Abstract
Objective
The optimal management of asymptomatic, skull-based meningiomas is not well defined. The aim of this study is to compare the imaging and clinical outcomes of patients with asymptomatic, skull-based meningiomas managed either with upfront stereotactic radiosurgery (SRS) or active surveillance.
Methods
This retrospective, multicenter study involved patients with asymptomatic, skull-based meningiomas. The study end-points included local tumor control and the development of new neurological deficits attributable to the tumor. Factors associated with tumor progression and neurological morbidity were also analyzed.
Results
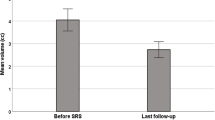
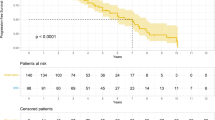
The combined unmatched cohort included 417 patients. Following propensity score matching for age, tumor volume, and follow-up 110 patients remained in each cohort. Tumor control was achieved in 98.2% and 61.8% of the SRS and active surveillance cohorts, respectively. SRS was associated with superior local tumor control (p < 0.001, HR = 0.01, 95% CI = 0.002–0.13) compared to active surveillance. Three patients (2.7%) in the SRS cohort and six (5.5%) in the active surveillance cohort exhibited neurological deterioration. One (0.9%) patient in the SRS-treated and 11 (10%) patients in the active surveillance cohort required surgical management of their meningioma during follow-up.
Conclusions
SRS is associated with superior local control of asymptomatic, skull-based meningiomas as compared to active surveillance and does so with low morbidity rates. SRS should be offered as an alternative to active surveillance as the initial management of asymptomatic skull base meningiomas. Active surveillance policies do not currently specify the optimal time to intervention when meningioma growth is noted. Our results indicate that if active surveillance is the initial management of choice, SRS should be recommended when radiologic tumor progression is noted and prior to clinical progression.

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Chamoun R, Krisht KM, Couldwell WT (2011) Incidental meningiomas. Neurosurg Focus 31:E19. https://doi.org/10.3171/2011.9.FOCUS11220
Nakamura M, Roser F, Michel J et al (2003) The natural history of incidental meningiomas. Neurosurgery 53:62–71. https://doi.org/10.1227/01.NEU.0000068730.76856.58
Hashimoto N, Rabo CS, Okita Y et al (2012) Slower growth of skull base meningiomas compared with non–skull base meningiomas based on volumetric and biological studies: clinical article. J Neurosurg 116:574–580. https://doi.org/10.3171/2011.11.JNS11999
Pikis S, Bunevicius A, Sheehan J (2021) Outcomes from treatment of asymptomatic skull base meningioma with stereotactic radiosurgery. Acta Neurochir 163:83–88. https://doi.org/10.1007/s00701-020-04648-4
Zeng L, Wang L, Ye F et al (2015) Clinical characteristics of patients with asymptomatic intracranial meningiomas and results of their surgical management. Neurosurg Rev 38:481–488. https://doi.org/10.1007/s10143-015-0619-1
Goldbrunner R, Stavrinou P, Jenkinson MD et al (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol noab. https://doi.org/10.1093/neuonc/noab150
Sughrue ME, Rutkowski MJ, Aranda D et al (2010) Treatment decision making based on the published natural history and growth rate of small meningiomas: a review and meta-analysis. J Neurosurg 113:1036–1042. https://doi.org/10.3171/2010.3.JNS091966
Oya S, Kim S-H, Sade B, Lee JH (2011) The natural history of intracranial meningiomas: clinical article. J Neurosurg 114:1250–1256. https://doi.org/10.3171/2010.12.JNS101623
Sheehan J, Pikis S, Islim A et al (2021) An international multicenter matched cohort analysis of incidental meningioma progression during active surveillance or after stereotactic radiosurgery: the IMPASSE Study. Neuro Oncol. https://doi.org/10.1093/neuonc/noab132
Huang RY, Bi WL, Weller M et al (2019) Proposed response assessment and endpoints for meningioma clinical trials: report from the response assessment in neuro-oncology working group. Neuro Oncol 21:26–36. https://doi.org/10.1093/neuonc/noy137
Barnett GH, Linskey ME, Adler JR et al (2007) Stereotactic radiosurgery–an organized neurosurgery-sanctioned definition. J Neurosurg 106:1–5. https://doi.org/10.3171/jns.2007.106.1.1
R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/
RStudio Team (2020). RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA URL http://www.rstudio.com/.
