Abstract
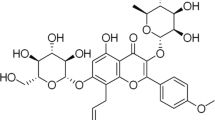
Chemotherapeutic drugs have shown some limitations in anti-tumor treatment, such as drug resistance, high toxicity and limited regime of clinical uses. Natural products have attracted extensive attention as potential source of unmodified chemical compounds for disease treatment. Withaferin A (WA) has the potential to inhibit multiple human tumors, but it is hardly available for oral administration due to its low water solubility and its side effects. We developed a methoxy poly(ethylene glycol) (mPEG) conjugated poly(d,l-lactide-co-glycolide) (PLGA) drug carrier particles to encapsulate WA for pancreatic cancer treatment. The results showed that WA does not lose its physicochemical properties after encapsulation, and our drug carriers are completely degraded within 1 month. We used the WA-loaded mPEG–PLGA particles for pancreatic cancer cell treatment where it exhibited stronger inhibition than free drug (WA) at the early treatment stage. Our formulation of the drug carriers provides an efficient encapsulation of WA that allows it bonding with heat shock proteins, thereby reducing the expression of AKT and CDK4 proteins to induce apoptosis in cancer cells. Together, our data demonstrate that mPEG–PLGA loaded with WA can achieve the design goals for cancer therapy given its advantages of sustained release and degradation property to reduce the side effect of WA, which provides a possibility for WA to be used in clinical applications.




Similar content being viewed by others
References
Kumar M, Liu ZR, Thapa L, Wang DY, Tian R, Qin RY (2004) Mechanisms of inhibition of growth of human pancreatic carcinoma implanted in nude mice by somatostatin receptor subtype 2. Pancreas 29(2):141–151
Michl P, Gress TM (2013) Current concepts and novel targets in advanced pancreatic cancer. Gut 62(2):317–326
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics. CA Cancer J Clin 62(1):10–29
Nd MW (2006) Ancient medicine, modern use: withania somnifera and its potential role in integrative oncology. Altern Med Rev 11:269–278
Kumar M, Liu ZR, Thapa L, Qin RY (2004) Anti-angiogenic effects of somatostatin receptor subtype 2 on human pancreatic cancer xenografts. Carcinogenesis 25(11):2075–2081
Okamoto S, Tsujioka T, Suemori S, Kida J, Kondo T, Tohyama Y, Tohyama K (2016) Withaferin A suppresses the growth of myelodysplasia and leukemia cell lines by inhibiting cell cycle progression. Cancer Sci 107(9):1302–1314
Wang Z, Dabrosin C, Yin X et al (2015) Broad targeting of angiogenesis for cancer prevention and therapy. Semin Cancer Biol 35(Suppl):S224–S243
Debernardi S, Massat NJ, Radon TP, Sangaralingam A, Banissi A, Ennis DP, Dowe T, Chelala C et al (2015) Noninvasive urinary miRNA biomarkers for early detection of pancreatic adenocarcinoma. Am J Cancer Res 5(11):3455–3466
Li X, Zhu F, Jiang JX, Sun CY, Wang X, Shen M, Tian R, Shi CJ et al (2015) Synergistic antitumor activity of withaferin A combined with oxaliplatin triggers reactive oxygen species-mediated inactivation of the PI3 K/AKT pathway in human pancreatic cancer cells. Cancer Lett 357(1):219–230
Matsuda Y, Naito Z, Kawahara K, Nakazawa N, Korc M, Ishiwata T (2011) Nestin is a novel target for suppressing pancreatic cancer cell migration, invasion and metastasis. Cancer Biol Ther 11(5):512–523
Aqil F, Jeyabalan J, Kausar H, Bansal SS, Sharma RJ, Singh IP, Vadhanam MV, Gupta RC (2012) Multi-layer polymeric implants for sustained release of chemopreventives. Cancer Lett 326(1):33–40
Han YC, Li SP, Cao XY, Yuan L, Wang YF, Yin YX, Qiu T, Dai HL, Wang XY (2014) Different inhibitory effect and mechanism of hydroxyapatite nanoparticles on normal cells and cancer cells in vitro and in vivo. Sci Rep 4:7134
Wang H, Zhao Y, Wu Y, Hu YL, Nan KH, Nie GJ, Chen H (2011) Enhanced anti-tumor efficacy by co-delivery of doxorubicin and paclitaxel with amphiphilic methoxy PEG–PLGA copolymer nanoparticles. Biomaterials 32(32):8281–8290
