Abstract
Objectives : To determine the health and nutritional status of rural Chinese children ages 12–24 months. Methods: This study used a cross-sectional design with a longitudinal component. Anthropometry and blood chemistry were measured on each child twice (n = 250). Caretaker knowledge and behaviors that relate to the child’s health and diet were evaluated by interview. Results: Children were taken outdoors at an average age of 131.8 days. 65.3% of surveyed children had serum 25-OH-D levels less than 12 ng/ml in the spring. This declined to 2.8% in the fall. Mean blood lead levels were 15.7 ± 11.0 μg/dl in the spring declining to 12.4 ± 12.5 μg/dl in the fall (t = 6.47, P = 0.000). This still left 63.5 and 54.9% of the children with toxic blood lead levels in spring and fall. Rates of respiratory disease declined significantly from spring to fall. A summer outdoors remarkably improved vitamin D-deficiency and lead toxicity. However, nutritional status worsened as during the summer diet was unable to keep up with growth and increased nutritional demand. From spring to fall serum zinc declined from 0.77 ± 0.19 to 0.66 ± 0.21 μg/ml (t = 3.33, P = 0.001) and blood hemoglobin declined from 12.5 ± 1.2 to 12.0 ± 1.2 gm/dl (t = 4.07, P = 0.000). Conclusions: Northern climate and cloistering of children creates a host of health risks for north China children. Vitamin D-deficiency, lead poisoning and respiratory disease are significantly worse during the winter months. These children need vitamin D supplementation during the winter and improved overall nutritional status during the summer to maintain ideal growth and development.
Similar content being viewed by others

Introduction
China is in an era of rapid, but imbalanced economic development. While children in urban areas receive high quality health care, children in rural areas continue to be cared for by poorly trained doctors and with limited medical equipment [1, 2]. Shen et al [3] report 38% of rural children aged 2–5 had moderate stunting and 15% had severe stunting, as compared with 10 and 3% among urban children. The health of these rural children is of interest to people concerned about equitable development globally. This paper will report on the overall health of young children in rural north China, focusing on disease outcomes, micronutrient deficiencies and lead toxicity.
Of continual concern in north China is the highly prevalent problem of vitamin D-deficiency. In a Beijing study sixty-four 12 to 14-year-old girls had a mean 25(OH)D level of 12.8 ± 6.7 nmol/l in winter [4]. Shanxi Province children with rickets have been shown to exhibit significantly lower 25(OH)D levels (36.23 ± 20.23 nmol/l) than controls (49.88 ± 13.55 nmol/l) [5].
Zinc insufficiency is associated with pneumonia [6], diarrhea, and stunting [7, 8]. The role of zinc in the immune system implicates low zinc intake as a possible contributor to many childhood illnesses [9].
In an era of rapid urbanization, it is easy to ignore the vast majority of the population who are not participating in the urbanization process. If urbanization and economic development deepens the rural–urban divide and worsens health disparities, China as a whole will suffer. This study reports on the health and nutritional status of rural children age 12–24 months in north China. This fills a research void that exists for characterization and basic understanding of the health of children in rural China.
Materials and Methods
Subjects
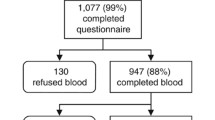
Subjects are 250 young children between 12 and 24 months of age. The research design is a cross-sectional design with a longitudinal component (data gathered in April and then again on the same cohort of children in September 2003), relying on the retrospective evaluation of caretaker knowledge and behaviors that relate to the child’s illness or health. A multi-stage cluster sampling (non-probability) method was used. Three townships in Yuci were selected representing a mountainous and remote location, and two locations in the plains. Villages (the cluster) were then selected randomly and all qualifying women and their children within each village were invited to participate.
Fourteen villages were samples. Excluded from the study were mothers lacking the cognitive ability to participate (1), immigrants to Yuci (0), infants born before 37 weeks gestation (2), children away from the village for the majority of their life (0), and children who were significantly disabled, mentally or physically, in fashions unrelated to rickets (1).
Data Analysis
Data analyses were carried out using SPSS (version 11.0). Several correlation coefficients (Pearson and rho) were used and P-values presented. All statistical tests were performed using an alpha of 0.05 which was used as the criterion of statistical significance.
Interview
Three female workers from the Yuci Maternal and Child Health Hospital were trained to conduct interviews using a 33-question survey designed by the researchers using the local language, Mandarin Chinese. The interviewer was blinded to any diagnostic or laboratory outcomes on the child; however, the interviewer could often see the child if he or she was being held by the caregiver.
