Abstract
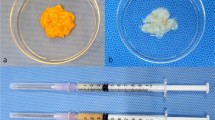
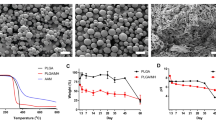
Biomaterials are often added to autologous fat grafts both as supporting matrices for the grafted adipocytes and as cell carrier for adipose-derived stem cells (ADSCs). This in vivo study used an autologous fat graft model to test a lamininalginate biomaterial, adipocytes, and ADSCs in immune-competent rats. We transplanted different combinations of shredded autologous adipose tissue [designated “A” for adipose tissue]), laminin-alginate beads [designated “B” for bead], and ADSCs [designated “C” for cell]) into the backs of 15 Sprague-Dawley rats. Group A received only adipocytes, Group B received only laminin-alginate beads, Group AB received adipocytes mixed with laminin-alginate beads, Group BC received laminin-alginate beads encapsulating ADSCs, and Group ABC received adipocytes and laminin-alginate beads containing ADSCs. Seven-tesla magnetic resonance imaging was used to evaluate the rats at the 1st, 6th, and 12th weeks after transplantation. At the 12th week, the rats were sacrificed and the implanted materials were retrieved for gross examination and histological evaluation. The results based on MRI, gross evaluation, and histological data all showed that implants in Group ABC had better resorption of the biomaterial, improved survival of the grafted adipocytes, and adipogenic differentiation of ADSCs. Volume retention of grafts in Group ABC (89%) was also significantly greater than those in Group A (58%) (p < 0.01). Our findings support that the combination of shredded adipose tissue with ADSCs in laminin-alginate beads provided the best overall outcome.





Similar content being viewed by others
References
Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001;28:111–9.
Bircoll M. Cosmetic breast augmentation utilizing autologous fat and liposuction techniques. Plast Reconstr Surg. 1987;79:267–71.
Claro F Jr, Figueiredo JC, Zampar AG, Pinto-Neto AM. Applicability and safety of autologous fat for reconstruction of the breast. Br J Surg. 2012;99(6):768–80.
Lu F, Li J, Gao J, et al. Improvement of the survival of human autologous fat transplantation by using VEGF-transfected adipose-derived stem cells. Plast Reconstr Surg. 2009;124:1437–46.
Hong SJ, Lee JH, Hong SM, Park CH. Enhancing the viability of fat grafts using new transfer medium containing insulin and fibroblast growth factor in autologous fat transplantation. J Plast Reconstr Aesthet Surg. 2010;63:1202–08.
Mackay DR, Manders EK, Saggers GC, Schenden MJ, Zaino R. The fate of dermal and dermal-fat grafts. Ann Plast Surg. 1993;31:42–6.
Kim HY, Jung BK, Lew DH, Lee DW. Autologous fat graft in the reconstructed breast: fat absorption rate and safety based on sonographic identification. Arch Plast Surg. 2014;41(6):740–7.
Mineda K, Kuno S, Kato H, Kinoshita K, Doi K, Hashimoto I, et al. Chronic inflammation and progressive calcification as a result of fat necrosis: the worst outcome in fat grafting. Plast Reconstr Surg. 2014;133(5):1064–72.
Kirkham JC, Lee JH, Medina MA 3rd, McCormack MC, Randolph MA, Austen WG Jr. The impact of liposuction cannula size on adipocyte viability. Ann Plast Surg. 2012;69(4):479–81.
Gause TM, Kling RE, Sivak WN, Marra KG, Rubin JP, Kokai LE. Particle size in fat graft retention: a review on the impact of harvesting technique in lipofilling surgical outcomes. Adipocyte. 2014;3(4):273–9.
Pu LL. Towards more rationalized approach to autologous fat grafting. J Plast Reconstr Aesthet Surg. 2012;65(4):413–9.
Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble JM. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy. 2013;15(6):641–8.
Minteer DM, Marra KG, Rubin JP. Adipose stem cells: biology, safety, regulation, and regenerative potential. Clin Plast Surg. 2015;42(2):169–79.
