Abstract
Purpose
Limited research has been published comparing PIEZO-ICSI with conventional ICSI. While positive effects have been documented in improving fertilization and degeneration, the outcomes in patients with previous poor results from conventional ICSI remain unclear. It is hypothesized that these patients may benefit the most from this form of insemination.
Methods
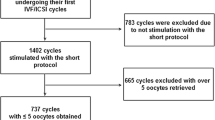
This retrospective paired within-patient cohort study investigated patients (n=72) undertaking PIEZO-ICSI after a previous conventional ICSI cycle resulted in poor outcomes (including low fertilization (<50%), high degeneration (>15%), and/or poor embryo development and utilization). Patients required at least five oocytes collected in both cycles and a period of less than 2 years between the cycles. The outcomes of both cycles were compared in respect to fertilization, degeneration, embryo utilization, and pregnancy rates. Further analyses were applied to patients <38 and ≥38 years of age, with <50% or ≥50% fertilization with conventional ICSI and with <20% or ≥20% utilization with conventional ICSI.
Results
PIEZO-ICSI resulted in significantly higher fertilization (61.9% vs 45.3%, P<0.0001) and lower degeneration (7.7% vs 18.2%, P=0.0001) when compared to the conventional ICSI cycles. The greatest benefit was seen in patients who had less than 50% fertilization or <20% utilization in their conventional ICSI cycle, with improvements in fertilization and degeneration rates resulting in a significantly higher number of embryos utilized (frozen or transferred) per cycle.
Conclusions
PIEZO-ICSI improved fertilization, degeneration, and utilization rates in patients with previous poor outcomes from conventional ICSI. The number of embryos available for use per cycle was also increased. Further significant improvements were achieved in patients who exhibited poor fertilization (<50%) or low utilization (<20%) from conventional ICSI.
Similar content being viewed by others
References
Palermo G, Joris H, Devroey P, Van Steirteghem A. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17–8. https://doi.org/10.1016/0140-6736(92)92425-f.
Esteves SC, Roque M, Bedoschi G, Haahr T, Humaidan P. Intracytoplasmic sperm injection for male infertility and consequences for offspring. Nat Rev Urol. 2018;15(9):535–62. https://doi.org/10.1038/s41585-018-0051-8.
Rubino P, Viganò P, Luddi A, Piomboni P. The ICSI procedure from past to future: a systematic review of the more controversial aspects. Hum Reprod Update. 2016;22:194–227. https://doi.org/10.1093/humupd/dmv050.
European IVF-Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE), Wyns C, De Geyter C, Calhaz-Jorge C, Kupka MS, Motrenko T, Smeenk J, Bergh C, Tandler-Schneider A, Rugescu IA, Vidakovic S, Goossens V. ART in Europe, 2017: results generated from European registries by ESHRE. Hum Reprod Open. 2021;2021(3). https://doi.org/10.1093/hropen/hoab026.
Ebner T, Yaman C, Moser M, Sommergruber M, Jesacher K, Tews G. A prospective study on oocyte survival rate after ICSI: influence of injection technique and morphological features. J Assist Reprod Genet. 2001;18:623–8. https://doi.org/10.1023/a:1013171505702.
Yanagida K, Katayose H, Yazawa H, Kimura Y, Konnai K, Sato A. The usefulness of a piezo-micromanipulator in intracytoplasmic sperm injection in humans. Hum Reprod. 1999;14(2):448–53. https://doi.org/10.1093/humrep/14.2.448.
Fujii Y, Endo Y, Mitsuhata S, Hayashi M, Motoyama H. Evaluation of the effect of piezo-intracytoplasmic sperm injection on the laboratory, clinical, and neonatal outcomes. Reprod Med Biol. 2020;19:198–205. https://doi.org/10.1002/rmb2.12324.
Furuhashi K, Saeki Y, Enatsu N, Iwasaki T, Ito K, Mizusawa Y, Matsumoto Y, Kokeguchi S, Shiotani M. Piezo-assisted ICSI improves fertilization and blastocyst development rates compared with conventional ICSI in women aged more than 35 years. Reprod Med Biol. 2019;18(4):357–61. https://doi.org/10.1002/rmb2.12290.
Kimura Y, Yanagimachi R. Intracytoplasmic sperm injection in the mouse. Biol Reprod. 1995;52(4):709–20. https://doi.org/10.1095/biolreprod52.4.709.
Katayose H, Yanagida K, Shinoki T, Kawahara T, Horiuchi T, Sato A. Efficient injection of bull spermatozoa into oocytes using a Piezo-driven pipette. Theriogenology. 1999;52(7):1215–24. https://doi.org/10.1016/S0093-691X(99)00213-7.
Salgado RM, Brom-de-Luna JG, Resende HL, Canesin HS, Hinrichs K. Lower blastocyst quality after conventional vs. Piezo ICSI in the horse reflects delayed sperm component remodeling and oocyte activation. J Assist Reprod Genet. 2018;35:825–40. https://doi.org/10.1007/s10815-018-1174-9.
Huang T, Kimura Y, Yanagimachi R. The use of piezo micromanipulation for intracytoplasmic sperm injection of human oocytes. J Assist Reprod Genet. 1996;13(4):320–8. https://doi.org/10.1007/BF02070146.
