Abstract
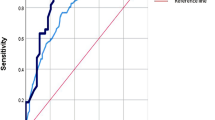
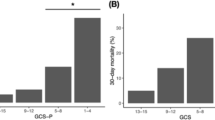
Posttraumatic hydrocephalus (PTH) is a disorder of disturbed cerebrospinal fluid (CSF) dynamics after traumatic brain injury (TBI). It can lead to brain metabolic impairment and dysfunction and has a high risk of clinical deterioration and worse outcomes. The incidence and risk factors for the development of PTH after decompressive craniectomy (DC) has been assessed in previous studies, but rare studies identify patients with higher risk for PTH among all TBI patients. This study aimed to develop and validate a risk scoring system to predict PTH after TBI. Demographics, injury severity, duration of coma, radiologic findings, and DC were evaluated to determine the independent predictors of PTH during hospitalization until 6 months following TBI through logistic regression analysis. A risk stratification system was created by assigning a number of points for each predictor and validated in an independent cohort. The model accuracy was assessed by the area under the receiver operating characteristic curve (AUC). Of 526 patients in the derivation cohort, 57 (10.84%) developed PTH during 6 months follow up. Age > 50 yrs (Odd ratio [OR] = 1.91, 95% confidence interval [CI] 1.09–3.75, 4 points), duration of coma ≥1 w (OR = 5.68, 95% CI 2.57–13.47, 9 points), Fisher grade III (OR = 2.19, 95% CI 1.24–4.36, 5 points) or IV (OR = 3.87, 95% CI 1.93–8.43, 7 points), bilateral DC (OR = 6.13, 95% CI 2.82–18.14, 9 points), and extra herniation after DC (OR = 2.36, 95% CI 1.46–4.92, 5 points) were independently associated with PTH. Rates of PTH for the low- (0–12 points), intermediate- (13–22 points) and high-risk (23–34 points) groups were 1.16%, 35.19% and 78.57% (p < 0.0001). The corresponding rates in the validation cohort, where 17/175 (9.71%) developed PTH, were 1.35%, 37.50% and 81.82% (p < 0.0001). The risk score model exhibited good-excellent discrimination in both cohorts, with AUC of 0.839 versus 0.894 (derivation versus validation) and good calibration (Hosmer-Lemshow p = 0.56 versus 0.68). This model will be useful to identify patients at high risk for PTH who may be candidates for preventive interventions, and to improve their outcomes.


Similar content being viewed by others
References
Beauchamp KM, Kashuk J, Moore EE, Bolles G, Rabb C, Seinfeld J (2010) Cranioplasty after postinjury decompressive craniectomy: is timing of the essence? J Trauma 69:270–274
Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS, Carney NA, Ghajar J (2007) Guidelines for the management of severe traumatic brain injury. Introduction. J Neurotrauma 24:S1–S2
Chen H, Guo Y, Chen SW, Wang G, Cao HL, Chen J (2012) Progressive epidural hematoma in patients with head trauma: incidence, outcome, and risk factors. Emerg Med Int 2012:134905
Choi I, Park HK, Chang JC, Cho SJ, Choi SK, Byun BJ (2008) Clinical factors for the development of posttraumatic hydrocephalus after decompressive craniectomy. J Korean Neurosurg Soc 43:227–231
Czosnyka M, Copeman J, Czosnyka Z, McConnell R, Dickinson C, Pickard JD (2000) Post-trauma-tic hydrocephalus: influence of craniectomy on the CSF circulation. J Neurol Neurosci 68:246–248
Czosnyka M, Czosnyka ZH, Whitfield PC, Donovan T, Pickard JD (2001) Age dependence of cerebrospinal pressure-volume compensation in patients with hydrocephalus. J Neurosurg 94:482–486
De Bonis P, Pompucci A, Mangiola A, Rigante L, Anile C (2010) Post-traumatic hydrocephalus after decompressive craniectomy: an underestimated risk factor. J Neurotrauma 27:1965–1970
De Bonis P, Sturiale CL, Anile C, Gaudino S, Mangiola A, Martucci M (2013) Decompressive craniectomy, interhemispheric hygroma and hydrocephalus: a timeline of events? Clin Neurol Neurosurg 115:1308–1312
Denes Z, Barsi P, Szel I, Boros E, Fazekas G (2011) Complication during postacute rehabilitation: patients with posttraumatic hydrocephalus. Int J Rehabil Res 34:222–226
Ding J, Guo Y, Tian H (2014) The influence of decompressive craniectomy on the development of hydrocephalus: a review. Arq Neuropsiquiatr 72:715–720
