Abstract
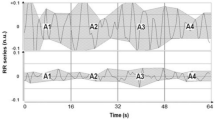
The assessment of the adequacy of general anesthesia for surgery, namely the nociception/anti-nociception balance, has received wide attention from the scientific community. Monitoring systems based on the frontal EEG/EMG, or autonomic state reactions (e.g. heart rate and blood pressure) have been developed aiming to objectively assess this balance. In this study a new multivariate indicator of patients’ steady-state during anesthesia (STAN) is proposed, based on wavelet analysis of signals linked to noxious activation. A clinical protocol was designed to analyze precise noxious stimuli (laryngoscopy/intubation, tetanic, and incision), under three different analgesic doses; patients were randomized to receive either remifentanil 2.0, 3.0 or 4.0 ng/ml. ECG, PPG, BP, BIS, EMG and \(\hbox {CO}_{2}\) were continuously recorded. ECG, PPG and BP were processed to extract beat-to-beat information, and \(\hbox {CO}_{2}\) curve used to estimate the respiration rate. A combined steady-state index based on wavelet analysis of these variables, was applied and compared between the three study groups and stimuli (Wilcoxon signed ranks, Kruskal–Wallis and Mann–Whitney tests). Following institutional approval and signing the informed consent thirty four patients were enrolled in this study (3 excluded due to signal loss during data collection). The BIS index of the EEG, frontal EMG, heart rate, BP, and PPG wave amplitude changed in response to different noxious stimuli. Laryngoscopy/intubation was the stimulus with the more pronounced response \((P<0.05)\). These variables were used in the construction of the combined index STAN; STAN responded adequately to noxious stimuli, with a more pronounced response to laryngoscopy/intubation (18.5–43.1 %, \(P<0.05\)), and the attenuation provided by the analgesic, detecting steady-state periods in the different physiological signals analyzed (approximately 50 % of the total study time). A new multivariate approach for the assessment of the patient steady-state during general anesthesia was developed. The proposed wavelet based multivariate index responds adequately to different noxious stimuli, and attenuation provided by the analgesic in a dose-dependent manner for each stimulus analyzed in this study.




Similar content being viewed by others
References
Monk TG, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after non-cardiac surgery. Anesth Analg. 2005;100(1):4–10.
Sessler DI, Sigl JC, Kelley SD, Chamoun NG, Manberg PJ, Saager L, Kurz A, Greenwald S. Hospital stay and mortality are increased in patients having a “triple low” of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia. J Am Soc Anesthesiol. 2012;116(6):1195–203.
Mashour GA. Neurophysiology and intraoperative nociception: new potentials? Anesthesiology. 2013;118(2):239.
Huiku M, Uutela K, van Gils M, Korhonen I, Kymlinen M, Merilinen P, Paloheimo M, Rantanen M, Takala P, Vierti-Oja H, Yli-Hankala A. Assessment of surgical stress during general anaesthesia. Br J Anaesth. 2007;98(4):447–55.
Paloheimo MPJ, Sahanne S, Uutela KH. Autonomic nervous system state: the effect of general anaesthesia and bilateral tonsillectomy after unilateral infiltration of lidocaine. Br J Anaesth. 2010;104(5):587–895.
Storm H. Skin conductance and the stress response from heel stick in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2000;83:143–7.
Barvais L, Engelman E, Eba JM, Coussaert E, Cantraine F, Kenny GN. Effect site concentrations of remifentanil and pupil response to noxious stimulation. Br J Anaesth. 2003;91(3):347–52.
Castro A, Amorim P, Nunes C, de Almeida F. Effect of propofol and remifentanil on a somatosensory evoked potential indicator of pain perception intensity in volunteers. J Clin Monit Comput. 2015;29(5):561–7. doi:10.1007/s10877-014-9632-0.
Greenwald SD, Rosow C. Bis and emg variability increase before somatic responses during surgery. Anesthesiology. 2006;105:1027.
Rehberg B, Ryll C, Hadzidiakos D, Dincklage FV, Baars JH. Variability comparison of the composite auditory evoked potential index and the bispectral index during propofol-fentanyl anesthesia. Technol Comput Simul. 2008;107(1):117–24.
Bennet HL, Patel L, Farida N, Beddell S, Bobbin M. Separation of the hypnotic component of anesthesia and facial emg responses to surgical stimulation. Anesthesiology. 2007;A730. http://www.asaabstracts.com/strands/asaabstracts/abstract.htm;jsessionid=A478F09D2699BD4D6172FD68AF622F61?year=2007&index=5&absnum=1737.
