Abstract
Currently, commercial synthetic vascular grafts made from Dacron and ePTFE for small-diameter, vascular applications (<6 mm) show limited reendothelization and are less compliant, often resulting in thrombosis and intimal hyperplasia. Although good blood compatibility can be achieved in autologous arteries and veins, the number of high quality harvest sites is limited, and the grafts are size-mismatched for use in the fistula or cardiovascular bypass surgery; thus, alternative small graft substitutes must be developed.
A biotube is an in vivo, tissue-engineered approach for the growth of autologous grafts through the subcutaneous implantation of an inert rod through the inflammation process. In the present study, we embedded silicone rods with a diameter of 2 mm into the dorsal subcutaneous tissue of rabbits for 4 weeks to grow biotubes. The formation of functional endothelium cells aligned on the inner wall surface was achieved by seeding with adipose stem cells (ADSCs). The ADSCs-seeded biotubes were implanted into the carotid artery of rabbits for more than 1 month, and the patency rates and remodeling of endothelial cells were observed by angiography and fluorescence staining, respectively. Finally, the mechanical properties of the biotube were also evaluated.
The fluorescence staining results showed that the ADSCs differentiated not only into endothelia cells but also into smooth muscle cells. Moreover, the patency of the ADSCs-seeded biotube remained high for at least 5 months. These small-sized ADSCs-seeded vascular biotubes may decrease the rate of intimal hyperplasia during longer implantation times and have potential clinical applications in the future.
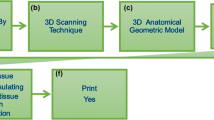
Graphical abstract





Similar content being viewed by others
References
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):480–6. https://doi.org/10.1161/CIRCULATIONAHA.108.191259.
United States Renal Data System. 2015 USRDS annual data report: Epidemiology of Kidney Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2015.
Wang X, Lin P, Yao Q, Chen C. Development of small-diameter vascular grafts. World J Surg. 2007;31(4):682–9. https://doi.org/10.1007/s00268-006-0731-z.
Enomoto S, Sumi M, Kajimoto K, Nakazawa Y, Takahashi R, Takabayashi C, et al. Long-term patency of small-diameter vascular graft made from fibroin, a silk-based biodegradable material. J Vasc Surg. 2010;51(1):155–64. https://doi.org/10.1016/j.jvs.2009.09.005.
Pawlowski KJ, Rittgers SE, Schmidt SP, Bowlin GL. Endothelial cell seeding of polymeric vascular grafts. Front Biosci. 2004;9:1412–21.
Abbott WM, Callow A, Moore W, Rutherford R, Veith F, Weinberg S. Evaluation and performance standards for arterial prostheses. J Vasc Surg. 1993;17(4):746–56.
Bennion RS, Williams RA, Stabile BE, Fox MA, Owens ML, Wilson SE. Patency of autogenous saphenous vein versus polytetrafluoroethylene grafts in femoropopliteal bypass for advanced ischemia of the extremity. Surg Gynecol Obstet. 1985;160(3):239–42.
Desmet W, Vanhaecke J, Vrolix M, Van de Werf F, Piessens J, Willems J, et al. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J. 1992;13(12):1637–40.
Seifu DG, Purnama A, Mequanint K, Mantovani D. Small-diameter vascular tissue engineering. Nat Rev Cardiol. 2013;10(7):410–21. https://doi.org/10.1038/nrcardio.2013.77.
Hsu S, Kambic H. On matching compliance between canine carotid arteries and polyurethane grafts. Artif Org. 1997;21(12):1247–54.
Fernandez CE, Achneck HE, Reichert WM, Truskey GA. Biological and engineering design considerations for vascular tissue engineered blood vessels (TEBVs). Curr Opin Chem Eng. 2014;3:83–90. https://doi.org/10.1016/j.coche.2013.12.001.
Dukkipati R, Peck M, Dhamija R, Hentschel DM, Reynolds T, Tammewar G, et al. Biological grafts for hemodialysis access: historical lessons, state-of-the-art and future directions. Semin Dial. 2013;26(2):233–9. https://doi.org/10.1111/j.1525-139X.2012.01106.x.
