Abstract
Objective
Unexpected intraoperative movement may be detrimental during delicate surgery. This study tested retrospectively an algorithm based on beat-by-beat circulatory variables (incorporated into a Cardiovascular depth of anesthesia index: CARDEAN©) in relationship to unexpected movement, and compared its performance to that of the electroencephalogram (EEG)-derived index: BIS®-XP 4.0.
Methods
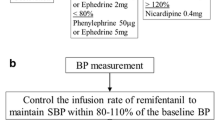
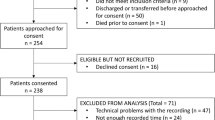
40 ASA I or II patients presenting for knee surgery had EEG (BIS® XP 4.0), beat-by-beat (Finapres®) finger non-invasive blood pressure (BP), conventional brachial BP and electrocardiogram (EKG) monitors attached. Anesthesia was induced and maintained with propofol and remifentanil. Before incision, the propofol concentration was set to maintain BIS <60. From incision to emergence, the anesthesiologist was denied access to BIS or Finapres. Anesthesia adjustment was titrated at the discretion of the anesthesiologist according to conventional signs only: brachial BP, EKG, eyelash reflex, movement. Occurrences of movement and eye signs (divergence of eyeballs, tears, corneal reflex, eyelash reflex) were observed. The CARDEAN algorithm was written retrospectively and tested vs. BIS.
Results
11 movements occurred in 8 patients. CARDEAN >60 predicted movement in 30% of the cases, 15 to 274 s before movement (sensitivity: 100%, specificity: 95%; relative operating curve ROC = 0.98; prediction probability pk = 0.98). BIS >60 predicted movement in 19% of cases (sensitivity: 64%; specificity: 94%, ROC: 0.85, pk: 0.85).
Conclusion
Retrospectively, a cardiovascular index predicted unexpected intraoperative movements. Prospective validation is needed.
Similar content being viewed by others
References
Antognini JF, Carstens E (2005) Measuring minimum alveolar concentration: more than meets the tail. Anesthesiology 103:679–680
Kearse LA, Manberg P, deBros F, Chamoun N, Sinai V (1994) Bispectral analysis of the electroencephalogram during induction of anesthesia may predict hemodynamic responses to laryngoscopy and intubation. Electroencephalogr Clin Neurophysiol 90:194–200
Sebel PS, Bowles SM, Saini V, Chamoun N (1995) EEG bispectrum predicts movement during thiopental/isoflurane anesthesia. J Clin Mon 11:83–91
Sebel PS, Lang E, Rampil IJ, White PF, Cork R, Jopling M, Smith NT, Glass PSA, Manberg P (1997) A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg 84:891–899
Johansen JW, Sebel PS (2000) Development and clinical application of electroencephalographic bispectrum monitoring. Anesthesiology 93:1336–1344
Myles PS, Leslie K, McNeil J, Forbes A, Chan MT (2004) Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 363:1757–1763
Ekman A, Lindholm ML, Lennmarken C, Sandin R (2004) Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol Scand 48:20–26
Monk TG, Saini V, Weldon C, Sigl JC: Anesthetic management and one-year mortality after non cardiac surgery. Anesth Analg 2005; 100: 4–10
Lennmarken C, Lindholm ML, Greenwald SD, Sandin R (2003) Confirmation that low intraoperative BIS levels predict increased risk of perioperative mortality. Anesthesiology 99 (Suppl):A303 (Abstract)
Pomfrett CJD, Barrie JR, Healy TEJ (1993) Respiratory sinus arrythmia: an index of light anesthesia. Brit J Anaesth 71:212–217
Korhonen I, Seitsonen E, van Gils M, Korttila K, Yli-Hankala A (2003) Heart Rate Variability Responses to Skin Incision in 0.8 MAC Sevoflurane anesthesia. IJBEM 5:240–241
Donchin Y, Feld JM, Porges SW (1985) Respiratory sinus arrhythmia during recovery from isoflurane-nitrous oxide anesthesia. Anesth Analg 64:811–815
Kalkman CJ, Drummond JC (2002) Monitors of depth of anesthesia: quo vadis? Anesthesiology 96:784–787
Marsh B, White M, Morton M, Kenny GNC (1991) Pharmacokinetic model driven infusion of propofol in children. Brit J Anaesth 67:41–48