Rantanen M, Yli-Hankala A, Gils MV, Yppril-Wolters H, Takala P, Huiku M, Kymlinen M, Seitsonen E, Korhonen I. Novel multiparameter approach for measurement of nociception at skin incision during general anaesthesia. Br J Anaesth. 2006;96(3):367–76.
Cividjian A, Martinez J, Precloux ECP, Beraud AM, Rochette Y, Cler M, Bourdon L, Escarment J, Quintin L. Beat-by-beat cardiovascular index to predict unexpected intraoperative movement in anaesthetized unparalyzed patients: a retrospective analysis. J Clin Monit Comput. 2007;21(2):91–101.
Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, Youngs EJ. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82.
Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology. 1997;86:24–33.
Seshagiri CV, Rosow CE, Greenwald S. Bis(r) variability in response to skin incision was greater opposite to the side of surgery. Anesthesiology. 2007; 807.
Castro A, Amorim P, Nunes CS, Almeida FG. Development of a scale to assess noxious stimuli intensity during anesthesia and surgery using rasch analysis. J Neurosurg Anesthesiol. 2011;23(4):426–7.
Sörnmo L, Laguna P. Bioelectrical signal processing in cardiac and neurological applications. 1st ed. Amsterdam: Elsevier; 2005.
Cleveland WS, Devlin SJ. Locally weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc. 1988;83(403):596–610.
Jiang T, Chen B, He X, Stuart P. Application of steady-state detection method based on wavelet transform. Comput Chem Eng. 2003;27(4):569–78.
Szabó Z. Contour image data compression using spline wavelets. J Electr Eng. 2004;55(11–12):290–5.
Bahoura M, Hassani M, Hubin M. DSP implementation of wavelet transform for real time ECG wave forms detection and heart rate analysis. Comput Methods Progr Biomed. 1997;52(1):35–44.
Mallat S, Zhong S. Characterization of signals from multiscale edges. IEEE Trans Pattern Anal Mach Intell. 1992;14(7):710–32.
Zbinden AM, Petersen-Felix S, Thomson DA, Anaes FRC. Anesthetic depth defined using multiple noxious stimuli during isoflurane/oxygen anesthesia. II hemodynamic responses. Anesthesiology. 1994;80(2):261–7.
Zbinden AM, Peterson-Felix S, Thomson DA, Anaes FRC. Reduction by fentanyl of the cp50 values of propofol and hemodynamic responses to various noxious stimuli. Anesthesiology. 1997;87(2):213–27.
Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, Torri G. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg. 2005;101(1):125–30.
Jeanne M, Clément C, Jonckheere J, Tavernier Logier R B. Variations of the analgesia nociception index during general anaesthesia for laparoscopic abdominal surgery. J Clin Monit Comput. 2012;26(4):289–94. doi:10.1007/s10877-012-9354-0.
La Rovere MT, Pinna GD, Raczak G. Baroreflex sensitivity: Measurement and clinical implications. Ann Noninvasive Electrocardiol. 2008;13(2):191–207.
Karri S, Maheshwari A, Koch C, Duncan MXMA. Deeper level of anesthesia is associated with adverse neurological outcomes in cardiac surgical patients. Anesth Analg. 2009;108(SCA Supp):1–104.
Farag E, Chelune GJ, Schubert A, Mascha EJ. Deeper level of anesthesia is associated with adverse neurological outcomes in cardiac surgical patients. Anesth Analg. 2006;103(3):633–40.
Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral index monitoring to prevent awareness during anaesthesia: the b-aware randomised controlled trial. Lancet. 2004;363(9423):1757–63.
Ekman A, Lindholm ML, Lennmarken C, Sandin R. Reduction in the incidence of awareness using bis monitoring. Acta Anaesthesiol Scand. 2004;48(1):20–6.
Bouillon TW, Bruhn J, Radulescu L, Andresen C, Shafer TJ, Cohane C, Shafer SL. Pharmacodynamic interaction between propofol and remifentanil regarding hypnosis, tolerance of laryngoscopy, bispectral index, and electroencephalographic approximate entropy. Anesthesiology. 2004;100(6):1353–72.
Acknowledgments
The first author was supported by a scholarship from the Portuguese Foundation for Science and Technology (FCT SFRH/BD/35879/2007). The authors would also like to acknowledge the support of UISPA—System Integration and Process Automation Unit—Part of the LAETA (Associated Laboratory of Energy, Transports and Aeronautics) a I&D Unit of the Foundation for Science and Technology (FCT), Portugal. FCT support under project PEst-OE/EME/LA0022/2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Castro, A., de Almeida, F.G., Amorim, P. et al. A novel multivariate STeady-state index during general ANesthesia (STAN). J Clin Monit Comput 31, 851–860 (2017). https://doi.org/10.1007/s10877-016-9905-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9905-x