Daenens K, Schepers S, Fourneau I, Houthoofd S, Nevelsteen A. Heparin-bonded ePTFE grafts compared with vein grafts in femoropopliteal and femorocrural bypasses: 1- and 2-year results. J Vasc Surg. 2009;49(5):1210–6. https://doi.org/10.1016/j.jvs.2008.12.009.
Campbell JH, Efendy JL, Campbell GR. Novel vascular graft grown within recipient’s own peritoneal cavity. Circ Res. 1999;85(12):1173–8.
Huang H, Zhou YM, Ishibashi-Ueda H, Takamizawa K, Ando J, Kanda K, et al. In vitro maturation of “biotube” vascular grafts induced by a 2-day pulsatile flow loading. J Biomed Mater Res B Appl Biomater. 2009;91(1):320–8. https://doi.org/10.1002/jbm.b.31405.
Nakayama Y, Ishibashi-Ueda H, Takamizawa K. In vivo tissue-engineered small-caliber arterial graft prosthesis consisting of autologous tissue (biotube). Cell Transplant. 2004;13(4):439–49.
Ma N, Wang Z, Chen H, Sun Y, Hong H, Sun Q, et al. Development of the novel biotube inserting technique for acceleration of thick-walled autologous tissue-engineered vascular grafts fabrication. J Mater Sci Mater Med. 2011;22(4):1037–43. https://doi.org/10.1007/s10856-011-4257-z.
Watanabe T, Kanda K, Yamanami M, Ishibashi-Ueda H, Yaku H, Nakayama Y. Long-term animal implantation study of biotube-autologous small-caliber vascular graft fabricated by in-body tissue architecture. J Biomed Mater Res B Appl Biomater. 2011;98(1):120–6. https://doi.org/10.1002/jbm.b.31841.
Oie T, Yamanami M, Ishibashi-Ueda H, Kanda K, Yaku H, Nakayama Y. In-body optical stimulation formed connective tissue vascular grafts, “biotubes,” with many capillaries and elastic fibers. J Artif Organs. 2010;13(4):235–40. https://doi.org/10.1007/s10047-010-0517-9.
Sakai O, Kanda K, Takamizawa K, Sato T, Yaku H, Nakayama Y. Faster and stronger vascular “Biotube” graft fabrication in vivo using a novel nicotine-containing mold. J Biomed Mater Res B Appl Biomater. 2009;90(1):412–20. https://doi.org/10.1002/jbm.b.31300.
Nakayama Y, Tsujinaka T. Acceleration of robust “biotube” vascular graft fabrication by in-body tissue architecture technology using a novel eosin Y-releasing mold. J Biomed Mater Res B Appl Biomater. 2014;102(2):231–8. https://doi.org/10.1002/jbm.b.32999.
Wu HC, Wang TW, Kang PL, Tsuang YH, Sun JS, Lin FH. Coculture of endothelial and smooth muscle cells on a collagen membrane in the development of a small-diameter vascular graft. Biomaterials. 2007;28(7):1385–92. https://doi.org/10.1016/j.biomaterials.2006.11.012.
Berglund JD, Galis ZS. Designer blood vessels and therapeutic revascularization. Br J Pharmacol. 2003;140(4):627–36. https://doi.org/10.1038/sj.bjp.0705457.
Miranville A, Heeschen C, Sengenes C, Curat CA, Busse R, Bouloumie A. Improvement of postnatal neovascularization by human adipose tissue-derived stem cells. Circulation. 2004;110(3):349–55. https://doi.org/10.1161/01.CIR.0000135466.16823.D0.
Schaffler A, Buchler C. Concise review: adipose tissue-derived stromal cells--basic and clinical implications for novel cell-based therapies. Stem cells. 2007;25(4):818–27. https://doi.org/10.1634/stemcells.2006-0589.
DiMuzio P, Tulenko T. Tissue engineering applications to vascular bypass graft development: the use of adipose-derived stem cells. J Vasc Surg. 2007;45(Suppl A):A99–103. https://doi.org/10.1016/j.jvs.2007.02.046.
Yamanami M, Ishibashi-Ueda H, Yamamoto A, Iida H, Watanabe T, Kanda K, et al. Implantation study of small-caliber “biotube” vascular grafts in a rat model. J Artif Organs. 2013;16(1):59–65. https://doi.org/10.1007/s10047-012-0676-y.