Pill K, Hofmann S, Redl H, Holnthoner W. Vascularization mediated by mesenchymal stem cells from bone marrow and adipose tissue: a comparison. Cell Regen (Lond). 2015;4:8
Matsumoto D, Sato K, Gonda K, Takaki Y, Shigeura T, Sato T, Aiba-Kojima E, Iizuka F, Inoue K, Suga H, Yoshimura K. Cell-assisted lipotransfer: supportive use of human adipose-derived cells for soft tissue augmentation with lipoinjection. Tissue Eng. 2006;12(12):3375–82.
Toyserkani NM, Quaade ML, Sørensen JA. Cell-assisted lipotransfer: a systematic review of its efficacy. Aesthet Plast Surg. 2016;40(2):309–18.
Feisst V, Meidinger S, Locke MB. From bench to bedside: use of human adipose-derived stem cells. Stem Cells Cloning. 2015;8:149–62.
Anderson SB, Lin CC, Kuntzler DV, Anseth KS. The performance of human mesenchymal stem cells encapsulated in cell-degradable polymer-peptide hydrogels. Biomaterials. 2011;32(14):3564–74.
Brännmark C, Paul A, Ribeiro D, Magnusson B, Brolén G, Enejder A, Forslöw A. Increased adipogenesis of human adipose-derived stem cells on polycaprolactone fiber matrices. PLoS One. 2014;9(11):e113620.
Catalán V, Gómez-Ambrosi J, Rodríguez A, Frühbeck G. Role of extracellular matrix remodelling in adipose tissue pathophysiology: relevance in the development of obesity. Histol Histopathol. 2012;27(12):1515–28.
Mori S, Kiuchi S, Ouchi A, Hase T, Murase T. Characteristic expression of extracellular matrix in subcutaneous adipose tissue development and adipogenesis; comparison with visceral adipose tissue. Int J Biol Sci. 2014;10(8):825–33.
Bhat A, Hoch AI, Decaris ML, Leach JK. Alginate hydrogels containing cell-interactive beads for bone formation. FASEB J. 2013;27(12):4844–52.
Glicklis R, Shapiro L, Agbaria R, Merchuk JC, Cohen S. Hepatocyte behavior within three-dimensional porous alginate scaffolds. Biotechnol Bioeng. 2005;67(3):344–53.
Miner JH. Laminins and their roles in mammals. Microsc Res Tech. 2008;71(5):349–56.
Williams SK, Kleinert LB, Patula-Steinbrenner V. Accelerated neovascularization and endothelialization of vascular grafts promoted by covalently bound laminin type 1. J Biomed Mater Res A. 2011;99(1):67–73.
Stamati K, Priestley JV, Mudera V, Cheema U. Laminin promotes vascular network formation in 3D in vitro collagen scaffolds by regulating VEGF uptake. Exp Cell Res. 2014;327(1):68–77.
Chen YS, Chen YY, Hsueh YS, Tai HC, Lin FH. Modifying alginate with early embryonic extracellular matrix, laminin and hyaluronic acid for adipose tissue engineering. J Biomed Mater Res A. 2015;104(3):669–77. doi:10.1002/jbm.a.35606.
Zuk PA, Zhu M, Ashjian P, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13:4279–95.
Dosier CR, Erdman CP, Park JH, Schwartz Z, Boyan BD, Guldberg RE. Resveratrol effect on osteogenic differentiation of rat and human adipose derived stem cells in a 3-D culture environment. J Mech Behav Biomed Mater. 2011;11:112–22.
Yushkevich PA, Piven J, Hazlett HC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31:1116–28.
Khouri RK, Rigotti G, Cardoso E, Khouri RK Jr, Biggs TM. Megavolume autologous fat transfer: part I. Theory and principles. Plast Reconstr Surg. 2014;133(3):550–7.
Moulonguet I, de Goursac C, Plantier F. Granulomatous reaction after injection of a new resorbable filler Novabel. Am J Dermatopathol. 2011;33:710–1.