A socio-economic status (SES) scale was created from a summary of family possessions—DVD/TV system, motorcycle, refrigerator, washing machine and telephone/mobile phone with scale from 0 (none of these possessions) to 5 (possessed all five). Scale reliability analysis comparing inter-item reliability between the five variables entered revealed a Chronbach’s alpha coefficient of 0.579.
Illness History
Child’s illness history was assessed by asking the mother three questions: Has your infant experienced any illnesses in the last week and what was it? Has your child experienced any illnesses in the last month and what was it? In the recent 6 months, has your child experienced any of the following illnesses? Listed were diarrhea, pneumonia, bronchitis, upper respiratory tract infection, and anemia. The first two questions were open-ended, allowing the mother to report what she remembered. The third question was meant as a prompt to the mother to help her consider in a more focused way whether her child had experienced any of the illnesses listed. Definitions used for illnesses followed the WHO IMCI (Integrated Management of Childhood Illness) definitions as follows [10]:
-
(1)
Diarrhea = More than three loose watery stools a day lasting for a few days or more (not routine soft stools, but out of the ordinary).
-
(2)
Pneumonia = Diagnosed by a doctor. (Defined as Respiratory infection with (a) Fast breathing, (b) Lower chest wall indrawing, or (c) Stridor.).
-
(3)
Bronchitis (recurring respiratory infection) = More than three times in recent 6 months.
-
(4)
Upper respiratory tract infection = Respiratory infection with fast breathing.
-
(5)
Anemia = Has your child been tested for anemia? Were you told by a doctor that he/she had anemia? Deficiency defined as blood Hemoglobin <11.5 g/dl.
-
(6)
Stunting = Height for age z-score below—2SD
-
(7)
Underweight = Weight for age z-score below—2SD
Anthropomorphic Measures
Body weight was measured using a beam-balance platform scale with a multipurpose bed-chair mounted on the platform. The scale was manufactured in Wuxi, China at the Wuxi Scale Factory (Ertong Chen (Child scale), model number RGT-50, maximum weight 50 kg). Chinese parents are reluctant to allow their infants to be fully unclothed, so infants wore one layer of standard clothing. The weight of a representative set of clothes was subtracted from the measured weight.
Recumbent length was measured using an aluminum measuring board manufactured in China by Nantong Instruments Factory, Nantong, China (Yingyouer shengao zuogao ji (Child and infant length measuring board), Sangong pai brand, model YSL-1, serial number 3037). The measuring range was 50–1,050 mm, with a variability of 1 mm. Weight-for-age, and height-for-age z-scores were calculated using ANTHRO (version 1.02, 29 June 1999, CDC/WHO), which is based on United States NCHS standards.
Blood Chemistry Measures
Two milliliter of blood (non-fasting) was collected by venipuncture on the inside of the elbow by manual extraction using a 5 ml plastic disposable injection syringe. All equipment used in collection such as Eppendorf tubes and micropippette were soaked in 10% nitric acid for 24 h, then washed clean by distilled water, ionized water, and dried to use. In pipetting, a new tip was used each time. All blood work was done in the laboratory of the Department of Nutrition Sciences at the Shanxi University Medical University.
-
(1)
Serum 25(OH)D was measured using the 25-Hydroxyvitamin D 125I Radioimmunoassay Kit manufactured by DiaSorinInc. (Stillwater, MN, USA).
-
(2)
Blood hemoglobin was measured by spectrophotometry using the Drab kin’s method.
-
(3)
Blood lead was assayed using Graphite Oven Atomic Absorption Spectrometry.
-
(4)
Hemoglobin levels were assayed using the Drab kin’s method. Serum zinc was assayed using the flame atomic absorption spectrophotometric method.
Except for 25(OH)D, controls were supplied by the China Academy of Science Medicine Institute of Environment and Health.
Informed Consent
Verbal informed consent was obtained from all subjects according to procedures approved by the Institutional Review Boards of the University of Colorado-Denver (Human Subjects Protocol number 875) and Shanxi Province Public Health Bureau (Shanxi Province Public Health Bureau Office Document No. 22, 2002).
