Abstract
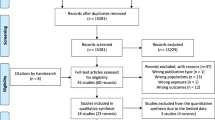
Objective Inconsistent findings of associations between gestational diabetes mellitus (GDM) and birth defects suggest unaccounted confounders may underlie the actual basis for such associations. We conducted a systematic review to assess observed associations between GDM and birth defects and the extent to which these could be explained by pre-pregnancy obesity. Methods Using a combination of search terms for GDM and birth defects, we searched PubMed, Scopus, CINAHL, and ClinicalTrials.gov for human-based studies published through September 2013. Studies were eligible for inclusion if they included information on maternal diabetes status, method of diagnosis of GDM, and assessment of birth defects. Twenty-four of 768 potential articles were included. We collected information on study design, location and period, method of determination of diabetes status, types of birth defects, and measures of association reported. Results There was no evidence for consistent association of GDM with birth defects, with the exception of a weak association between GDM and congenital heart defects. When stratified by maternal pre-pregnancy BMI, an association between GDM and congenital heart defects and between GDM and neural tube defects was evident only in women with both GDM and pre-pregnancy obesity. Conclusions for Practice Our findings suggest reported associations between GDM and birth defects may be due, in part, to undiagnosed metabolic disorders associated with obesity, such as pregestational diabetes mellitus, rather than GDM. These findings highlight the need for increased efforts for pre-pregnancy screening for undiagnosed diabetes and awareness of the importance of weight management among women of childbearing age with obesity.

Similar content being viewed by others
References
Aberg, A., Westbom, L., & Kallen, B. (2001). Congenital malformations among infants whose mothers had gestational diabetes or preexisting diabetes. Early Human Development, 61(2), 85–95.
Abolfazl, M., Hamidreza, T. S., Narges, M., & Maryam, Y. (2008). Gestational diabetes and its association with unpleasant outcomes of pregnancy. Pakistan Journal of Medical Sciences, 24(4), 566–570.
Agopian, A. J., Moulik, M., Gupta-Malhotra, M., Marengo, L. K., & Mitchell, L. E. (2012). Descriptive epidemiology of non-syndromic complete atrioventricular canal defects. Paediatric and Perinatal Epidemiology, 26(6), 515–524. doi:10.1111/ppe.12006.
Agopian, A. J., Tinker, S. C., Lupo, P. J., Canfield, M. A., & Mitchell, L. E. (2013). Proportion of neural tube defects attributable to known risk factors. Birth Defects Research Part A, 97(1), 42–46. Retrieved, from http://www.ncbi.nlm.nih.gov/pubmed/23427344.
Anderson, J. L., W, D. K., Canfield, M. A., Shaw, G. M., Watkins, M. L., & Werler, M. M. (2005). Maternal obesity, gestational diabetes, and central nervous system birth defects. Epidemiology, 16(1), 87–92.
Aryasinghe, L., M, D., Ansari, T. A., Khoury, R., Mathew, E., Sharbatti, S. A., & Shaikh, R. B. (2012). Congenital anomalies at birth: A hospital based study in UAE. Journal of Nepal Paediatric Society, 32(2), 105–112.
Correa, A., Gilboa, S. M., Besser, L. M., Botto, L. D., Moore, C. A., Hobbs, C. A., … Reece, E. A. (2008). Diabetes mellitus and birth defects. American Journal of Obstetrics and Gynecology, 199(3), 237.e231–239. doi:10.1016/j.ajog.2008.06.028.
Correa, A., & Marcinkevage, J. (2013). Prepregnancy obesity and the risk of birth defects: An update. Nutrition Reviews, 71(Suppl 1), S68–77. doi:10.1111/nure.12058.
Fadl, H. E., Ostlund, I. K., Magnuson, A. F., & Hanson, U. S. (2010). Maternal and neonatal outcomes and time trends of gestational diabetes mellitus in Sweden from 1991 to 2003. Diabetic Medicine, 27(4), 436–441. doi:10.1111/j.1464-5491.2010.02978.x.
Ferencz, C., Rubin, J. D., McCarter, R. J., & Clark, E. B. (1990). Maternal diabetes and cardiovascular malformations: Predominance of double outlet right ventricle and truncus arteriosus. Teratology, 41(3), 319–326. doi:10.1002/tera.1420410309.
Finer, L. B., & Zolna, M. R. (2011). Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception. doi:10.1016/j.contraception.2011.07.013.
Garcia-Patterson, A., Erdozain, L., Ginovart, G., Adelantado, J. M., Cubero, J. M., Gallo, G., … Corcoy, R. (2004). In human gestational diabetes mellitus congenital malformations are related to pre-pregnancy body mass index and to severity of diabetes. Diabetologia, 47(3), 509–514. doi:10.1007/s00125-004-1337-3.
Gasim, T. (2012). Gestational diabetes mellitus: maternal and perinatal outcomes in 220 saudi women. Oman Medical Journal, 27(2), 140–144. doi:10.5001/omj.2012.29.
Gilboa, S. M., Correa, A., Botto, L. D., Rasmussen, S. A., Waller, D. K., Hobbs, C. A., … Riehle-Colarusso, T. J. (2010). Association between prepregnancy body mass index and congenital heart defects. American Journal of Obstetrics and Gynecology, 202(1), 51.e51–51.e10. doi:10.1016/j.ajog.2009.08.005.
