Abstract
Purpose
The aim of this study was to determine whether a higher biological effective dose (BED) would result in improved local control in patients treated with fractionated stereotactic radiotherapy (FSRT) for their resected brain metastases.
Methods
Patients with newly diagnosed brain metastases without previous brain radiotherapy were retrospectively reviewed. Patients underwent surgical resection of at least one brain metastasis and were treated with adjuvant FSRT, delivering 25–36 Gy in 5–6 fractions. Outcomes were computed using Kaplan–Meier survival analysis and univariate analysis.
Results
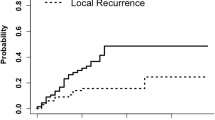
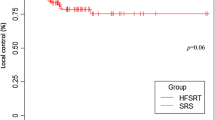
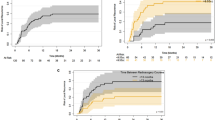
Fifty-four patients with 63 post-operative cavities were included. Median follow-up was 16 months (3–60). Median metastasis size at diagnosis was 2.9 cm (0.6–8.1) and median planning target volume was 19.7 cm3 (6.3–68.1). Two-year local control (LC) was 83%. When stratified by dose, 2 years LC rate was 95.1% in those treated with 30–36 Gy in 5–6 fractions (BED10 of 48–57.6 Gy10) versus 59.1% lesions treated with 25 Gy in 5 fractions (BED10 of 37.5 Gy10) (p < 0.001). LC was not associated with resection cavity size. One year overall survival was 68.7%, and was independent of BED10. Symptomatic radiation necrosis occurred in 7.9% of patients and was not associated with dose.
Conclusion
In the post-operative setting, high-dose FSRT (BED10 > 37.5 Gy10) were associated with a significantly higher rate of LC compared to lower BED regimens. Overall, 25 Gy in 5 fractions is not an adequate dose to control microscopic disease. If selecting a 5-fraction regimen, 30 Gy in five fractions appears to provide excellent tumor bed control.

Similar content being viewed by others
References
Andrews DW, Scott CB, Sperduto PW et al (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. https://doi.org/10.1016/S0140-6736(04)16250-8
Sittenfeld SMC, Suh JH, Murphy ES, Yu JS, Chao ST (2018) Contemporary management of 1–4 brain metastases. Front Oncol 8:385. https://doi.org/10.3389/fonc.2018.00385
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1040–1048. https://doi.org/10.1016/S1470-2045(17)30414-X
Soon YY, Tham IW, Lim KH, Koh WY, Lu JJ (2014) Surgery or radiosurgery plus whole brain radiotherapy versus surgery or radiosurgery alone for brain metastases. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009454.pub2
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. https://doi.org/10.1016/S1470-2045(09)70263-3
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409. https://doi.org/10.1001/jama.2016.9839
Brown PD, Ballman KV, Cerhan JH et al (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC.3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1049–1060. https://doi.org/10.1016/S1470-2045(17)30441-2
Combs SE, Bilger A, Diehl C et al (2018) Multicenter analysis of stereotactic radiotherapy of the resection cavity in patients with brain metastases. Cancer Med 7:2319–2327. https://doi.org/10.1002/cam4.1477
Eaton BR, LaRiviere MJ, Kim S et al (2015) Hypofractionated radiosurgery has a better safety profile than single fraction radiosurgery for large resected brain metastases. J Neurooncol 123:103–111. https://doi.org/10.1007/s11060-015-1767-4
Minniti G, Scaringi C, Paolini S et al (2016) Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (> 2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys 95:1142–1148. https://doi.org/10.1016/j.ijrobp.2016.03.013
Minniti G, Esposito V, Clarke E et al (2013) Multidose stereotactic radiosurgery (9 Gy × 3) of the postoperative resection cavity for treatment of large brain metastases. Int J Radiat Oncol Biol Phys 86:623–629. https://doi.org/10.1016/j.ijrobp.2013.03.037
Kumar AMS, Miller J, Hoffer SA et al (2018) Postoperative hypofractionated stereotactic brain radiation (HSRT) for resected brain metastases: improved local control with higher BED10. J Neurooncol 139:449–454. https://doi.org/10.1007/s11060-018-2885-6
Abuodeh Y, Ahmed KA, Naghavi AO et al (2016) Postoperative stereotactic radiosurgery using 5-Gy x 5 sessions in the management of brain metastases. World Neurosurg 90:58–65. https://doi.org/10.1016/j.wneu.2016.02.007
Lockney NA, Wang DG, Gutin PH et al (2017) Clinical outcomes of patients with limited brain metastases treated with hypofractionated (5x6Gy) conformal radiotherapy. Radiother Oncol 123:203–208. https://doi.org/10.1016/j.radonc.2017.03.018
Rajakesari S, Arvold ND, Jimenez RB et al (2014) Local control after fractionated stereotactic radiation therapy for brain metastases. J Neurooncol 120:339–346. https://doi.org/10.1007/s11060-014-1556-5
Soliman H, Ruschin M, Angelov L, et al (2018) Consensus contouring guidelines for postoperative completely resected cavity stereotactic radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 100:436–442. https://doi.org/10.1016/j.ijrobp.2017.09.047
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Musunuru, H.B., Witt, J.S., Yadav, P. et al. Impact of adjuvant fractionated stereotactic radiotherapy dose on local control of brain metastases. J Neurooncol 145, 385–390 (2019). https://doi.org/10.1007/s11060-019-03308-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03308-7