Abstract
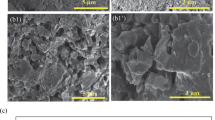
In a new approach combining additive manufacturing with bioceramics, a metallic 3D porous structure coated with bioactive glass was produced for possible use in orthopedic implants. This approach aims to combine high mechanical properties of the metallic structure with enhanced biological activity. 316L stainless steel (316L-SS) lattice structures were fabricated using selective laser melting. Despite its good mechanical properties, 316L-SS lacks the biofunctionality required to achieve long-term implantation. To be successfully used as biomaterial, these porous 3D lattice structures were thus coated by 58S bioglass through a simple impregnation method. The use of a silica layer was evaluated as possible pretreatment to improve bioglass adhesion. The coated parts are then assessed by scanning electron microscopy coupled with energy-dispersive spectrometry to qualify the coating. Porous sample parts pretreated with a silica layer presented a denser coating structure when compared with untreated porous metallic structures. The bioactivity in SBF medium shows the formation of a uniform apatite layer after 7 days of immersion, producing the bioregeneration capability. This latter, combined with the lightweight framework structure provided by 316-SS, will increase the lifetime of this new generation of orthopedic implants.








Similar content being viewed by others
References
Smith MC, Ben-Shlomo Y, Dieppe P, et al (2017) Rates of hip and knee joint replacement amongst different ethnic groups in England: an analysis of National Joint Registry data. Osteoarthr Cartil 25:448–454. https://doi.org/10.1016/j.joca.2016.12.030
Culliford D, Maskell J, Judge A et al (2015) Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research datalink. Osteoarthr Cartil 23:594–600. https://doi.org/10.1016/j.joca.2014.12.022
Lübbeke A, Silman AJ, Barea C et al (2018) Mapping existing hip and knee replacement registries in Europe. Health Policy (N Y) 122:548–557. https://doi.org/10.1016/j.healthpol.2018.03.010
Kurtz S, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Ser A 89:780–785. https://doi.org/10.2106/JBJS.F.00222
Ginebra M-P, Espanol M, Maazouz Y et al (2018) Bioceramics and bone healing. EFORT Open Rev 3:173–183. https://doi.org/10.1302/2058-5241.3.170056
Strumza E, Yeheskel O, Hayun S (2019) The effect of texture on the anisotropy of thermophysical properties of additively manufactured AlSi10Mg. Addit Manuf 29:100762. https://doi.org/10.1016/j.addma.2019.06.013
Gumbleton R, Cuenca JA, Klemencic GM et al (2019) Evaluating the coefficient of thermal expansion of additive manufactured AlSi10Mg using microwave techniques. Addit Manuf 30:100841. https://doi.org/10.1016/j.addma.2019.100841
Gao C, Peng S, Feng P, Shuai C (2017) Bone biomaterials and interactions with stem cells. Bone Res 5:1–33. https://doi.org/10.1038/boneres.2017.59
Yan Q, Dong H, Su J et al (2018) A review of 3D printing technology for medical applications. Engineering 4:729–742. https://doi.org/10.1016/j.eng.2018.07.021
Zadpoor AA, Malda J (2017) Additive manufacturing of biomaterials, tissues, and organs. Ann Biomed Eng 45:1–11. https://doi.org/10.1007/s10439-016-1719-y
Liu F, Mao Z, Zhang P et al (2018) Functionally graded porous scaffolds in multiple patterns: new design method, physical and mechanical properties. Mater Des 160:849–860. https://doi.org/10.1016/j.matdes.2018.09.053