Brice DD, Hetherington RR, Utting JE (1970) A simple study of awareness and dreaming during anesthesia. Brit J Anaesth 42:535–541
Struys MM, Jensen EW, Smith W, Smith NT, Rampil I, Dumortier FJ, Mestach C, Mortier EP (2002) Performance of the ARX-derived auditory evoked potential index as an indicator of anesthetic depth: a comparison with bispectral index and hemodynamic measures during propofol administration. Anesthesiology 96:803–816
Smith WD, Dutton RC, Smith NT (1996) Measuring the performance of anesthetic depth indicators. Anesthesiology 84:38–51
Pichot V, Buffière S, Gaspoz JM, Costes F, Molliex S, Duverney D, Roche F, Barthelemy JC (2001) Wavelet transform of heart rate variability to assess autonomic nervous activity does not predict arousal from general anesthesia. Can J Anaesth 48:859–863
Yli-Hankala A, Porkkala T, Kaukinen S, Hakkinen V, Jantti V (1991) Respiratory sinus arrhythmia is reversed during positive pressure ventilation. Acta Physiol Scand 141:399–407
Di Rienzo M, Bertinieri G, Mancia G, Pedotti A (1985) A new method for evaluating the baroreflex role by a joint pattern analysis of pulse interval and systolic blood pressure series. Med Biol Eng Comp 23 (suppl part I):313–314
Lafrenière G, Milne B, Brunet DG, Adams MA, Parlow JL (2000) Autonomic circulatory and cerebrocortical responses during increasing depth of propofol sedation/hypnosis in humans. Can J Anaesth 47:441–448
Parlow J, Viale JP, Annat G, Hughson RL, Quintin L (1995) Spontaneous cardiac baroreflex in humans: comparison with drug-induced responses. Hypertension 25:1058–1068
Bristow JD, Prys-Roberts C, Fisher A, Pickering TG (1969) Sleight P: Effects of anesthesia on baroreflex control of heart rate in man. Anesthesiology 31:422–428
Legramante JM, Raimondi G, Massaro M, Cassarino S, Peruzzi G, Iellamo F (1999) Investigating feed-forward neural regulation of circulation from analysis of spontaneous arterial pressure and heart rate fluctuations. Circulation 99:1760–1766
Hughson RL, Quintin L, Annat G, Yamamoto Y, Gharib C (1993) Spontaneous baroreflex by sequence and power spectral methods in humans. Clin Phys 13:663–676
Abrahams VC, Hilton SM, Zbrozyna A (1960) Active muscle vasodilatation produced by stimulation of the brain stem: its significance in the defence reaction. J Physiol (London) 154:491–513
Bandler R (1982) Induction of “rage” following microinjections of glutamate into midbrain but not hypothalamus of cats. Neurosci Lett 30:183–188
Kircheim HR (1976) Systemic arterial baroreceptor reflexes. Physiol Rev 56:100–176
Craig AD (2003) A new view of pain as a homeostatic emotion. Trends Neurosci 26:303–307
Rampil I, Matteo RS (1987) Changes in spectral edge frequency correlate with the hemodynamic response to laryngoscopy and intubation. Anesthesiology 67:139–142
Guignard B, Menigaux C, Dupont X, Fletcher D, Chauvin M (2000) The effect of remifentanil on the bispectral index change and hemodynamic responses after orotracheal intubation. Anesth Analg 90:161–167
White PF, Boyle WA (1989) Relationship between hemodynamic and electroencephalographic changes during general anesthesia. Anesth Analg 68:177–181
Ghouri AF, Monk TG, White PF (1993) Electroencephalogram spectral edge frequency, lower esophageal contractility and autonomic responsiveness during general anesthesia . J Clin Mon 9:176–185
Hung OR, Varvel JR, Shafer SL, Stanski DR (1992) Thiopental pharmacodynamics: II. quantitation of clinical and electroencephalographic depth of anesthesia. Anesthesiology 77:237–244
Raymondos K, Munte S, Krauss T, Grouven U, Piepenbrock S (2003) Cortical activity assessed by Narcotrend® in relation to haemodynamic responses to tracheal intubation at different stages of cortical suppression and reflex control. Eur J Anaesthesiol 19:1–8
Muthuswany J, Roy RJ (1999) The use of fuzzy integrals and bispectral analysis of the electroencephalogram to predict movement under anesthesia. IEEE Trans Biomed Eng 46:291–299
