022) Radiation therapy for brain metastases: an ASTRO clinical practice guideline. Pract Radiat Oncol. https://doi.org/10.1016/j.prro.2022.02.003
Lindquist C (1989) Gamma knife surgery for recurrent solitary metastasis of a cerebral hypernephroma: case report. Neurosurgery 25:802–804. https://doi.org/10.1097/00006123-198911000-00018
Higuchi Y, Serizawa T, Nagano O et al (2009) Three-staged stereotactic radiotherapy without whole brain irradiation for large metastatic brain tumors. Int J Radiat Oncol Biol Phys 74:1543–1548. https://doi.org/10.1016/j.ijrobp.2008.10.035
Serizawa T, Higuchi Y, Yamamoto M et al (2018) Comparison of treatment results between 3- and 2-stage Gamma Knife radiosurgery for large brain metastases: a retrospective multi-institutional study. J Neurosurg 131:227–237. https://doi.org/10.3171/2018.4.JNS172596
Schasfoort J, Ruschin M, Sahgal A et al (2021) Quantifying the sensitivity of target dose on intra-fraction displacement in intra-cranial stereotactic radiosurgery. Pract Radiat Oncol. https://doi.org/10.1016/j.prro.2021.11.012
Wright G, Schasfoort J, Harrold N, Hatfield P, Bownes P (2019) Intra-fraction motion gating during frameless Gamma Knife. J Radiosurg SBRT 6:67–76
Uto M, Ogura K, Katagiri T, Takehana K, Mizowaki T (2021) Interfractional target changes in brain metastases during 13-fraction stereotactic radiotherapy. Radiat Oncol 16:140. https://doi.org/10.1186/s13014-021-01869-4
Ohtakara K, Hoshi H (2014) Target volume geometric change and/or deviation from the cranium during fractionated stereotactic radiotherapy for brain metastases: potential pitfalls in image guidance based on bony anatomy alignment. J Med Imaging Radiat Oncol 58:729–736. https://doi.org/10.1111/1754-9485.12194
Kubo K, Kenjo M, Doi Y et al (2019) MRI appearance change during stereotactic radiotherapy for large brain metastases and importance of treatment plan modification during treatment period. Jpn J Radiol 37:850–859. https://doi.org/10.1007/s11604-019-00886-4
Hessen E, Nijkamp J, Damen P et al (2020) Predicting and implications of target volume changes of brain metastases during fractionated stereotactic radiosurgery. Radiother Oncol 142:175–179. https://doi.org/10.1016/j.radonc.2019.07.011
Lee MH, Kim KH, Cho KY et al (2019) Volumetric changes of intracranial metastases during the course of fractionated stereotactic radiosurgery and significance of adaptive planning. J Neurosurg. https://doi.org/10.3171/2019.3.JNS183130
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MK and AA contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MK, RN, and AA. The first draft of the manuscript was written by MK, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was conducted in accordance with the tenets of the Declaration of Helsinki. Approval was given by the relevant IRB (IRB number 21-24).
Consent to participate
Written informed consent was obtained from all patients included in this study.
Consent to publish
Informed consent was obtained from all patients whose images were included in publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kawashima, M., Akabane, A., Noda, R. et al. Interfractional change of tumor volume during fractionated stereotactic radiotherapy using gamma knife for brain metastases. J Neurooncol 159, 409–416 (2022). https://doi.org/10.1007/s11060-022-04075-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04075-8