Ibrahim MZ, Sarhan AAD, Yusuf F, Hamdi M (2017) Biomedical materials and techniques to improve the tribological, mechanical and biomedical properties of orthopedic implants—a review article. J Alloys Compd. https://doi.org/10.1016/j.jallcom.2017.04.231
Mahmoud D, Elbestawi M (2017) Lattice structures and functionally graded materials applications in additive manufacturing of orthopedic implants: a review. J Manuf Mater Process 1:13. https://doi.org/10.3390/jmmp1020013
Harrysson OLA, Cansizoglu O, Marcellin-Little DJ et al (2008) Direct metal fabrication of titanium implants with tailored materials and mechanical properties using electron beam melting technology. Mater Sci Eng C 28:366–373. https://doi.org/10.1016/j.msec.2007.04.022
Murr LE, Gaytan SM, Martinez E et al (2012) Next generation orthopaedic implants by additive manufacturing using electron beam melting. Int J Biomater. https://doi.org/10.1155/2012/245727
Yuan L, Ding S, Wen C (2019) Additive manufacturing technology for porous metal implant applications and triple minimal surface structures: a review. Bioact Mater 4:56–70. https://doi.org/10.1016/j.bioactmat.2018.12.003
Pantoja M, Velasco F, Abenojar J, Martinez MA (2019) Development of superhydrophobic coatings on AISI 304 austenitic stainless steel with different surface pretreatments. Thin Solid Films 671:22–30. https://doi.org/10.1016/j.tsf.2018.12.016
Fathi MH, Doost Mohammadi A (2008) Preparation and characterization of sol–gel bioactive glass coating for improvement of biocompatibility of human body implant. Mater Sci Eng A 474:128–133. https://doi.org/10.1016/j.msea.2007.05.041
Fathi MH, Doostmohammadi A (2009) Bioactive glass nanopowder and bioglass coating for biocompatibility improvement of metallic implant. J Mater Process Technol 209:1385–1391. https://doi.org/10.1016/j.jmatprotec.2008.03.051
Omar SA, Ballarre J, Ceré SM (2016) Protection and functionalization of AISI 316 L stainless steel for orthopedic implants: hybrid coating and sol gel glasses by spray to promote bioactivity. Electrochim Acta 203:309–315. https://doi.org/10.1016/j.electacta.2016.01.051
Al-Rashidy ZM, Farag MM, Ghany NAA et al (2017) Aqueous electrophoretic deposition and corrosion protection of borate glass coatings on 316 L stainless steel for hard tissue fixation. Surfaces Interfaces 7:125–133. https://doi.org/10.1016/j.surfin.2017.03.010
Deposition AL (2010) Atomic layer deposition を用いた磁性薄膜の作製スカーミオンの作製. 250. https://doi.org/https://doi.org/10.1016/B978-1-4377-7867-0.00019-2
George SM (2010) Atomic layer deposition: an overview. Chem Rev 110:111–131. https://doi.org/10.1021/cr900056b
Putkonen M, Sajavaara T, Rahkila P et al (2009) Atomic layer deposition and characterization of biocompatible hydroxyapatite thin films. Thin Solid Films 517:5819–5824. https://doi.org/10.1016/j.tsf.2009.03.013
Wang D, Bierwagen GP (2009) Sol–gel coatings on metals for corrosion protection. Prog Org Coat 64:327–338. https://doi.org/10.1016/j.porgcoat.2008.08.010
Houmard M, Nunes EHM, Vasconcelos DCL et al (2014) Correlation between sol–gel reactivity and wettability of silica films deposited on stainless steel. Appl Surf Sci 289:218–223. https://doi.org/10.1016/j.apsusc.2013.10.137
Pourhashem S, Afshar A (2014) Double layer bioglass-silica coatings on 316L stainless steel by sol–gel method. Ceram Int 40:993–1000. https://doi.org/10.1016/j.ceramint.2013.06.096
Luo J, Jia X, Gu R et al (2018) 316L stainless steel manufactured by selective laser melting and its biocompatibility with or without hydroxyapatite coating. Metals (Basel) 8:548. https://doi.org/10.3390/met8070548