Inkster, M. E., Fahey, T. P., Donnan, P. T., Leese, G. P., Mires, G. J., & Murphy, D. J. (2006). Poor glycated haemoglobin control and adverse pregnancy outcomes in type 1 and type 2 diabetes mellitus: Systematic review of observational studies. BMC Pregnancy and Childbirth, 6, 30. doi:10.1186/1471-2393-6-30.
Janssen, P. A., Rothman, I., & Schwartz, S. M. (1996). Congenital malformations in newborns of women with established and gestational diabetes in Washington State, 1984–91. Paediatric and Perinatal Epidemiology, 10(1), 52–63. Retrieved, from http://www.ncbi.nlm.nih.gov/pubmed/8746431.
Lapolla, A., Dalfra, M. G., Bonomo, M., Parretti, E., Mannino, D., Mello, G., & Di Cianni, G. (2009). Gestational diabetes mellitus in Italy: A multicenter study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. doi:10.1016/j.ejogrb.2009.04.023.
Mannan, M. A., Rahman, M. H., Ara, I., & Afroz, H. (2012). Prevelence and pregnancy outcome of gestational diabetes mellitus among Bangladeshi urban pregnant women. Journal of Medicine (Bangladesh), 13(2), 147–151.
Martinez-Frias, M. L., Frias, J. P., Bermejo, E., Rodriguez-Pinilla, E., Prieto, L., & Frias, J. L. (2005). Pre-gestational maternal body mass index predicts an increased risk of congenital malformations in infants of mothers with gestational diabetes. Diabetic Medicine, 22(6), 775–781. doi:10.1111/j.1464-5491.2005.01492.x.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., The Prisma Group (2009). Preferred reporting items for systemic reviews and meta-analyses: The Prisma Statement. Journal of Clincal Epidemiology, 62, 1006–1012.
Moore, L. L., Singer, M. R., Bradlee, M. L., Rothman, K. J., & Milunsky, A. (2000). A prospective study of the risk of congenital defects associated with maternal obesity and diabetes mellitus. Epidemiology, 11(6), 689–694.
Mosher, W. D., Jones, J., & Abma, J. C. (2012). Intended and unintended births in the United States: 1982–2010. National Health Statistics Reports, 55, 1–28. Retrieved, from http://www.ncbi.nlm.nih.gov/pubmed/23115878.
Pablo Velazquez, G., Genero, V. M., & Martha Leticia Martinez, M. (2010). Neonatal morbidity and mortality associated with gestational diabetes. Revista Chilena de Obstetricia y Ginecologia, 75(1), 35–41.
Porter, M. P., Faizan, M. K., Grady, R. W., & Mueller, B. A. (2005). Hypospadias in Washington State: Maternal risk factors and prevalence trends. Pediatrics, 115(4), e495–e499. doi:10.1542/peds.2004-1552.
Ramachandran, A., Snehalatha, C., Clementina, M., Sasikala, R., & Vijay, V. (1998). Foetal outcome in gestational diabetes in south Indians. Diabetes Research and Clinical Practice, 41(3), 185–189.
Ramos-Arroyo, M. A., Rodriguez-Pinilla, E., & Cordero, J. F. (1992). Maternal diabetes: the risk for specific birth defects. European Journal Epidemiology, 8(4), 503–508. Retrieved, from http://www.ncbi.nlm.nih.gov/pubmed/1397216.
Reece, E. A., Ma, X. D., Wu, Y. K., & Dhanasekaran, D. (2002). Aberrant patterns of cellular communication in diabetes-induced embryopathy. I. Membrane signalling. The Journal of Maternal-Fetal & Neonatal Medicine, 11(4), 249–253. doi:10.1080/jmf.11.4.249.253.
Reece, E. A., Ma, X. D., Zhao, Z., Wu, Y. K., & Dhanasekaran, D. (2005). Aberrant patterns of cellular communication in diabetes-induced embryopathy in rats: II, apoptotic pathways. American Journal of Obstetrics and Gynecology, 192(3), 967–972. doi:10.1016/j.ajog.2004.10.592.
Savona-Ventura, C., & Gatt, M. (2004). Embryonal risks in gestational diabetes mellitus. Early Human Development, 79(1), 59–63. Retrieved, from http://www.ncbi.nlm.nih.gov/pubmed/15449398.
Sheffield, J. S., Butler Koster, E.L., Casey, B.M., McIntire, D.D., Leveno, K.J. (2002). Maternal diabetes mellitus and infant malformations. Obstetrics and Gynecology, 100(5), 925–930.
Shnorhavorian, M., Bittner, R., Wright, J. L., & Schwartz, S. M. (2011). Maternal risk factors for congenital urinary anomalies: Results of a population-based case-control study. Urology. doi:10.1016/j.urology.2011.04.022.
Stothard, K. J., Tennant, P. W., Bell, R., & Rankin, J. (2009). Maternal overweight and obesity and the risk of congenital anomalies: A systematic review and meta-analysis. JAMA, 301(6), 636–650. doi:10.1001/jama.2009.113.
Van Bennekom, C. M., Mitchell, A. A., Moore, C. A., & Werler, M. M. (2013). Vasoactive exposures during pregnancy and risk of microtia. Birth Defects Research. Part A, 97(1), 53–59. doi:10.1002/bdra.23101.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Rights and permissions
About this article
Cite this article
Parnell, A.S., Correa, A. & Reece, E.A. Pre-pregnancy Obesity as a Modifier of Gestational Diabetes and Birth Defects Associations: A Systematic Review. Matern Child Health J 21, 1105–1120 (2017). https://doi.org/10.1007/s10995-016-2209-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-2209-4