Abstract
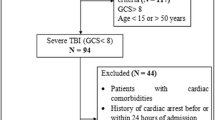
We examined the incidence and timing of posttraumatic cerebral infarction (PTCI) and provide predictive factors for the development of PTCI in patients with moderate or severe traumatic brain injury. Three hundred and fifty-three consecutive patients with moderate or severe head trauma were retrospectively reviewed to determine the incidence and timing of PTCI and to evaluate the effects of age, gender, admission Glasgow Coma Scores (GCS), decompressive craniectomy, brain herniation, and low systolic blood pressure (BP) on the development of cerebral infarction. Risk factors for posttraumatic cerebral infarction were evaluated using logistic regression analysis. PTCI was observed in 36 (11.96%) of the 353 patients, and in a majority of cases, cerebral infarction developed within 2 weeks after injury. Poor admission GCS (P < 0.01), low systolic BP (P < 0.01), brain herniation (P < 0.05), and decompression craniotomy (P < 0.05) were significantly associated with the development of PTCI. No relationship was found between PTCI and gender or increased age. Posttraumatic cerebral infarction is a relatively common complication in patients with head trauma that develops early in the clinical course. Low GCS, low systolic BP, brain herniation, and decompression craniotomy may be risk factors for PTCI in patients with moderate or severe traumatic brain injury.

Similar content being viewed by others
References
Abe M, Udono H, Tabuchi K, Uchino A, Yoshikai T, Taki K (2003) Analysis of ischemic brain damage in cases of acute subdural hematomas. Surg Neurol 59:464–472
Czosnyka M, Copeman J, Czosnyka Z et al (2000) Post-traumatic hydrocephalus: influence of craniectomy on the CSF circulation. J Neurol Neurosurg Psychiatry 68:246–248
Droste DW, Ritter MA, Dittrich R, Heidenreich S, Wichter T, Freund M, Ringelstein EB (2003) Arterial hypertension and ischemic stroke. Acta Neurol Scand 107:241–251
Greene KA, Marclano FF, Johnson BA, Spetzler RF, Harrington TR (1995) Impact of traumatic subarachnoid hemorrhage on outcome in non-penetrating head injury. J Neurosurg 83:445–452
Brain Trauma Foundation, American Association of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care (1996) Guidelines for the management of severe head injury. J Neurotrauma 13:641–734
Ivanusa M, Ivanusa Z (2004) Risk factors and in-hospital outcomes in stroke and myocardial infarction patients. BMC Public Health 4:26
Macpherson P, Graham DI (1973) Arterial spasm and slowing of the cerebral circulation in the ischemia of head injury. J Neurol Neurosurg Psychiatry 36:1069–1072
Mazzini L, Campini R, Angelino E, Rognone F, Pastore I, Oliveri G (2003) Posttraumatic hydrocephalus: a clinical, neuroradiologic, and neuropsychologic assessment of long-term outcome. Arch Phys Med Rehabil 84:1637–1641
Messing-Junger AM, Marzog J, Wobker G, Sabel M, Book WJ (2003) Decompressive craniectomy in severe brain injury. Zentralbl Neurochir 64:171–177
Mirvis SE, Wolf AL, Numaguchi Y, Corradino G, Joslyn JN (1990) Posttraumatic cerebral infarction diagnosed by CT: prevalence, origin, and outcome. AJR Am J Roentgenol 154:1293–1298
Moulin T, Tatu L, Crepin Leblond T, Chavot D, Berges S, Rumbach T (1997) The Besancon Stroke Registry: an acute stroke registry of 2500 consecutive patients. Eur Neurol 38:10–20
Pasqualin A, Vivenza C, Licata C, Cavazzani P, De Pian R (1984) Cerebral vasospasm after head injury. Neurosurgery 15:855–857
Phillips SJ, Whisnant JP (1992) Hypertension and the brain. The National High Blood Pressure Education Program. Arch Intern Med 152:938–945
Robertson CS, Grossman RG, Goodman JC, Narayan RK (1987) The predictive value of cerebral anaerobic metabolism with cerebral infarction after head injury. J Neurosurg 67:361–368
Rothfus WE, Goldberg AL, Tabas JH, Deeb ZL (1987) Callosomarginal infarction secondary to transfalcial herniation. AJNR Am J Neuroradiol 8:1073–1076
Sacco RL (1995) Risk factors and outcomes for ischemic stroke. Neurology 45:S10–S14
Sato M, Tanaka S, Kohama A, Fujii C (1986) Occipital lobe infarction caused by tentorial herniation. Neurosurgery 18:300–305
Shapiro K, Fried A, Takei F, Kohn I (1985) Effect of the skull and dura on neural axis pressure–volume relationships and CSF hydrodynamics. J Neurosurg 63:76–81
Tomberg TA, Tikk AA (1989) Traumatic cerebral infarct. Zh Vopr Neirokhir Im N N Burdenko (2):23–26 (Mar–Apr)
Uhl E, Kreth FW, Elias B, Goldammer A, Hempelmann RG, Liefner M, Nowak G, Oertel M, Schmieder K, Schneider GH (2004) Outcome and prognostic factors of hemicraniectomy for apace occupying cerebral infarction. J Neurol Neurosurg Psychiatry 75:270–274
Weisberg LA (1979) CT and acute head trauma. Comput Radiol 3:15–28