Melo-Fonseca F, Lima R, Costa MM et al (2018) 45S5 BAG-Ti6Al4V structures: The influence of the design on some of the physical and chemical interactions that drive cellular response. Mater Des 160:95–105. https://doi.org/10.1016/j.matdes.2018.08.056
Yamamoto A, Kohyama Y, Kuroda D, Hanawa T (2004) Cytocompatibility evaluation of Ni-free stainless steel manufactured by nitrogen adsorption treatment. Mater Sci Eng C 24:737–743. https://doi.org/10.1016/j.msec.2004.08.017
Zadpoor AA (2019) Additively manufactured porous metallic biomaterials. J Mater Chem B 7:4088–4117. https://doi.org/10.1039/c9tb00420c
Gopi D, Ramya S, Rajeswari D, Kavitha L (2013) Corrosion protection performance of porous strontium hydroxyapatite coating on polypyrrole coated 316L stainless steel. Colloids Surfaces B Biointerfaces 107:130–136. https://doi.org/10.1016/j.colsurfb.2013.01.065
He L, Wang Z, Sheath P et al (2015) Growth of nano-textured graphene coatings across highly porous stainless steel supports towards corrosion resistant coatings. Carbon. https://doi.org/10.1016/j.carbon.2015.02.042
Manakari V, Parande G, Gupta M (2016) Selective laser melting of magnesium and magnesium alloy powders: a review. Metals 7:2
Yan X, Yu C, Zhou X et al (2004) Highly ordered mesoporous bioactive glasses with superior in vitro bone-forming bioactivities. Angew Chemie Int Ed 43:5980–5984. https://doi.org/10.1002/anie.200460598
Brinker CJ, Lu Y, Sellinger A, Fan H (2010) ChemInform abstract: evaporation-induced self-assembly: nanostructures made easy. ChemInform. https://doi.org/10.1002/chin.199928288
Tabia Z, El Mabrouk K, Bricha M, Nouneh K (2019) Mesoporous bioactive glass nanoparticles doped with magnesium: drug delivery and acellular in vitro bioactivity. RSC Adv. https://doi.org/10.1039/C9RA01133A
Bricha M, Belmamouni Y, Essassi EM et al (2013) Hydrothermal synthesis and appraisal of Mg-doped hydroxyapatite nanopowders. J Biomater Tissue Eng 3:570–580. https://doi.org/10.1166/jbt.2013.1120
Belmamouni Y, Bricha M, Ferreira J, El Mabrouk K (2015) Hydrothermal synthesis of Si-doped hydroxyapatite nanopowders: mechanical and bioactivity evaluation. Int J Appl Ceram Technol 12:329–340. https://doi.org/10.1111/ijac.12210
Karapatis N, Egger G (1999) Optimization of powder layer density in selective laser sintering. Int Solid Free Fabr Symp. https://doi.org/10.26153/tsw/746
Zegzulka J, Gelnar D, Jezerska L et al (2018) Internal friction angle of metal powders. Metals (Basel) 8:255. https://doi.org/10.3390/met8040255
Li XN, Chen XM, Hu WL (2009) In Situ synthesis and characterization of β-tricalcium phosphate/Na doped 58S bioglass composite by sol–gel technique. Mater Sci Forum 610–613:1278–1283. https://doi.org/10.4028/www.scientific.net/msf.610-613.1278
Mozafari M, Moztarzadeh F, Tahriri M (2010) Investigation of the physico-chemical reactivity of a mesoporous bioactive SiO2-CaO-P2O5 glass in simulated body fluid. J Non Cryst Solids 356:1470–1478. https://doi.org/10.1016/j.jnoncrysol.2010.04.040
Liu Y, Xue K, YAO S, (2019) Structure, degradation and hydroxyapatite conversion of B-doped 58S bioglass and glass-ceramics. J Ceram Soc Jpn 127:232–241. https://doi.org/10.2109/jcersj2.18206
Chitra S, Bargavi P, Durgalakshmi D et al (2019) Role of sintering temperature dependent crystallization of bioactive glasses on erythrocyte and cytocompatibility. Process Appl Ceram 13:12–23. https://doi.org/10.2298/pac1901012c
Busca G, Lorenzelli V (1982) Materials chemistry infrared spectroscopic identification of species arising from reactive adsorption of carbon oxides on metal oxide surfaces. Mater Chem 7:89–126. https://doi.org/10.1016/0390-6035(82)90059-1
