Abstract
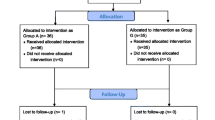
Although video laryngoscopy solves the problem of glottis exposure, it is difficult to deliver the tube to the glottic opening when the tracheal tube is unevenly shaped. This study aimed to compare the effects of different tube shapes on the first-pass success (FPS) rate in patients undergoing video laryngoscopy-assisted tracheal intubation. Three hundred patients above 18 years of age who underwent general anaesthesia and required endotracheal intubation were included in the study. The participants were randomly allocated to three groups with 100 participants in each group as follows: Group A, video laryngoscopes with a self-equipped stylet are used for tube preshaping; Group B: curvature of the video laryngoscope blade is modelled for tube preshaping; Group C: tube preshaping angle is consistent with the video laryngoscope blade, and the bending point is set 1 cm above the tracheal tube cuff. The primary outcome was FPS rates. The secondary outcomes included time to tracheal intubation, haemodynamic responses and adverse events. No significant differences in patient characteristics or airway assessments were noted (P > 0.05). Compared with Groups A, Group B and Group C exhibited a higher FPS rate (68% vs. 86% vs. 92%; P < 0.001). However, there is no significant difference in FPS rate between Group B and Group C (P > 0.05). And the time to tracheal intubation in Group C was significantly less than that in Group A and Group B (22.21 ± 4.01 vs. 19.92 ± 4.11 vs. 17.71 ± 3.47; P < 0.001). The straight-to-cuff stylet preshape angulation of curvature of the blade could provide a higher FPS rate and shorter time to tracheal intubation during video laryngoscopy-assisted endotracheal intubation. Trial registration: Chinese Clinical Trial Registry, ChiCTR1900026019.



Similar content being viewed by others
References
Mcnarry AF, Patel A. The evolution of airway management-new concepts and conflicts with traditional practice. Br J Anaesth. 2017;119:i154–66.
Mort TC, Braffett BH. Conventional versus video laryngoscopy for tracheal tube exchange: Glottic visualization, success rates, complications, and rescue alternatives in the high-risk difficult airway patient. Anesth Analg. 2015;121:440–8.
Lewis SR, Butler AR, Parker J, Cook TM, Schofield-Robinson OJ, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a Cochrane systematic review. Br J Anaesth. 2017;119:369–83.
Kerrey BT, Rinderknecht AS, Geis GL, Nigrovic LE, Mittiga MR. Rapid sequence intubation for pediatric emergency patients: higher frequency of failed attempts and adverse effects found by video review. Ann Emerg Med. 2012;60:259–61.
Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20:71–8.
Goto T, Gibo K, Hagiwara Y, Okubo M, Brown DF, Brown CA, Hasegawa K. Factors associated with first-pass success in pediatric intubation in the emergency department. West J Emerg Med. 2016;17:129–34.
Lascarrou JB, Boisrame-Helms J, Bailly A. Video laryngoscopy vs direct laryngoscopy on successful first-pass Orotracheal intubation among ICU patients: a randomized clinical trial. JAMA. 2017;317:483–93.
Gao YX, Song YB, Gu ZJ, Zhang JS, Chen CF, Sun H, Lu Z. Video versus direct laryngoscopy on successful first pass endotracheal intubation in ICU patients. World J Emerg Med. 2018;9:99–104.
Sulser S, Ubmann D, Schlaepfer M, Brueesch M, Goliasch G, Seifert B, Spahn DR, Ruetzler K. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: a randomised clinical trial. Eur J Anaesthesiol. 2016;33:943–8.
Jiang L, Qiu S, Zhang P, Yao W, Chang Y, Dai Z. The midline approach for endotracheal intubation using GlideScope video laryngoscopy could provide better glottis exposure in adults: a randomized controlled trial. BMC Anesthesiol. 2019;19:200.
Russell TM, Hormis A, Rotherham NHS Foundation Trust. Should the Glidescope video laryngoscope be used first line for all oral intubations or only in those with a difficult airway? A review of current literature. J Perioper Pract. 2018;28(12):322–33.
Hossfeld B, Frey K, Doerges V, Lampl L, Helm M. Improvement in glottic visualisation by using the C-MAC PM video laryngoscope as a first-line device for out-of-hospital emergency tracheal intubation: an observational study. Eur J Anaesthesiol. 2015;32(6):425–31.
Levitan RM, Heitz JW, Sweeney M, Cooper RM. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–7.
Maldini B, Hodžović I, Goranović T, Mesarić J. Challenges in the use of video laryngoscopes. Acta Clin Croat. 2016;55(Suppl 1):41–50.
Levitan RM, Pisaturo JT, Kinkle WC, Butler K, Everett WW. Stylet bend angles and tracheal tube passage using a straight-to-cuff shape. Acad Emerg Med. 2006;13:1255–8.
Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–8.
Park JW, Choi HJ. Study on the effect of a cold environment on the quality of three video laryngoscopes: McGrath MAC, GlideScope Ranger, and Pentax Airway Scope. Clin Exp Emerg Med. 2019;6:351–5.
Grape S, Schoettker P. The role of tracheal tube introducers and stylets in current airway management. J Clin Monit Comput. 2017;31:531–7.
Jones L, Mulcahy K, Fox J, Cook TM, Kelly FE. C-MAC© videolaryngoscopy: the anaesthetic assistant’s view. J Perioper Pract. 2018;28:83–9.
Wang Y, Wen C, Deng XM, Jin JH, Wang YH, Xu WL, Liu JH. Comparison of different stylet angulation and endotracheal tube camber on time to intubation with the Tosight. J Clin Anesthesiol. 2014;30:659–62.
Wang L, Sui JH, Deng XM, Xu WL, Chen KY, Wei LX, Yang D. Impacts of different nostril for nasotracheal intubation with video laryngoscopy. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2019;41:379–82.
Böttiger BW, Hinkelbein J. Comparison of different video laryngoscopes for emergency intubation in a standardized airway manikin with immobilized cervical spine by experienced anaesthetists: a randomized, controlled crossover trial. Resuscitation. 2012;83:740–5.
Ruetzler K, Imach S, Weiss M, Haas T, Schmidt AR. Comparison of five video laryngoscopes and conventional direct laryngoscopy. Anaesthesist. 2015;64:513–9.
Funding
This work was funded by the Research Foundation of Technology Bureau of Anhui Province, China Grant Nos. 201904a07020026, Zeping Dai, and 201904b11020014, Weidong Yao. The funding agent had no role in the study design, data collection, or data analyses.
Author information
Authors and Affiliations
Contributions
ZY and JLX collected the data. YWD and CY supervised the research and analysed the data. JLX and CY wrote and revised the manuscript. CYQ and DZP designed and conducted the study. All of the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of iInterest
All authors declare that they have no conflict of interest to disclose.
Ethical approval
The study was approved by the Ethical Issues Committee of the First Affiliated Hospital of Wannan Medical College, Anhui, China (Chairperson Prof Wu P) on March 6, 2019.
Informed consent
Written informed consent was obtained from all the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, Y., Jiang, L., Zhang, Y. et al. An optimal tracheal tube preshaping strategy for endotracheal intubation using video laryngoscopy: a randomized controlled trial. J Clin Monit Comput 36, 1629–1634 (2022). https://doi.org/10.1007/s10877-022-00806-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00806-4