Abstract
BACKGROUND:
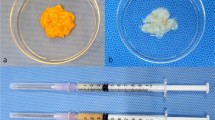
Autologous fat grafting is one of the most common procedures used in plastic surgery to correct soft tissue deficiency or depression deformity. However, its clinical outcomes are often suboptimal, and lack of metabolic and architectural support at recipient sites affect fat survival leading to complications such as cyst formation, calcification. Extracellular matrix-based scaffolds, such as allograft adipose matrix (AAM) and poly(lactic-co-glycolic) acid (PLGA), have shown exceptional clinical promise as regenerative scaffolds. Magnesium hydroxide (MH), an alkaline ceramic, has attracted attention as a potential additive to improve biocompatibility. We attempted to combine fat graft with regenerative scaffolds and analyzed the changes and viability of injected fat graft in relation to the effects of injectable natural, and synthetic (PLGA/MH microsphere) biomaterials.
METHODS:
In vitro cell cytotoxicity, angiogenesis of the scaffolds, and wound healing were evaluated using human dermal fibroblast cells. Subcutaneous soft-tissue integration of harvested fat tissue was investigated in vivo in nude mouse with random fat transfer protocol Fat integrity and angiogenesis were identified by qRT-PCR and immunohistochemistry.
RESULTS:
In vitro cell cytotoxicity was not observed both in AAM and PLGA/MH with human dermal fibroblast. PLGA/MH and AAM showed excellent wound healing effect. In vivo, the AAM and PLGA/MH retained volume compared to that in the only fat group. And the PLGA/MH showed the highest angiogenesis and anti-inflammation.
CONCLUSION:
In this study, a comparison of the volume retention effect and angiogenic ability between autologous fat grafting, injectable natural, and synthetic biomaterials will provide a reasonable basis for fat grafting.






Similar content being viewed by others
References
Li FW, Zeng L, Luo SK. Microenvironmental changes in the surviving fat 1 year after autologous fat transplantation for breast augmentation. Aesthet Surg J. 2021;41:NP127–33.
Yoshimura K, Sato K, Aoi N, Kurita M, Hirohi T, Harii K. Cell-assisted lipotransfer for cosmetic breast augmentation: supportive use of adipose-derived stem/stromal cells. Aesthetic Plast Surg. 2008;32:48–55.
Nalbach L, Müller D, Wrublewsky S, Metzger W, Menger MD, Laschke MW, et al. Microvascular fragment spheroids: Three-dimensional vascularization units for tissue engineering and regeneration. J Tissue Eng. 2021;12:20417314211035593.
Shoshani O, Shupak A, Ullmann Y, Ramon Y, Gilhar A, Kehat I, et al. The effect of hyperbaric oxygenation on the viability of human fat injected into nude mice. Plast Reconstr Surg. 2000;106:1390–6.
Choi JH, Gimble JM, Lee K, Marra KG, Rubin JP, Yoo JJ, et al. Adipose tissue engineering for soft tissue regeneration. Tissue Eng Part B Rev. 2010;16:413–26.
Kokai LE, Sivak WN, Schilling BK, Karunamurthy A, Egro FM, Schusterman MA, et al. Clinical evaluation of an off-the-shelf allogeneic adipose matrix for soft tissue reconstruction. Plast Reconstr Surg Global Open. 2020;8:e2574.
Flynn LE. The use of decellularized adipose tissue to provide an inductive microenvironment for the adipogenic differentiation of human adipose-derived stem cells. Biomaterials. 2010;31:4715–24.
Giatsidis G, Succar J, Waters TD, Liu W, Rhodius P, Wang C, et al. Tissue-engineered soft-tissue reconstruction using noninvasive mechanical preconditioning and a shelf-ready allograft adipose matrix. Plast Reconstr Surg. 2019;144:884–95.
Gold MH, Andriessen A, Day D, Dayan SH, Fabi SG, Goldberg DJ, et al. The role of a shelf-ready, human-derived, soft tissue injectable adipose matrix for facial volume correction. J Cosmet Dermatol. 2020;19:2476–83.
Han TT, Toutounji S, Amsden BG, Flynn LE. Adipose-derived stromal cells mediate in vivo adipogenesis, angiogenesis and inflammation in decellularized adipose tissue bioscaffolds. Biomaterials. 2015;72:125–37.
Baek SW, Song DH, Lee HI, Kim DS, Heo Y, Kim JH, et al. Poly(L-Lactic Acid) composite with surface-modified magnesium hydroxide nanoparticles by biodegradable oligomer for augmented mechanical and biological properties. Materials (Basel). 2021;14:5869.
Dharmayanti C, Gillam TA, Williams DB, Blencowe A. Drug-eluting biodegradable implants for the sustained release of bisphosphonates. Polymers (Basel). 2020;12:2930.
Kim DS, Lee JK, Jung JW, Baek SW, Kim JH, Heo Y, et al. Promotion of bone regeneration using bioinspired PLGA/MH/ECM scaffold combined with bioactive PDRN. Materials (Basel). 2021;14:4149.
Kupikowska-Stobba B, Lewińska D. Polymer microcapsules and microbeads as cell carriers for in vivo biomedical applications. Biomater Sci. 2020;8:1536–74.