Wilkens RH, Odom GL (1970) Intracranial arterial spasm associated with craniocerebral trauma. J Neurosurg 32:626–633
Yang X-F, Yao Y, Hu W-W, Li G, Xu J-F, Zhao X-Q, Liu W-G (2005) Is decompressive craniectomy for malignant middle cerebral artery infarction of any worth? J Zhejiang Univ Sci B 6:644–649
Ziai WC, Port JD, Cowan JA, Garonzik IM, Bhardwaj A, Rigamonti D (2003) Decompressive craniectomy for intractable cerebral edema: experience of a single center. J Neurosurg Anesthesiol 15:25–32
Zubkov AY, Pilkington AS, Bernanke DH et al (1999) Posttraumatic cerebral vasopasm: clinical and morphological presentations. J Neurotrauma 16:763–770
Acknowledgments
This study was supported by the Shanghai Municipal Health Bureau (grant no. 054011) and Shanghai Science and Technology Council (grant no. 03ZR14059).
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Jizong Zhao, Beijing, China
Posttraumatic cerebral infarction (PTCI) is one of the most severe secondary injury after brain trauma. It often results in a poor clinical outcome. Thus, recognition of this secondary brain insult and the associated risk factors may help identify the group at risk and tailor management of patients with severe TBI. In this article, the authors defined the incidence and timing of PTCI, described the risk factors after logistic regression analysis, and demonstrated that a low GCS, low systolic BP, herniation, and decompression craniotomy were risk factors for PTCI. This will help neurosurgeons to recognize PTCI in the early stage. In this paper, the patients’ ages ranged from 2 to 86 years; are there differences in the risk factors between children and adults? Since, at present, it is reported that the mechanism is different between children and adults, so perhaps there will be new findings after analyzing the data in subgroups by ages. And what is the reason of PTCI high incidence during the second week, iatrogenic, or other reasons? The author mentioned that aggressive management of PTCI should be recommended. What are effective treatments and how about the outcomes? So a more comprehensive analysis about specific interventions for PTCI is absolutely needed in the future.
Comments
Dattatraya Muzumdar, Mumbai, India
Tian et al. present their experience of posttraumatic cerebral infarction in the management of 353 head trauma patients. They suggest that PTCI should be diagnosed early for prompt institution of treatment and possibly an improved outcome. The use of a sufficiently powered study and multivariable models to predict the long-term outcome of moderate and severe head trauma is a positive nature of this study. The identification of variables like low GCS, low systolic BP, herniation, and decompression craniotomy as risk factors early during the course of moderate to severe head trauma is also an important attribute of this study.
The limitation of the study lies in its retrospective nature. A prospective study with detailed neurologic examination and neuropsychological assessment to demonstrate that the observed morbidity could be attributed to cerebral infarction and not to primary posttraumatic brain damage or to other nonischemic complications would be helpful. A validation of surrogate PTCI outcomes would be useful for research on those measurements that can effectively predict an increased risk of cerebral infarction, hence abandoning measures whose theoretical rationale is not demonstrated. Magnetic resonance imaging, particularly diffusion-weighted and perfusion-weighted techniques, should be used as a reference standard to diagnose brain infarction and clarify whether the use of more sensitive neuroradiologic investigations actually improves detection of posttraumatic cerebral infarction.
The outcome in posttraumatic cerebral infarction is usually dismal since there is a high incidence of mortality and severe morbidity compromising quality of life and increased care cost to the family in particular and the state in general. PTCI occurs due to the severe parenchymal or vascular injury leading to primary and later secondary brain injury releasing free oxygen radicals. Until now, cerebral protective agents like Ca-channel blockers or free oxygen radical scavengers have not shown any significant encouraging results. In essence, the treatment of posttraumatic cerebral infarction lies in prevention and early detection.
Rights and permissions
About this article
Cite this article
Tian, HL., Geng, Z., Cui, YH. et al. Risk factors for posttraumatic cerebral infarction in patients with moderate or severe head trauma. Neurosurg Rev 31, 431–437 (2008). https://doi.org/10.1007/s10143-008-0153-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-008-0153-5