Islim AI, Mohan M, Moon RDC et al (2019) Incidental intracranial meningiomas: a systematic review and meta-analysis of prognostic factors and outcomes. J Neurooncol 142:211–221. https://doi.org/10.1007/s11060-019-03104-3
Meling TR, Da Broi M, Scheie D, Helseth E (2019) Meningiomas: skull base versus non-skull base. Neurosurg Rev 42:163–173. https://doi.org/10.1007/s10143-018-0976-7
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35. https://doi.org/10.1002/1097-0142(1950)3:1%3c32::AID-CNCR2820030106%3e3.0.CO;2-3
Rubin G, Herscovici Z, Laviv Y et al (2011) Outcome of untreated meningiomas. Isr Med Assoc J 13:157–160
Lee EJ, Kim JH, Park ES et al (2017) A novel weighted scoring system for estimating the risk of rapid growth in untreated intracranial meningiomas. J Neurosurg 127:971–980. https://doi.org/10.3171/2016.9.JNS161669
Goldbrunner R, Minniti G, Preusser M et al (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17:e383–e391. https://doi.org/10.1016/S1470-2045(16)30321-7
Bir SC, Patra DP, Maiti TK et al (2017) Direct comparison of gamma knife radiosurgery and microsurgery for small size meningiomas. World Neurosurg 101:170–179. https://doi.org/10.1016/j.wneu.2017.01.105
Gupta A, Xu Z, Cohen-Inbar O et al (2019) Treatment of asymptomatic meningioma with gamma knife radiosurgery: long-term follow-up with volumetric assessment and clinical outcome. Neurosurgery 85:E889–E899. https://doi.org/10.1093/neuros/nyz126
Kim KH, Kang SJ, Choi J-W et al (2018) Clinical and radiological outcomes of proactive gamma knife surgery for asymptomatic meningiomas compared with the natural course without intervention. J Neurosurg 130:1740–1749. https://doi.org/10.3171/2017.12.JNS171943
Bindal R, Goodman JM, Kawasaki A et al (2003) The natural history of untreated skull base meningiomas. Surg Neurol 59:87–92. https://doi.org/10.1016/S0090-3019(02)00995-3
Goldbrunner R, Stavrinou P, Jenkinson MD et al (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol. https://doi.org/10.1093/neuonc/noab150
Nakamura M, Struck M, Roser F et al (2008) Olfactory groove meningiomas: clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery 62:844–852. https://doi.org/10.1227/01.NEU.0000333788.83349.1E
Nakamura M, Roser F, Dormiani M et al (2005) Facial and cochlear nerve function after surgery of cerebellopontine angle meningiomas. Neurosurgery 57:77–90. https://doi.org/10.1227/01.neu.0000154699.29796.34
Bambakidis NC, Kakarla UK, Kim LJ et al (2008) Evolution of surgical approaches int the treatment of petroclival meningionas: a retrospective review. Neurosurgery. https://doi.org/10.1227/01.NEU.0000333784.04435.65
Chen C-M, Huang AP-H, Kuo L-T, Tu Y-K (2011) Contemporary surgical outcome for skull base meningiomas. Neurosurg Rev 34:281–296. https://doi.org/10.1007/s10143-011-0321-x
Sheehan JP, Lee C-C, Xu Z et al (2015) Edema following Gamma Knife radiosurgery for parasagittal and parafalcine meningiomas. J Neurosurg 123:1287–1293. https://doi.org/10.3171/2014.12.JNS142159
Daou BJ, Palmateer G, Wilkinson DA et al (2021) Radiation-induced imaging changes and cerebral edema following stereotactic radiosurgery for brain AVMs. AJNR Am J Neuroradiol 42:82–87. https://doi.org/10.3174/ajnr.A6880
O’Connor KP, Algan O, Vesely SK et al (2019) Factors associated with treatment failure and radiosurgery-related edema in WHO ragde 1 and 2 meningioma patients receiving gamma knife radiosurgery. World Neurosurg 130:e558–e565. https://doi.org/10.1016/j.wneu.2019.06.152
Ganz JC, Reda WA, Abdelkarim K (2009) Adverse radiation effects after gamma knife surgery in relation to dose and volume. Acta Neurochir (Wien) 151:9–19. https://doi.org/10.1007/s00701-008-0174-4
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jason Sheehan; Methodology: Jason Sheehan; Formal analysis and investigation: Georgios Mantziaris, Stylianos Pikis, Jason Sheehan; Writing—original draft preparation: Georgios Mantziaris; Writing—review and editing: All authors; Supervision: Jason Sheehan.
Corresponding author
Ethics declarations
Conflict of interest
L. Dade Lunsford is a shareholder in Elekta AB, the manufacturer of some radiosurgical devices. Roman Liscak is a consultant for Elekta AB. All remaining authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
The participating centers obtained approval by the local institutional review boards for the study and for sharing de-identified data with the coordinating office.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mantziaris, G., Pikis, S., Samanci, Y. et al. Stereotactic radiosurgery versus active surveillance for asymptomatic, skull-based meningiomas: an international, multicenter matched cohort study. J Neurooncol 156, 509–518 (2022). https://doi.org/10.1007/s11060-021-03923-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03923-3