Results
Study Population
In the spring phase of the study the children ranged in age from 12 to 24 months (Table 1). Participation rate in the spring was 80.5% and the return rate in the fall was 70.4%. The average age of mothers was 28.3 ± 4.2 years in the spring. 16.8% of mothers surveyed had completed senior high school or college. 69.5% had completed junior high school (9 years of education). 10.9% had completed primary school. 2.8% were illiterate. 73.6% of mothers breast-fed their infant the first 6 months of life and they weaned them at an average age of 15.9 ± 5.4 months. These children were not taken outdoors until they were an average of 131.8 days old. They began eating solid foods at 6.42 ± 2.3 months of age.
Blood Chemistry Markers
As a measure of health and nutritional status, blood tests were done on participating children in both the spring and fall (Table 2). Blood levels of hemoglobin and zinc declined from spring to fall a significant amount. The percentage of children with blood Hgb levels below 11.5 gm/dl nearly doubled, increasing from 14.0 to 27.8% (Table 2). This represented a mean Hgb level decline during the 5-month interval from 12.5 to 12.0 gm/dl (paired samples t = 4.07, df = 146, P = 0.000). 1.8% of children in the spring and 4.1% in the fall had Hgb levels below the norm of 10 gm/dl.
Mean zinc level declined from 0.77 ± 0.19 to 0.66 ± 0.21 μg/ml from spring to fall (Table 2), and this decline was statistically significant (paired samples t = .3.3, P = 0.001, n = 87). Also, the number of children whose serum zinc levels fell below 0.60 μg/ml increased from 14.8 to 39.1% from spring to fall (Table 2). Zinc insufficiency in populations tends to result in more frequent and severe infections, but zinc-insufficiency was not associated with pneumonia or diarrhea in this study.
In the spring 65.3% of surveyed children were found to be vitamin D-deficient (25-OH-D < 12 ng/ml). In this northern climate, with extended time indoors in the winter, and only 4.2% of children given vitamin D supplements often in the recent month, vitamin D-deficiency is inevitable (Table 3). After a summer of sun exposure the percentage vitamin D-deficient was reduced to 2.9%.
Mean serum 25-OH-D levels for males was 16.96 ± 34.49 ng/ml compared to 10.21 ± 12.91 for girls, and this difference was shown to be statistically significant (t = −1.76, P = 0.082).
Toxic Lead Levels
In the spring 63.5% of children had blood lead levels over the acceptable limit of 10 μg/dl. Repeated blood tests on 184 children in the fall, revealed that 54.9% of the children still had blood lead levels over the 10 μg/dl limit. Mean blood lead level declined from spring to fall (15.7 ± 11.0 μg/dl vs. 12.4 ± 12.5) and this decline was statistically significant (t = 6.47, P = 0.000).
Blood lead levels were found to be negatively associated with socioeconomic status of the family (r = −0.23, P = 0.002), education level of the mother (r = −0.16, P = 0.019), and number of children in the home (r = 0.19, P = 0.007).
Disease Outcomes
The attack rate in the recent 6 months of infectious diseases was diarrhea 25.6%, pneumonia 9.2%, bronchitis 17.7%, and upper respiratory tract infection (URI) 14.1%. Attack rates for each of these diseases declined significantly from spring to fall (Table 4), except for diarrhea whose decline was not statistically significant. The reported rate of anemia increased, which parallels the measured blood Hgb decline from spring to fall (Table 2), although the decline in reported anemia was not statistically significant.
Height for age z-scores showed an increase from spring to fall (Table 4), so the children’s height was getting closer to the NCHS standard. This may reflect the remarkable healing of rickets during that same time period [11]. The percent of malnourished children (weight-for-age z-score below 2 standard deviations below the mean on NCHS standards) increased from spring to fall but a statistically insignificant amount.
Discussion
Nutritional Deficiencies
This study found that in the spring, after a long winter, 65.3% of the children had serum 25-OH-D levels below 12 ng/ml. Even though the 25-OH-D levels of most of the children returned to normal by September of the same year, these children were living long periods of time with severe vitamin D-deficiency, which may have contributed to disease outcomes. Infants with vitamin D-deficiency suffer in myriad ways. In addition to the skeletal abnormalities of rickets [12], vitamin D-deficiency is associated with pneumonia [13, 14], stunting, and gastrointestinal infections [15]. Vitamin D-deficiency in infancy is also suspected to lead to adult morbidities such as Type I diabetes [16], hypertension [17] and breast, ovarian, prostate, and colorectal cancers [18], and there is even a putative relationship between vitamin D-deficiency and tuberculosis [19].