Filgueiras MRT, La Torre G, Hench LL (1993) Solution effects on the surface reactions of three bioactive glass compositions. J Biomed Mater Res 27:1485–1493. https://doi.org/10.1002/jbm.820271204
Bui XV, Dang TH (2019) Bioactive glass 58S prepared using an innovation sol–gel process. Process Appl Ceram 13:98–103
Joughehdoust S, Manafi S (2012) Synthesis and in vitro investigation of sol–gel derived bioglass-58S nanopowders. Mater Sci Pol 30:45–52. https://doi.org/10.2478/s13536-012-0007-2
Gong W, Dong Y, Wang S et al (2017) A novel nano-sized bioactive glass stimulates osteogenesis via the MAPK pathway. RSC Adv 7:13760–13767. https://doi.org/10.1039/c6ra26713k
Gu D, Shen Y (2009) Balling phenomena in direct laser sintering of stainless steel powder: metallurgical mechanisms and control methods. Mater Des 30:2903–2910. https://doi.org/10.1016/j.matdes.2009.01.013
Mahmoud D, Elbestawi MA (2019) Selective laser melting of porosity graded lattice structures for bone implants. Int J Adv Manuf Technol 100:2915–2927. https://doi.org/10.1007/s00170-018-2886-9
Gopi D, Murugan N, Ramya S, Kavitha L (2014) Electrodeposition of a porous strontium-substituted hydroxyapatite/zinc oxide duplex layer on AZ91 magnesium alloy for orthopedic applications. J Mater Chem B 2:5531–5540. https://doi.org/10.1039/c4tb00960f
Arumugam MK, Hussein MA, Adesina AY (2019) In vitro corrosion and bioactivity performance of surface-treated Ti-20Nb-13Zr alloys for orthopedic applications. Coatings 9:344
Sidane D, Khireddine H, Yala S et al (2015) Morphological and mechanical properties of hydroxyapatite bilayer coatings deposited on 316L SS by sol–gel method. Metall Mater Trans B Process Metall Mater Process Sci 46:2340–2347. https://doi.org/10.1007/s11663-015-0397-8
Sidane D, Khireddine H, Bir F et al (2017) Hydroxyapatite-TiO2-SiO2-coated 316L stainless steel for biomedical application. Metall Mater Trans A Phys Metall Mater Sci 48:3570–3582. https://doi.org/10.1007/s11661-017-4108-8
Bricha M, Belmamouni Y, Essassi EM et al (2012) Surfactant-assisted hydrothermal synthesis of hydroxyapatite nanopowders. J Nanosci Nanotechnol 12:8042–8049. https://doi.org/10.1166/jnn.2012.6664
Taghian Dehaghani M, Ahmadian M, Fathi M (2015) Synthesis, Characterization, and Bioactivity Evaluation of Amorphous and Crystallized 58S Bioglass Nanopowders. Int J Appl Ceram Technol 12:867–874. https://doi.org/10.1111/ijac.12293
Kokubo T, Kushitani H, Sakka S et al (1990) Solutions able to reproduce in vivo surface-structure changes in bioactive glass-ceramic A-W3. J Biomed Mater Res 24:721–734. https://doi.org/10.1002/jbm.820240607
Xia W, Chang J (2008) Preparation, in vitro bioactivity and drug release property of well-ordered mesoporous 58S bioactive glass. J Non Cryst Solids 354:1338–1341. https://doi.org/10.1016/j.jnoncrysol.2006.10.084
Acknowledgements
Authors address their acknowledgements to the National Center of Scientific and Technological Research, CNRST (Rabat, Morocco), the Regional Council Fes-Meknes and the Euromed University of Fes for supporting the present study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Handling Editor: Annela M. Seddon.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tabia, Z., Bricha, M., El Mabrouk, K. et al. Manufacturing of a metallic 3D framework coated with a bioglass matrix for implant applications. J Mater Sci 56, 1658–1672 (2021). https://doi.org/10.1007/s10853-020-05370-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-020-05370-3