Yoshida N, Perry AC. Piezo-actuated mouse intracytoplasmic sperm injection (ICSI). Nat Protoc. 2007;2(2):296–304. https://doi.org/10.1038/nprot.2007.7.
Hiraoka K, Kitamura S. Clinical efficiency of Piezo-ICSI using micropipettes with a wall thickness of 0.625 μm. J Assist Reprod Genet. 2015;32:1827–33. https://doi.org/10.1007/s10815-015-0597-9.
Zander-Fox D, Lam K, Pacella-Ince L, Tully C, Hamilton H, Hiraoka K, et al. PIEZO-ICSI increases fertilization rates compared with standard ICSI: a prospective cohort study. Reprod Biomed Online. 2021;43(3):404–12. https://doi.org/10.1016/j.rbmo.2021.05.020.
Takeuchi S, Minoura H, Shibahara T, Shen X, Futamura N, Toyoda N. Comparison of piezo-assisted micromanipulation with conventional micromanipulation for intracytoplasmic sperm injection into human oocytes. Gynecol Obstet Invest. 2001;52:158–62. https://doi.org/10.1159/000052965.
Newman JE, Paul RC, Chambers GM. Assisted reproductive technology in Australia and New Zealand 2019. Sydney: National Perinatal Epidemiology and Statistics Unit, the University of New South Wales, Sydney. 2021. https://npesu.unsw.edu.au/surveillance/assisted-reproductive-technology-australia-and-new-zealand-2019. Accessed 6 Dec 2021.
Nwandison M, Bewley S. What is the right age to reproduce? Fet Matern Med Rev. 2006;17(3):185–204. https://doi.org/10.1017/S0965539506001781.
Motteram C, Vollenhoven B, Hope N, Osianlis T, Rombauts LJ. Live birth rates after combined adjuvant therapy in IVF-ICSI cycles: a matched case-control study. Reprod Biomed Online. 2015;30(4):340–8. https://doi.org/10.1016/j.rbmo.2014.12.004.
Popkiss S, Horta F, Vollenhoven B, Green MP, Zander-Fox D. Calcium chloride dihydrate supplementation at ICSI improves fertilization and pregnancy rates in patients with previous low fertilization: a retrospective paired treatment cycle study. J Assist Reprod Genet. 2022;39(5):1055–64. https://doi.org/10.1007/s10815-022-02407-1.
Alvarez GM, Villanueva S, Geller M, Cetica P, Dalvit G. PIEZO-ICSI as alternative tool to improve oocyte activation in in vitro matured bovine oocytes model. Fertil Steril. 2018;110:e217.
ESHRE Special Interest Group of Embryology and Alpha Scientists in Reproductive Medicine. The Vienna consensus: report of an expert meeting on the development of ART laboratory performance indicators. Reprod Biomed Online. 2017;35(5):494–510. https://doi.org/10.1016/j.rbmo.2017.06.015.
Rosen MP, Shen S, Dobson AT, Fujimoto VY, McCulloch CE, Cedars MI. Oocyte degeneration after intracytoplasmic sperm injection: a multivariate analysis to assess its importance as a laboratory or clinical marker. Fertil Steril. 2006;85(6):1736–43. https://doi.org/10.1016/j.fertnstert.2005.12.017.
Heffner LJ. Advanced maternal age–how old is too old? N Engl J Med. 2004;351(19):1927–9. https://doi.org/10.1056/NEJMp048087.
Grøndahl ML, Christiansen SL, Kesmodel US, Agerholm IE, Lemmen JG, Lundstrøm P, Bogstad J, Raaschou-Jensen M, Ladelund S. Effect of women’s age on embryo morphology, cleavage rate and competence-a multicenter cohort study. PLoS One. 2017;12(4):e0172456. https://doi.org/10.1371/journal.pone.0172456.
Cimadomo D, Fabozzi G, Vaiarelli A, Ubaldi N, Ubaldi FM, Rienzi L. Impact of maternal age on oocyte and embryo competence. Front Endocrinol. 2018;9:327. https://doi.org/10.3389/fendo.2018.00327.
Spandorfer SD, Davis OK, Barmat LI, Chung PH, Rosenwaks Z. Relationship between maternal age and aneuploidy in in vitro fertilization pregnancy loss. Fertil Steril. 2004;81(5):1265–9. https://doi.org/10.1016/j.fertnstert.2003.09.057.
Mikwar M, MacFarlane AJ, Marchetti F. Mechanisms of oocyte aneuploidy associated with advanced maternal age. Mutat Res Rev Mutat Res. 2020;785:108320. https://doi.org/10.1016/j.mrrev.2020.108320.
Hiraoka K, Isuge M, Kamada Y, Kaji T, Suhara T, Kuga A, Ohuchi K, Hayashi M, Kawai K. Piezo-ICSI for human oocytes. J Vis Exp 2021; (170). https://doi.org/10.3791/60224.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Caddy, M., Popkiss, S., Weston, G. et al. PIEZO-ICSI increases fertilization rates compared with conventional ICSI in patients with poor prognosis. J Assist Reprod Genet 40, 389–398 (2023). https://doi.org/10.1007/s10815-022-02701-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02701-y