About 73.6% of these children were breast-fed their first 6 months of life and this continued to around 16 months of age. High rates of prolonged breast-feeding have been shown to be beneficial among Chinese children [20]. Children in this study began life with a nutritional advantage, but then lost it as introduction of solid foods was somewhat delayed (6.42 ± 2.3 months of age) but even more so, these children were not taken outdoors until they were an average of 131.8 days of age, thus missing out on the benefits of solar-derived vitamin D.
This study discovered high rates of serum zinc levels below the norm of 0.60 μg/ml, and the percentage of children abnormal increased from spring to fall (14.8 and 39.1%). Hemoglobin and zinc both declined significantly from spring to fall, possibly due to low intake of protein and animal-based foods during the summer months [21]. This study also found high rates of diarrhea and respiratory illness among surveyed children. Anemia is commonly found in protein energy malnutrition (PEM) which may adversely affect immune function and resistance to infection [22]. Previous research has found zinc supplementation in regions of general zinc insufficiency to reduce rates of diarrhea and pneumonia [23, 8]. A new study in Bangladesh showed that zinc added to a standard antibiotic helped hospitalized children with pneumonia recover faster [6]. It is possible that general zinc insufficiency over time is contributing to the burden of disease among children in this survey.
Shanxi children live in a context of low intake of zinc, protein and iron [21], and have low levels of 25-OH-D. This combination of dietary deficiencies puts these children at increased risk of infections such as pneumonia and diarrhea. Low iron intake and ensuing anemia further compromises vitamin D absorption, thus contributing to the problem of vitamin D-deficiency. Having largely solved the problem of undernutrition, China now faces the challenge of ensuring every child a balanced diet with adequate amounts of crucial minerals and vitamins.
Between 3.3 and 4.3% of these children are stunted. WHO has estimated that 50–70% of all childhood deaths from infectious diseases are attributed to the child being underweight [24]. This may be contributing to the rates of infectious disease found in this study.
In summary, through the summer these children’s weight-for-age decreased, height-for-age increased and they have lower blood levels for most of the micro and macronutrients tested in this study. An increase in physical activity during the summer coupled with growth demands, increase children’s nutritional needs. Based on dietary and blood micronutrient measures, it appears that this need was not being met. However, as of the fall, these children experienced less illness and much of the rickets they had previously was healed, so something beneficial was occurring as well. The two most obvious changes are development and improved vitamin D status through increased sun exposure.
Solving Nutrition Deficiencies in Rural China
People need adequate sun exposure [25–30], especially growing children at risk for rickets and associated diseases. Zlotkin et al. [31] found an association between the use of sunscreen and rickets. Education and public health information in China need to promote practices that lead to good vitamin D health and aid in preventing rickets, osteoporosis and other associated diseases.
How to solve nutritional deficiencies in children in contexts of poverty is a global health challenge. Universal vitamin distribution has been widely promoted and successful in some cases, but it is being questioned [32]. Food-based solutions relying on the integration of the agricultural system with the health system so that the foods produced meet crucial nutritional imbalances [33] seems the best approach for China.
Lead Toxicity
The decline in rate of lead toxicity from 63.5% in the spring to 54.9% in the fall may be a result of being out of the lead contamination in the home. In a follow-up study to this research it was discovered that the main route of exposure for these children was through the burning of contaminated coal in their homes where children then inadvertently ingested the coal dust [34]. Frequency of hand-washing was actually found to be negatively associated with blood lead levels.
We have shown that blood lead levels of children correlate with SES, mother’s education and number of children in the home. This creates a picture of poverty and low education found in those families whose children have high lead levels. The negative influence of lead pollution on children’s intellectual and physical development has been well documented [35, 36], including China [37–41]. So these children are in a negative cycle. Researchers in China have spent much effort to investigate the extent of lead poisoning, and following the discovery of a wide-spread prevalence of lead poisoning in cities, the government took public policy steps to limit the problem. After phasing out leaded gas in 1997 within 2 years the prevalence of childhood lead poisoning fell by 35% in Shanghai [39]. Such measures have not taken hold in rural areas.
Research Limitations
Behavior is hard to operationalize and hard to measure. The inherent normative bias of surveys is hard to avoid, making it challenging to detect significance. Interviewer bias and recall bias may have influenced the accuracy of survey results.
Unique Contributions of this Study
In the early 1990s Popkin and Ge published a monumental series of papers on the nutritional status of adults and children in China with evidence from both rural and urban contexts [42]. The 1990s represented a massive migration of people from rural to urban areas in China, with a new focus and prioritization of urban trends in China. This has been at the expense of rural areas and the majority of the people who still live there. This paper fills a research gap on the health and nutritional status of children in rural China in the modern era.