Orive G, Hernández RM, Gascón AR, et al. Cell encapsulation: promise and progress. Nat Med. 2003;9:104–7.
Lawson MA, Barralet JE, Wang L, Shelton RM, Triffitt JT. Adhesion and growth of bone marrow stromal cells on modified alginate hydrogels. Tissue Eng. 2004;10:1480–91.
Smetana K Jr. Cell biology of hydrogels. Biomaterials. 1993;14:1046–50.
Hohenester E, Tisi D, Talts JF, Timpl R. The crystal structure of a laminin G-like module reveals the molecular basis of alpha-dystroglycan binding to laminins, perlecan, and agrin. Mol Cell. 1999;4:783–92.
Kang SW, Cha BH, Park H, Park KS, Lee KY, Lee SH. The effect of conjugating RGD into 3D alginate hydrogels on adipogenic differentiation of human adipose-derived stromal cells. Macromol Biosci. 2011;11(5):673–9.
Chandler EM, Berglund CM, Lee JS, Polacheck WJ, Gleghorn JP, Kirby BJ, et al. Stiffness of photocrosslinked RGD-alginate gels regulates adipose progenitor cell behavior. Biotechnol Bioeng. 2011;108(7):1683–92.
Schuller-Petrović S, Pavlović MD, Schuller SS, Schuller-Lukić B, Neuhold N. Early granulomatous foreign body reactions to a novel alginate dermal filler: the system’s failure? J Eur Acad Dermatol Venereol. 2013;27(1):121–3.
Andre P, Moulonguet I. Alginate (novabel): a new class of injectable filler. Facial Plast Surg. 2014;30(6):644–6.
Coppack SW, Pinkney JH, Mohamed-Ali V. Leptin production in human adipose tissue. Proc Nutr Soc. 1998;57:461–70.
Mohamed-Ali V, Pinkney JH, Coppack SW. Adipose tissue as an endocrine and paracrine organ. Int J Obes Relat Metab Disord. 1998;22:1145–58.
Deng Y, Scherer PE. Adipokines as novel biomarkers and regulators of the metabolic syndrome. Ann N Y Acad Sci. 2010;1212:E1–19.
Stillaert F, Findlay M, Palmer J, et al. Host rather than graft origin of Matrigel-induced adipose tissue in the murine tissue-engineering chamber. Tissue Eng. 2007;13:2291–300.
Wu L, Wang T, Ge Y, Cai X, Wang J, Lin Y. Secreted factors from adipose tissue increase adipogenic differentiation of mesenchymal stem cells. Cell Prolif. 2012;45:311–9.
Acknowledgments
We thank Dr. Ya-Hui Tsai and Hsiao-Fang Wei for technical and statistic assistance. We also thank the 7T Animal MRI Core Lab of the Neurobiology and Cognitive Science Center, National Taiwan University for their technical support.
Funding
The experiments in this study were partially funded by Far Eastern Memorial Hospital (FEMH-2012-C-004). No other funding was received.
Author contributions
Y-S C: First author, partially financed the study and carried out the project. Y-SH: Provided instruction for creating the laminin-alginate beads. Y-YC: Original author of the methods for creating the laminin-alginate biomaterial. C-YL: Pathologist, provided support for histological staining and reading. H-CT: Adviser regarding the medical aspects of this study. F-HL: Professor at the Institute of Biomedical Engineering and project director.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Presented at the 13th annual meeting of the International Federation for Adipose Therapeutics and Science (IFATS), New Orleans, Louisiana, USA, 2015. Title: Evaluation of biomaterial, adipocytes, and ADSC interaction in pure autologous fat grafting model through 7-TMRI.
Rights and permissions
About this article
Cite this article
Chen, YS., Hsueh, YS., Chen, YY. et al. Evaluation of a laminin-alginate biomaterial, adipocytes, and adipocyte-derived stem cells interaction in animal autologous fat grafting model using 7-Tesla magnetic resonance imaging. J Mater Sci: Mater Med 28, 18 (2017). https://doi.org/10.1007/s10856-016-5826-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5826-y