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6:1–9
Fotakopoulos G, Tsianaka E, Siasios G, Vagkopoulos K, Fountas K (2016) Posttraumatic hydroceph-alus after decompressive craniectomy in 126 patients with severe traumatic brain injury. J Neurol Surg A Cent Eur Neurosurg 77:88–92
Gudeman SK, Kishore PR, Becker DP, Lipper MH, Girevendulis AK, Jeffries BF, Butterworth JF 4th (1981) Computed tomography in the evaluation of incidence and significance of post-traumatic hydrocephalus. Radiology 141:397–402
Guyot LL, Michael DB (2000) Post-traumatic hydrocephalus. Neurol Res 22:25–28
Honeybul S (2010) Complications of decomepressive craniectomy for head injury. J Clin Neurosci 7:430–435
Honeybul S, Ho KM (2012) Incidence and risk factors for post-traumatic hydrocephalus following decompressive craniectomy for intractable intracranial hypertension and evacuation of mass lesions. J Neurotrauma 29:1872–1878
Jiao QF, Liu Z, Li S, Zhou LX, Li SZ, Tian W, You C (2007) Influencing factors for posttraumatic hydrocephalus in patients suffering from severe traumatic brain injuries. Chin J Traumatol 10:159–162
Kaen A, Jimenez-Roldan L, Alday R, Gomez PA, Lagares A, Alén JF, Lobato RD (2010) Interhemi-spheric hygroma after decompressive craniectomy: does it predict posttraumatic hydrocephalus? J Neurosurg 113:1287–1293
Kammersgaard LP, Linnemann M, Tibæk M (2013) Hydrocephalus following severe traumatic brain injury in adults. Incidence, timing, and clinical predictors during rehabilitation. NeuroRehabilitation 33:473–480
Ki HJ, Lee HJ, Lee HJ, Yi JS, Yang JH, Lee IW (2015) The risk factors for hydrocephalus and subdural hygroma after decompressive crainectomy in head injured patients. J Korean Neurosurg Soc 58:254–261
Kondziella D, Sonnewald U, Tullberg M, Wikkelso C (2008) Brain metabolism in adult chronic hydrocephalus. J Neurochem 106:1515–1524
Licata C, Cristofori L, Gambin R, Vivenza C, Turazzi S (2001) Post-traumatic hydrocephalus. J Neurosurg Sci 45:141–149
Mazzini L, Campini R, Angelino E, Rognone F, Pastore I, Oliveri G (2003) Posttraumatic hydrocephalus: a clinical, neuroradiologic, and neuropsychologic assessment of long-term outcome. Arch Phys Med Rehabil 84:1637–1641
Mohd Nor MA, Abdul Rahman NA, Adnan JS (2013) Post-traumatic hydrocephalus. Malays J Med Sci 20:95–96
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57:S4–S16
Shi SS, Zhang GL, Zeng T, Lin YF (2011) Posttraumatic hydrocephalus associated with decompressive cranial defect in severe brain-injured patients. Chin J Traumatol 14:343–347
Symss NP, Oi S (2013) Theories of cerebrospinal fluid dynamics and hydrocephalus: historical trend. J Neurosurg Pediatr 11:170–177
Teasdale GM, Pettigrew LE, Wilson JT, Murray G, Jennett B (1998) Analyzing outcome of treatment of severe head injury: a review and update on advancing the use of the Glasgow outcome scale. J Neurotrauma 15:587–597
Tian HL, Xu T, Hu J, Cui YH, Chen H, Zhou LF (2008a) Risk factors related to hydrocephalus after traumatic subarachnoid hemorrhage. Surg Neurol 69:241–246
Tian HL, Geng Z, Cui YH, Hu J, Xu T, Cao HL (2008b) Risk factors for posttraumatic cerebral infarction in patients with moderate or severe head trauma. Neurosurg Rev 31:431–437
Yoshioka H, Inagawa T, Tokuda Y, Inokuchi F (2000) Chronic hydrocephalus in elderly patients following subarachnoid hemorrhage. Surg Neurol 53:119–125
Yuan F, Ding J, Chen H, Guo Y, Wang G, Gao WW (2012) Predicting progressive hemorrhagic injury after traumatic brain injury: derivation and validation of a risk score based on admission characteristics. J Neurotrauma 29:2137–2142
Acknowledgements
This study was supported by the National Natural Science Foundation of China (grant 81471245 and 81501657).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Rights and permissions
About this article
Cite this article
Chen, H., Yuan, F., Chen, SW. et al. Predicting posttraumatic hydrocephalus: derivation and validation of a risk scoring system based on clinical characteristics. Metab Brain Dis 32, 1427–1435 (2017). https://doi.org/10.1007/s11011-017-0008-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-017-0008-2