References
Dong, Y. (2000). Contrasting on supply and demand of the medical health services between city and village (Chinese). China Public Health, 16(1), 82–83.
Shi, L. (1993). Health care in China: A rural–urban comparison after the socioeconomic reforms. Bulletin of the World Health Organization, 71(6), 723–736.
Shen, T., Habicht, J. T., & Chang, Y. (1996). Effect of economic reforms on child growth in urban and rural areas of China. NEJM, 335(6), 400–406.
Du, X. Q., Greenfield, H., Fraser, D. R., Ge, K. Y., Trube, A., & Wang, Y. Z. (2001). Vitamin D deficiency and associated factors in adolescent girls in Beijing. American Journal of Clinical Nutrition, 74, 494–500.
Zhang, H., Chen, Y. L., Huang, W., & Xue, Y. (1999). Serum 25(OH)D3 levels in rachitic children before and after vitamin D supplementation. (Chinese) Zhongguo Gonggong Weisheng (China Public Health), 15, 705.
Brooks, W., Yunus, M., Santosham, M., Wahed, M. A., Nahar, K., & Yeasmin, S., et al (2004). Zinc for severe pneumonia in very young children: Double-blind placebo-controlled trial. Lancet, 363(9422), 1683–1688. .
An, H., Yin, S., & Zu, Q. (2001). Effects of supplementing calcium, iron and zinc on the fetus development and growth during pregnancy. Zhonghua Yufang Yuxie Zazhi. (China Journal of Preventive Medicine), 35(6), 370–373.
Umeta, M., West, C. E., Haidar, J., Deurenberg, P., & Hautvast, G. A. J. (2000). Zinc supplementation and stunted infants in Ethiopia: A randomised controlled trial. Lancet, 355, 2021–2008.
Shankar, A. H., & Prasad, A. S. (1998). Zinc and immune function: The biological basis of altered resistance to infection. The American Journal of Clinical Nutrition, 68(suppl), 447S–463S.
World Health Organization. (2001). IMCI (Integrated Management of Childhood Illness). Geneva: World Health Organization and UNICEF 32.
Strand, M. A., Perry, J., Jin, M. M., Tracer, D. P., Fischer, P. R., & Zhang, P. Y., et al (2007). Diagnosis of rickets and reassessing its prevalence among rural children in Northern China. Pediatrics International (in press), 49(2).
Strand, M. A., & Lee, G. (2003). Preventing rickets in locally appropriate ways: A case report from North China. International Quarterly of Community Health, 21(4), 293–318.
Barness, L. (1987). Nutrition and nutritional disorders. In R. E. Behrman, V. C. Vaughan, & W. E. Nelson (Eds.), Nelson Textbook of Pediatrics (pp. 113–154). Philadelphia: WB Saunders.
Muhe, L., Lulseged, S., Mason, K. E., & Somoes, E. A. (1997). Case–control study of the role of nutritional rickets in the risk of developing pneumonia in Ethiopian children. Lancet, 349, 1801–1804.
Hassan, N., & Combs, G. F. J. (2000). Household risk factors for rickets in Bangladesh. Improving health and economics development: Approaches to preventing diet-related rickets, Dhaka, Bangladesh. Ithaca, NY: Cornell University. .
Hypponen, E., Laara, E., Reunanen, A., Jarvelin, M. R., & Virtanen, S. M. (2001). Intake of vitamin D and risk of type 1 diabetes: A birth-cohort study. Lancet, 358, 1500–1503.
Krause, R., Buhring, M., Hopfenmuller, W., Holick, M. F., & Sharma, A. M. (1998). Ultraviolet B and blood pressure. Lancet, 352, 709–710.
Vieth, R. (1999). Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. The American Journal of Clinical Nutrition, 69, 842–856.
Wilkinson, R. J., Llewlyn, M., & Toossi, Z., et al (2000). Influence of vitamin D deficiency and vitamin D receptor polymorphisms on tuberculosis among Gujarati Asians in west London: A case–control study. Lancet, 355, 618–621.
Prentice, A. (1996). Extended breast-feeding and growth in rural China. Nutrition Reviews, 52(4), 144–146.
Strand, M. A. (2004). Determinants of rickets in Chinese children and associated health outcomes. Dissertation, Department of Health and Behavioral Science. Denver, CO: University of Colorado at Denver.
Tsang, R. C., Zlotkin, S. H., Nichols, B. L., & Hansen, J. W. (Eds.) (1997) Nutrition during infancy: Principles and practice 2nd edition. Cincinnati, OH: Digital Education Publishing, Inc. Chapter ten.
