Abstract
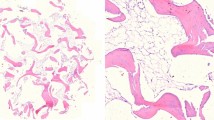
Aseptic and septic periprosthetic osteolysis following total hip arthroplasty has become increasingly recognized as a major clinical problem. An aggressive granulomatous tissue, the interfacial membrane, develops at the interface between the bone and the prostheses or the bone and the cement. Our hypothesis was that during the septic and aseptic loosening of the total hip arthroplasty, there is a clear pathological abnormality in the tissue elements building up the interfacial membrane, which is responsible for the different aetiologies of the disease and could be monitored besides the classical methods by differential scanning calorimetry. In our study, the interfacial membrane pieces removed during operations of revision hip arthroplasties in the cases of aseptic loosening and during prosthesis removals in the cases of septic implant loosening. We investigated stem parts of cemented hip arthroplasties only. Our measurements were carried out on eight septic and 12 aseptic samples. With our investigations, we could demonstrate that DSC is a useful and well-applicable method for the investigation of the interfacial membrane that develops in septic and aseptic loosening of hip arthroplasty. DSC scans clearly demonstrated significant differences between the different types and conditions of samples (aseptic membrane: T m = 62.2 °C and ΔH cal = 2.13 J/g, septic membrane: T m = 60.2 °C and ΔH cal = 3.22 J/g,). These investigations can help us make a correct diagnosis in the problematic cases of loosened total hip arthroplasty. To decide the possible septic feature of a given sample, calorimetry could serve as one of the quickest procedures available.


Similar content being viewed by others
References
Goodman SB, Ma T. Cellular chemotaxis induced by wear particles from joint replacements. Biomaterials. 2010;31:5045–50.
Glant TT, Jacobs JJ, Mikecz K, Yao J, Chubinskaja S, Williams JM, Urban RL, Shanbhag AS, Lee SH, Sumner DR. Particulate-induced, prostaglandin- and cytokine-mediated bone resorption in an experimental system and in failed joint replacements. Am J Ther. 1996;3:27–41.
Yao J, Glant TT, Lark MW, Mikecz K, Jacobs JJ, Hutchinson NI, Hoerrner LA, Kuettner KE, Galante JO. The potential role of fibroblasts in periprosthetic osteolysis: fibroblast response to titanium particles. J Bone Miner Res. 1995;10:1417–27.
Koreny T, Tunyogi-Csapó M, Gál I, Vermes C, Jacobs JJ, Glant TT. The role of fibroblasts and fibroblast-derived factors in periprosthetic osteolysis. Arthritis Rheum. 2006;54:3221–32.
Tunyogi-Csapo M, Koreny T, Vermes C, Galante JO, Jacobs JJ, Glant TT. Role of fibroblasts and fibroblast-derived growth factors in periprosthetic angiogenesis. J Orthop Res. 2007;25:1378–88.
Lochner K, Fritsche A, Jonitz A, Hansmann D, Mueller P, Mueller-Hilke B, Bader R. The potential role of human osteoblasts for periprosthetic osteolysis following exposure to wear particles. Int J Mol Med. 2011;28:1055–63.
Huss RS, Huddleston JI, Goodman SB, Butcher EC, Zabel BA. Synovial tissue-infiltrating natural killer cells in osteoarthritis and periprosthetic inflammation. Arthritis Rheum. 2010;62:3799–805.
Miller TT. Imaging of hip arthroplasty. Semin Musculoskelet Radiol. 2006;10:30–46.
Cahir JG, Toms AP, Marshall TJ, Wimhurst J, Nolan J. CT and MRI of hip arthroplasty. Clin Radiol. 2007;62:1163–71.
Fabbri N, Rustemi E, Masetti C, Kreshak J, Gambarotti M, Vanel D, Toni A, Mercuri M. Severe osteolysis and soft tissue mass around total hip arthroplasty: description of four cases and review of the literature with respect to clinico-radiographic and pathologic differential diagnosis. Eur J Radiol. 2011;77:43–50.
Bedair H, Ting N, Jacovides C, Saxena A, Moric M, Parvizi J, Della Valle CJ. The Mark Coventry award: diagnosis of early postoperative TKA infection using synovial fluid analysis. Clin Orthop Relat Res. 2011;469:34–40.
Buttaro MA, Tanoira I, Comba F, Piccaluga F. Combining C-reactive protein and interleukin-6 may be useful to detect periprosthetic hip infection. Clin Orthop Relat Res. 2010;468:3263–7.