Leistritz L, Kochs E, Galicki M, Witte H (2002) Prediction of movement following noxious stimulation during 1 minum alveolar anesthetic concentration isoflurane/nitrous oxide anesthesia by means of midle latency auditory evoked responses. Clin Neurophysiol 113:930–935
Katoh T, Suzuki A, Ikeda K (1998) Electroencephalographic derivatives as a tool for predicting the depth of sedation and anesthesia induced by sevoflurane. Anesthesiology 88:642–650
Rodriguez RA, Hall LE, Duggan S, Splinter WM (2004) The bispectral index does not correlate with clinical signs of inhalational anesthesia during sevoflurane induction and arousal in children. Can J Anaesth 51:472–480
Author information
Authors and Affiliations
Corresponding author
Additional information
Cividjian A., Martinez J.Y., Combourieu E., Precloux P., Beraud A.M., Rochette Y.,Cler M., Bourdon L., Escarment J., Quintin L. Beat-by-beat cardiovascular index to predict unexpected intraoperative movement in anesthetized unparalyzed patients: a retrospective analysis.
Appendix
Appendix
Detailed description of the CARDEAN algorithm

Beat-by-beat R–R interval and SBP time-series were digitally filtered using a low-pass filter (cut-off = 0.1 Hz). Local minimums and maximums were detected. For each SBP rise higher than a threshold comprised between 2 and 5mmHg (e.g. hatched area) the following steps were performed. (a) The SBP rise time was calculated (time interval between the 2 opened circles). (b) The SBP area under the curve (AUC) was calculated with respect to the SBP value at the onset of the SBP rise (left opened circle). The AUC under the SBP curve was calculated over a period (ΔT) equal to 1.5 times the SBP rise time, with respect to the onset of the SBP rise. (c) The RR interval rise following the SBP rise was detected. (d) The R–R interval AUC was calculated with respect to the R–R interval value at the onset of the R–R interval rise (left opened circle). The AUC under the R–R interval curve, positive or negative, was calculated over a period of identical length (ΔT) as for the corresponding SBP rise, with respect to the onset of the R–R interval rise. The R–R interval curve between the 2 opened circles was named here R–R baroreflex response. (e) The R–R interval area to SBP area ratio (Area Ratio) was calculated (parameter p1). (f) The amplitude RR− of the R–R interval fall preceding the R–R baroreflex response was calculated (parameter p2). (g) The amplitude RR+ of the RR rise during the R–R baroreflex response was calculated. The parameter p3 = RR+/RR− was derived. (h) The parameter p4 was calculated as being the difference (ΔRR) between the RR value at the onset of the R–R baroreflex response (left opened circle) and the RR value at the end of the R–R baroreflex response (right opened circle). When (a) p1 was smaller than a threshold comprised between 1 and 3 and (b) p2 was greater than a threshold comprised between 40 and 80 and (c) p3 was smaller than a threshold comprised between 0.3 and 0.75 and (d) p4 was smaller than a threshold comprised between −20 and 10, CARDEAN index was set to a value greater than 60. This signs an “occluded” baroreflex response. If at least one of criteria 1–4 was not fulfilled, CARDEAN index was set to a value smaller that 60. This signs a normal baroreflex response. The precise value of thresholds were tuned retrospectively in order to achieve an acceptable fit between the CARDEAN index and the occurrence of movement.
Rights and permissions
About this article
Cite this article
Cividjian, A., Martinez, J.Y., Combourieu, E. et al. Beat-by-beat cardiovascular index to predict unexpected intraoperative movement in anesthetized unparalyzed patients: a retrospective analysis. J Clin Monit Comput 21, 91–101 (2007). https://doi.org/10.1007/s10877-006-9061-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-006-9061-9