Bhatnagar P, Kumari M, Pahuja R, Pant AB, Shukla Y, Kumar P, Gupta KC (2018) Hyaluronic acid-grafted PLGA nanoparticles for the sustained delivery of berberine chloride for an efficient suppression of Ehrlich ascites tumors. Drug Deliv Transl Res 8(3):565–579
Park J, Fong PM, Lu J, Russell KS, Booth CJ, Saltzman WM, Fahmy TM (2009) PEGylated PLGA nanoparticles for the improved delivery of doxorubicin. Nanomed Nanotechnol Biol Med 5(4):410–418
Shen M, Xu YY, Sun Y, Han BS, Duan YR (2015) Preparation of a thermosensitive gel composed of a mPEG–PLGA–PLL–cRGD nanodrug delivery system for pancreatic tumor therapy. ACS Appl Mater Interfaces 7(37):20530–20537
Cu Y, Saltzman WM (2009) Controlled surface modification with poly(ethylene)glycol enhances diffusion of PLGA nanoparticles in human cervical mucus. Mol Pharm 6(1):173–181
Danhier F, Lecouturier N, Vroman B, Jerome C, Marchand-Brynaert J, Feron O, Preat V (2009) Paclitaxel-loaded PEGylated PLGA-based nanoparticles: in vitro and in vivo evaluation. J Control Release 133(1):11–17
Zhang KR, Tang X, Zhang J, Lu W, Lin X, Zhang Y, Tian B, Yang H et al (2014) PEG–PLGA copolymers: their structure and structure-influenced drug delivery applications. J Control Release 183:77–86
Li J, Jiang GQ, Ding FX (2008) The effect of pH on the polymer degradation and drug release from PLGA–mPEG microparticles. J Appl Polym Sci 109(1):475–482
Guo Y, He W, Yang S, Zhao D, Li Z, Luan Y (2017) Co-delivery of docetaxel and verapamil by reduction-sensitive PEG–PLGA–SS–DTX conjugate micelles to reverse the multi-drug resistance of breast cancer. Colloids Surf B Biointerfaces 151:119–127
Liu P, Yu H, Sun Y, Zhu M, Duan Y (2012) A mPEG–PLGA–b-PLL copolymer carrier for adriamycin and siRNA delivery. Biomaterials 33(17):4403–4412
Qureshi WA, Zhao RF, Wang H, Ji TJ, Ding YP, Ihsan A, Mujeeb A, Nie GJ et al (2016) Co-delivery of doxorubicin and quercetin via mPEG–PLGA copolymer assembly for synergistic anti-tumor efficacy and reducing cardio-toxicity. Sci Bull 61(21):1689–1698
Wang L, Hu Y, Hao Y, Li L, Zheng C, Zhao H et al (2018) Tumor-targeting core-shell structured nanoparticles for drug procedural controlled release and cancer sonodynamic combined therapy. J Control Release 286:74–84
Zhang X, Wang Q, Qin L, Fu H, Fang Y, Han B, Duan Y (2016) EGF-modified mPEG–PLGA–PLL nanoparticle for delivering doxorubicin combined with Bcl-2 siRNA as a potential treatment strategy for lung cancer. Drug Deliv 23(8):2936–2945
Mosquera J, Garcia I, Liz-Marzan LM (2018) Cellular uptake of nanoparticles versus small molecules: a matter of size. Accounts Chem Res 51(9):2305–2313
Zhou YQ, Peng ZL, Seven ES, Leblanc RM (2018) Crossing the blood-brain barrier with nanoparticles. J Control Release 270:290–303
He Z, Sun Y, Cao J, Duan Y (2016) Degradation behavior and biosafety studies of the mPEG–PLGA–PLL copolymer. Phys Chem Chem Phys 18(17):11986–11999
Teng Y, Bai M, Sun Y, Wang Q, Li F, Duan Y et al (2015) Enhanced delivery of PEAL nanoparticles with ultrasound targeted microbubble destruction mediated siRNA transfection in human MCF-7/S and MCF-7/ADR cells in vitro. Int J Nanomed 10:5447–5457
Hanson JA, Chang CB, Graves SM, Li Z, Mason TG, Deming TJ (2008) Nanoscale double emulsions stabilized by single-component block copolypeptides. Nature 455(7209):85–88
Dinsmore AD, Hsu MF, Nikolaides MG, Marquez M, Bausch AR, Weitz DA (2002) Colloidosomes: selectively permeable capsules composed of colloidal particles. Science 298(5595):1006–1009
Moussa EM, Panchal JP, Moorthy BS, Blum JS, Joubert MK, Narhi LO, Topp EM (2016) Immunogenicity of therapeutic protein aggregates. J Pharm Sci 105(2):417–430
Nunes C, Suryanarayanan R, Botez CE, Stephens PW (2004) Characterization and crystal structure of d-mannitol hemihydrate. J Pharm Sci 93(11):2800–2809
Garidel P, Pevestorf B, Bahrenburg S (2015) Stability of buffer-free freeze-dried formulations: a feasibility study of a monoclonal antibody at high protein concentrations. Eur J Pharm Biopharm 97:125–139
Nicoud L, Owczarz M, Arosio P, Morbidelli M (2015) A multiscale view of therapeutic protein aggregation: a colloid science perspective. Biotechnol J 10(3):367–378