Sarkar S, Salacinski HJ, Hamilton G, Seifalian AM. The mechanical properties of infrainguinal vascular bypass grafts: their role in influencing patency. Eur J Vasc Endovasc Surg. 2006;31(6):627–36. https://doi.org/10.1016/j.ejvs.2006.01.006.
Kaushal S, Amiel GE, Guleserian KJ, Shapira OM, Perry T, Sutherland FW, et al. Functional small-diameter neovessels created using endothelial progenitor cells expanded ex vivo. Nat Med. 2001;7(9):1035–40. https://doi.org/10.1038/nm0901-1035.
Niklason LE, Gao J, Abbott WM, Hirschi KK, Houser S, Marini R, et al. Functional arteries grown in vitro. Science. 1999;284(5413):489–93.
Hoerstrup SP, Cummings Mrcs I, Lachat M, Schoen FJ, Jenni R, Leschka S, et al. Functional growth in tissue-engineered living, vascular grafts: follow-up at 100 weeks in a large animal model. Circulation. 2006;114(1):I159–66. https://doi.org/10.1161/CIRCULATIONAHA.105.001172.
Zhao Y, Zhang S, Zhou J, Wang J, Zhen M, Liu Y, et al. The development of a tissue-engineered artery using decellularized scaffold and autologous ovine mesenchymal stem cells. Biomaterials. 2010;31(2):296–307. https://doi.org/10.1016/j.biomaterials.2009.09.049.
Roh JD, Sawh-Martinez R, Brennan MP, Jay SM, Devine L, Rao DA, et al. Tissue-engineered vascular grafts transform into mature blood vessels via an inflammation-mediated process of vascular remodeling. Proc Natl Acad Sci USA. 2010;107(10):4669–74. https://doi.org/10.1073/pnas.0911465107.
Mirensky TL, Nelson GN, Brennan MP, Roh JD, Hibino N, Yi T, et al. Tissue-engineered arterial grafts: long-term results after implantation in a small animal model. J Pediatr Surg. 2009;44(6):1127–32. https://doi.org/10.1016/j.jpedsurg.2009.02.035.
Cho SW, Lim SH, Kim IK, Hong YS, Kim SS, Yoo KJ, et al. Small-diameter blood vessels engineered with bone marrow-derived cells. Ann Surg. 2005;241(3):506–15.
Rosenman JE, Kempczinski RF, Pearce WH, Silberstein EB. Kinetics of endothelial cell seeding. J Vasc Surg. 1985;2(6):778–84.
Neff LP, Tillman BW, Yazdani SK, Machingal MA, Yoo JJ, Soker S, et al. Vascular smooth muscle enhances functionality of tissue-engineered blood vessels in vivo. J Vasc Surg. 2011;53(2):426–34. https://doi.org/10.1016/j.jvs.2010.07.054.
Krawiec JT, Vorp DA. Adult stem cell-based tissue engineered blood vessels: a review. Biomaterials. 2012;33(12):3388–400. https://doi.org/10.1016/j.biomaterials.2012.01.014..
Huang HS. Current advances of stem cell-based approaches to tissue-engineered vascular grafts. OA Tissue Eng. 2013;1(1):2.
Furukoshi M, Moriwaki T, Nakayama Y. Development of an in vivo tissue-engineered vascular graft with designed wall thickness (biotube type C) based on a novel caged mold. J Artif Organs. 2015. https://doi.org/10.1007/s10047-015-0859-4.
Watanabe T, Kanda K, Ishibashi-Ueda H, Yaku H, Nakayama Y. Autologous small-caliber “biotube” vascular grafts with argatroban loading: a histomorphological examination after implantation to rabbits. J Biomed Mater Res B Appl Biomater. 2010;92(1):236–42. https://doi.org/10.1002/jbm.b.31510.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Tseng, Y., Roan, J., Ho, Y. et al. An in vivo study on endothelialized vascular grafts produced by autologous biotubes and adipose stem cells (ADSCs). J Mater Sci: Mater Med 28, 166 (2017). https://doi.org/10.1007/s10856-017-5986-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-017-5986-4