Meermans G, Haddad FS. Is there a role for tissue biopsy in the diagnosis of periprosthetic infection? Clin Orthop Relat Res. 2010;468:1410–7.
Wirtz DC, Niethard FU. Etiology, diagnosis and therapy of aseptic hip prosthesis loosening: a status assessment. Z Orthop Ihre Grenzgeb. 1997;135:270–80.
Jaiswal A, Gilbert RE, Sunil Kumar KH, Carrothers AD, Kuiper JH, Richardson JB. Function and survival after revision of hip resurfacing. Hip Int. 2011;21:610–5.
Oussedik SI, Dodd MB, Haddad FS. Outcomes of revision total hip replacement for infection after grading according to a standard protocol. J Bone Joint Surg Br. 2010;92:1222–6.
Klouche S, Lhotellier L, Mamoudy P. Infected total hip arthroplasty treated by an irrigation-debridement/component retention protocol. A prospective study in a 12-case series with minimum 2 years’ follow-up. Orthop Traumatol Surg Res. 2011 Mar 7. Epub.
Sharma AK, Gioe TJ, Nelson TE. Two-stage exchange for infected resurfacing arthroplasty: use of a novel cement spacer technique. J Arthroplasty. 2011;26:976–8.
Engesæter LB, Dale H, Schrama JC, Hallan G, Lie SA. Surgical procedures in the treatment of 784 infected THAs reported to the Norwegian arthroplasty register. Acta Orthop. 2011;82:530–7.
Hofmann AA. Two-stage exchange is better than direct exchange in the infected THA. Orthopedics. 1999;22:918–22.
Gazsó I, Kránicz J, Bellyei Á, Lőrinczy D. DSC analysis of the abnormalities of human leg skeletal muscles. A preliminary study. Thermochimica Acta. 2003;402:117–22.
Sillinger T, Than P, Kocsis B, Lőrinczy D. Differential scanning calorimetric measurement of cartilage destruction caused by septic arthritis. J Thermal Anal Calorim. 2005;82:221–3.
Pintér C, Bognár G, Horváth B, Sydo T, Ligeti E, Pulai J, Lőrinczy D. DSC analysis of human fat tissue in idiopathic avascular necrosis of the femoral head– a preliminary study. J Thermal Anal Calorim. 2009;95:781–5.
Benkő L, Danis J, Hubmann R, Kasza G, Gömöri É, Rőth E, Lőrinczy D. DSC examination of the esophagus after implication of special stents, designed for the management of acute esophagus variceal bleeding. An experimental study. J Thermal Anal Calorim. 2009;95:763–8.
Bognár G, Szabó I, Pintér C, Ligeti E, Lőrinczy D. Changes in thermal denaturation properties of the long head of the biceps during lifetime. J Thermal Anal Calorim. 2010;102:65–8.
Wiegand N, Vámhidy L, Lőrinczy D. Differential scanning calorimetric examination of ruptured lower limb tendons in human. J Thermal Anal Calorim. 2010;101:487–92.
Sohár G, Pallagi E, Szabó-Révész P, Tóth K. New thermogravimetric protocol for the investigation of normal and damaged human hyaline cartilage. J Thermal Anal Calorim. 2007;89:853–6.
Tóth K, Sohár G, Aigner Z, Greksa F, Szabó-Révész P. Novel calorimetric properties of human cartilage samples in rheumatoid arthritis. J. Thermal Anal Calorim. 2009;5:813–5.
Tóth K, Sohár G, Pallagi E, Szabó-Révész P. Further characterization of degenerated human cartilage with differential scanning calorimetry. Thermochimica Acta. 2007;464:75–7.
Than P, Lőrinczy D. Differential scanning calorimetric examination of the osteoarthritic hyaline cartilage in rabbits. Thermochimica Acta. 2003;404:149–53.
Than P, Vermes C, Schäffer B, Lőrinczy D. Differential scanning calorimetric examination of the human hyaline cartilage: a preliminary study. Thermochimica Acta. 2000;346:147–51.
Acknowledgements
The SETARAM Micro DSC-II was purchased thanks to a grant (CO-272) from the Hungarian Scientific Research Fund (Dénes Lőrinczy).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Naumov, I., Lőrinczy, D., Vámhidy, L. et al. Differential scanning calorimetric examination of the interfacial membrane in failed hip joint replacements. J Therm Anal Calorim 109, 783–787 (2012). https://doi.org/10.1007/s10973-012-2254-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-012-2254-1