Wen L, Zheng X, Wang X, Lan H, Yin Z (2017) Bilateral effects of excipients on protein stability: preferential interaction type of excipient and surface aromatic hydrophobicity of protein. Pharm Res 34(7):1378–1390
Aryal S, Prabaharan M, Pilla S, Gong S (2009) Biodegradable and biocompatible multi-arm star amphiphilic block copolymer as a carrier for hydrophobic drug delivery. Int J Biol Macromol 44(4):346–352
Decuzzi P, Godin B, Tanaka T, Lee SY, Chiappini C, Liu X, Ferrari M (2010) Size and shape effects in the biodistribution of intravascularly injected particles. J Control Release 141(3):320–327
Gu M, Yu Y, Gunaherath G, Gunatilaka A, Li D, Sun D (2014) Structure–activity relationship (SAR) of withanolides to inhibit Hsp90 for its activity in pancreatic cancer cells. Invest New Drugs 32(1):68–74
Liu X, Qi W, Cooke LS, Kithsiri Wijeratne EM, Xu Y, Marron MT, Leslie Gunatilaka AA, Mahadevan D (2011) An analog of withaferin A activates the MAPK and glutathione “stress” pathways and inhibits pancreatic cancer cell proliferation. Cancer Invest 29(10):668–675
Yoneyama T, Arai MA, Sadhu SK, Ahmed F, Ishibashi M (2015) Hedgehog inhibitors from Withania somnifera. Bioorg Med Chem Lett 25(17):3541–3544
Bauer TW, Liu W, Fan F, Camp ER, Yang A, Somcio RJ et al (2005) Targeting of urokinase plasminogen activator receptor in human pancreatic carcinoma cells inhibits c-Met- and insulin-like growth factor-I receptor-mediated migration and invasion and orthotopic tumor growth in mice. Cancer Res 65(17):7775–7781
Bi Y, Min M, Shen W, Liu Y (2016) Numb/Notch signaling pathway modulation enhances human pancreatic cancer cell radiosensitivity. Tumour Biol 37(11):15145–15155
Gu WJ, Liu HL (2013) Induction of pancreatic cancer cell apoptosis, invasion, migration, and enhancement of chemotherapy sensitivity of gemcitabine, 5-FU, and oxaliplatin by hnRNP A2/B1 siRNA. Anticancer Drugs 24(6):566–576
Kikuta K, Masamune A, Watanabe T, Ariga H, Itoh H, Hamada S et al (2010) Pancreatic stellate cells promote epithelial–mesenchymal transition in pancreatic cancer cells. Biochem Biophys Res Commun 403(3–4):380–384
Sun XD, Liu XE, Huang DS (2013) Curcumin reverses the epithelial–mesenchymal transition of pancreatic cancer cells by inhibiting the Hedgehog signaling pathway. Oncol Rep 29(6):2401–2407
Xu WT, Bian ZY, Fan QM, Li G, Tang TT (2009) Human mesenchymal stem cells (hMSCs) target osteosarcoma and promote its growth and pulmonary metastasis. Cancer Lett 281(1):32–41
Yin Y, Lin Q, Sun H, Chen D, Wu Q, Chen X, Li S (2012) Cytotoxic effects of ZnO hierarchical architectures on RSC96 Schwann cells. Nanoscale Res Lett 7:439
Sun HL, Dai XW, Han B (2014) TRIM29 as a novel biomarker in pancreatic adenocarcinoma. Dis Markers. https://doi.org/10.1155/2014/317817
Yu Y, Hamza A, Zhang T, Gu M, Zou P, Newman B et al (2010) Withaferin A targets heat shock protein 90 in pancreatic cancer cells. Biochem Pharmacol 79(4):542–551
Xia Y, Rocchi P, Iovanna JL, Peng L (2012) Targeting heat shock response pathways to treat pancreatic cancer. Drug Discov Today 17(1–2):35–43
Xia S, Miao Y, Liu S (2018) Withaferin A induces apoptosis by ROS-dependent mitochondrial dysfunction in human colorectal cancer cells. Biochem Biophys Res Commun 503(4):2363–2369
Sherr CJ, McCormick F (2002) The RB and p53 pathways in cancer. Cancer Cell 2:103–112
Acknowledgements
This work was supported by National Key Research and Development Program of China (No. 2016YFC1101302), and the National Natural Science Foundation of China (81773160, 51572206), HUBEI Natural Science Foundation (2017CFB467) to MW, and Tongji Hospital Science Fund for Distinguished Young Scholars (2017) to MW.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shao, Q., Feng, Y., Wang, W. et al. Drug carrier for sustained release of withaferin A for pancreatic cancer treatment. J Mater Sci 55, 1702–1714 (2020). https://doi.org/10.1007/s10853-019-04139-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-019-04139-7