Manary, M. J., Hotz, C., Krebs, N. F., Gibson, R. S., Westcott, J. E., & Arnold, T., et al (2000). Dietary phytate reduction improves zinc absorption in Malawian children recovering from tuberculosis but not in well children. Journal of Nutrition, 130, 2959–2964.
WHO. (2002). The World Health Report – Reducing risks, promoting healthy life. Geneva: World Health Organization.
Bishop, N. (1999). Rickets today – Children still need milk and sunshine. New England Journal of Medicine, 341(8), 602–604.
Nowak, R. (2002). Catch the rays: Sunshine before birth could be crucial for brain development. New Scientist, 173, 7.
Studzinski, G. P., & Moore, DC. (1995). Sunlight – Can it prevent as well as cause cancer? Cancer Research, 55, 4014–4022.
Xiao, W. (2001). Tao Yisheng de ‘Ziran Liaofa.’ (Dr. Tao’s ‘Natural Therapy’). Tian Feng, 224(8), 20.
Holick, M. F. (2006). Resurrection of vitamin D deficiency and rickets. Journal of Clinical Investigation, 116(8), 2062–2072.
Holick, M. F. (2004). Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. The American Journal of Clinical Nutrition, 80(suppl), 1678S–1688S.
Zlotkin, S. H. (1999). Limited vitamin D intake and use of sunscreens may lead to rickets. BMJ, 318, 1417.
Black, J., & Loff, B. (2001). Ways of getting vitamin A to children in developing countries have to be improved. BMJ, 322, 995.
Duxbury, J. M. (2000). Agricultural opportunities to improve human nutrition in Bangladesh: Relevance to rickets prevention. Improving health and economics development: Approaches to preventing diet-related rickets, Dhaka, Bangladesh. Ithaca, NY: Cornell University.
Perry, J. (2005). Personal communication.
Canfield, R. L., Jr Henderson, C. R., Cory-Slechta, D. A., Cox, C., Jusko, T. A., & Lanphear, B. P. (2003). Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. New England Journal of Medicine, 348(16), 1517–1526.
Tong, S., Baghurst, P. A., Sawyer, M. G., Burns, J., & McMichael, A. J. (1998). Declining blood lead levels and changes in cognitive function during childhood. JAMA, 280(22), 1915–1919.
Liu, J., & Liu, D. (2000). A survey of Taiyuan City 521 infants and children blood lead levels and influencing factors. (Chinese) Zhongguo Gonggong Weisheng (China Public Health), 16(4), 357–358.
Shen, X. (1996). Childhood lead poisoning in China. The Science of the Total Environment, 181, 101–109.
Yan, C., Shen, X., Xue, M. P., Yu, X. G., Jin, X. M., & Zhang, Y. P., et al (2003). A clinical analyses of 102 patients with childhood lead poisoning in Shanghai. (Chinese). Linchuang erke zazhi (Journal of Clinical Pediatrics), 21(4), 235–238.
Zhao, L., Zhu, G., Zhang, B. P., Wu, H. Y., Li, H. B., & Guo, B. C., et al (2003). Investigation on children’s blood lead level in urban areas of Henan Province. (Chinese) Zhongguo gonggong weisheng (China Journal of Public Health), 19(9), 1098–1099.
Zhao, Y., Xiong, H., Lei, X. Y., & Zhang, H. (2000). Lanzhou city survey of infant blood lead levels and analysis of reasons. (Chinese). Clinical Pediatric Journal 18(6), 365.
Popkin, B. M., Keyou, G., Zhai, F. Y., Guo, X. G., Ma, H. J., & Zohoori, N. (1993). The nutrition transition in China: a cross-sectional analysis. European Journal of Clinical Nutrition, 47, 333–346.
Acknowledgements
With gratitude to those who diligently completed this project in the face of SARS: Ni Shuhua, Gao Zhuqi, Xi Weiping, Guan Xiaoli, Liu Qiao’e, Wei Yuqin, Zhang Haizhen, Li Caihong, Jin Meimei, Jia Yihong, Wang Aiai, Zhao Runshou and Guo Jinzhi. This project was partially funded by the Nestle Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strand, M.A., Perry, J., Zhao, J. et al. Severe Vitamin D-deficiency and the Health of North China Children. Matern Child Health J 13, 144–150 (2009). https://doi.org/10.1007/s10995-007-0250-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-007-0250-z