Lee HI, Heo Y, Baek SW, Kim DS, Song DH, Han DK. Multifunctional biodegradable vascular PLLA scaffold with improved X-ray opacity, anti-inflammation, and re-endothelization. Polymers (Basel). 2021;13:1979.
Shin EY, Kim DS, Lee MJ, Lee AR, Shim SH, Baek SW, et al. Prevention of chemotherapy-induced premature ovarian insufficiency in mice by scaffold-based local delivery of human embryonic stem cell-derived mesenchymal progenitor cells. Stem Cell Res Ther. 2021;12:431.
Ko KW, Choi B, Kang EY, Shin SW, Baek SW, Han DK. The antagonistic effect of magnesium hydroxide particles on vascular endothelial activation induced by acidic PLGA degradation products. Biomater Sci. 2021;9:892–907.
Lih E, Kum CH, Park W, Chun SY, Cho Y, Joung YK, et al. Modified magnesium hydroxide nanoparticles inhibit the inflammatory response to biodegradable Poly(lactide- co-glycolide) implants. ACS Nano. 2018;12:6917–25.
Park JH, Kwon DY, Heo JY, Park SH, Park JY, Lee B, et al. Effect of drug carrier melting points on drug release of dexamethasone-loaded microspheres. Tissue Eng Regen Med. 2017;14:743–53.
Bedair TM, Lee CK, Kim DS, Baek SW, Bedair HM, Joshi HP, et al. Magnesium hydroxide-incorporated PLGA composite attenuates inflammation and promotes BMP2-induced bone formation in spinal fusion. J Tissue Eng. 2020;11:2041731420967591.
Lih E, Park W, Park KW, Chun SY, Kim H, Joung YK, et al. A Bioinspired scaffold with anti-inflammatory magnesium hydroxide and decellularized extracellular matrix for renal tissue regeneration. ACS Cent Sci. 2019;5:458–67.
Kang EY, Park SB, Choi B, Baek SW, Ko KW, Rhim WK, et al. Enhanced mechanical and biological characteristics of PLLA composites through surface grafting of oligolactide on magnesium hydroxide nanoparticles. Biomater Sci. 2020;8:2018–30.
Zhang S, Lu Q, Cao T, Toh WS. Adipose tissue and extracellular matrix development by injectable decellularized adipose matrix loaded with basic fibroblast growth factor. Plast Reconstr Surg. 2016;137:1171–80.
Peticone C, Thompson DS, Dimov N, Jevans B, Glass N, Micheletti M, et al. Characterisation of osteogenic and vascular responses of hMSCs to Ti-Co doped phosphate glass microspheres using a microfluidic perfusion platform. J Tissue Eng. 2020;11:2041731420954712.
Wong YH, Tan HY, Kasbollah A, Abdullah BJJ, Yeong CH. Preparation and in vitro evaluation of neutron-activated, theranostic samarium-153-labeled microspheres for transarterial radioembolization of hepatocellular carcinoma and liver metastasis. Pharmaceutics. 2019;11:596.
Shin SW, Jang YD, Ko KW, Kang EY, Han JH, Bedair TM, et al. PCL microspheres containing magnesium hydroxide for dermal filler with enhanced physicochemical and biological performances. J Ind Eng Chem. 2019;80:854–61.
Eto H, Kato H, Suga H, Aoi N, Doi K, Kuno S, et al. The fate of adipocytes after nonvascularized fat grafting: evidence of early death and replacement of adipocytes. Plast Reconstr Surg. 2012;129:1081–92.
Suga H, Eto H, Aoi N, Kato H, Araki J, Doi K, et al. Adipose tissue remodeling under ischemia: death of adipocytes and activation of stem/progenitor cells. Plast Reconstr Surg. 2010;126:1911–23.
Kokai LE, Schilling BK, Chnari E, Huang YC, Imming EA, Karunamurthy A, et al. Injectable allograft adipose matrix supports adipogenic tissue remodeling in the nude mouse and human. Plast Reconstr Surg. 2019;143:299e–309.
Nguyen MTN, Tran HLB. Fabrication of an injectable acellular adipose matrix for soft tissue regeneration. J Sci Adv Mater Dev. 2021;6:1–10.
Acknowledgements
This work was supported by Basic Science Research Program (2020R1A2B5B03002344) and Bio & Medical Technology Development Program (2018M3A9E2024579) through the National Research Foundation of Korea funded by the Ministry of Science and ICT (MSIT) and the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (202011A05-05), Republic of Korea. DKH, EH, and JCL conceived and supervised the project. The manuscript was written by DHK and DSK. The animal study was conducted by DHK, HJH, and SHB. JW Jung and SWB fabricated and analyzed characteristics of the scaffolds. JWJ and THK performed the experiments and analyzed the data. All authors have read and agreed to the published version of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
The study was performed after approval by the CHA University Bundang CHA Medical Center Internal Review Board (CHAMC 2020-03-013-003) and carried out following the guidelines for animal experimentation of the Animal Institutional Review Board of CHA University CHA Bundang Medical Center (IACUC 200074).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, DH., Kim, DS., Ha, HJ. et al. Fat Graft with Allograft Adipose Matrix and Magnesium Hydroxide-Incorporated PLGA Microspheres for Effective Soft Tissue Reconstruction. Tissue Eng Regen Med 19, 553–563 (2022). https://doi.org/10.1007/s13770-021-00426-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-021-00426-0