Abstract
Objective
To assess rates of successful testicular sperm retrieval and intracytoplasmic sperm injection (ICSI) outcome in cancer survivors affected by non-obstructive azoospermia (NOA) or retrograde ejaculation (RE)/failure of emission (FOE).
Methods
A retrospective analysis of cancer survivors who did not cryopreserve sperm prior to treatment undergoing testicular sperm extraction (TESE). Non-cancer NOA patients and neurologic RE/FOE were the control group.
Results
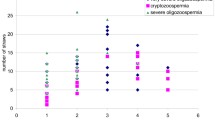
A total of 97 cancer survivors were offered TESE and 88 (91%) accepted. Sperm was retrieved and cryopreserved in 34/67 patients with NOA (50.7%) and in 21/21 patients affected by RE/FOE (100%). Sperm retrieval rates were similar in the control group (44.9% in NOA and 100% in RE/FOE). The ICSI cumulative pregnancy rate (60%) and live birth rate (40%) per couple in 30 NOA men did not differ from controls (50.0 and 46.5%, respectively; p = 0.399/0.670). The cumulative pregnancy rate (66.7%) and live birth rate (55.6%) in 18 RE/FOE men did not differ from the control group (38.9 and 33.3%, respectively; p = 0.181/0.315). The cancer type and the resulting infertility disorder (NOA or RE/FOE) were not associated with ICSI outcomes. Female partner age was inversely related to the cumulative live birth rate, being fourfold lower (11.5%) in women ≥ 40 years and 48.8% in younger women (p = 0.0037).
Conclusions
The rate of successful TESE and the ICSI outcome in cancer survivors with NOA and RE/FOE is the same as non-cancer azoospermic patients. Female partner age (older than 40 years) was associated with a significant reduction in live birth rates after TESE-ICSI procedures.

Similar content being viewed by others
References
Botchan A, Karpol S, Lehavi O, Paz G, Kleiman SE, Yogev L, et al. Preservation of sperm of cancer patients: extent of use and pregnancy outcome in a tertiary infertility center. Asian J Androl. 2013;15:382–6.
Hotaling JM, Lopushnyan NA, Davenport M, Christensen H, Pagel ER, Muller CH, et al. Raw and test-thaw semen parameters after cryopreservation among men with newly diagnosed cancer. Fertil Steril. 2013;99:464–9.
Rives N, Perdrix A, Hennebicq S, Saias-Magnan J, Melin MC, Berthaut I, et al. The semen quality of 1158 men with testicular cancer at the time of cryopreservation: results of the French National CECOS Network. J Androl. 2012;33:1394–401.
Tournaye H, Goossens E, Verheyen G, Frederickx V, De Block G, Devroey P, et al. Preserving the reproductive potential of men and boys with cancer: current concepts and future prospects. Hum Reprod Update. 2004;10:525–32.
Nieschlag EBH, Wieacker P, Meschede D, Kamischke A, Kliesch S. Disorders at the testicular level. In: Nieschlag EBH, Wieacker P, Meschede D, Kamischke A, Kliesch S, editors. Andrology. Heidelberg: Springer-Verlag Berlin; 2010. p. 193–238.
Ethics ETFo, Law. Taskforce 7: ethical considerations for the cryopreservation of gametes and reproductive tissues for self use. Hum Reprod. 2004;19:460–2.
Oktay K, Harvey BE, Loren AW. Fertility preservation in patients with cancer: ASCO clinical practice guideline update summary. J Oncol Pract. 2018;14:381–5.
Daudin M, Rives N, Walschaerts M, Drouineaud V, Szerman E, Koscinski I, et al. Sperm cryopreservation in adolescents and young adults with cancer: results of the French national sperm banking network (CECOS). Fertil Steril. 2015;103:478–86 e1.
Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20:1890–7.
Chan PT, Palermo GD, Veeck LL, Rosenwaks Z, Schlegel PN. Testicular sperm extraction combined with intracytoplasmic sperm injection in the treatment of men with persistent azoospermia postchemotherapy. Cancer. 2001;92:1632–7.
Kiekens C, Spiessens C, Duyck F, Vandenweghe D, Coucke W, Vanderschueren D. Pregnancy after electroejaculation in combination with intracytoplasmic sperm injection in a patient with idiopathic anejaculation. Fertil Steril. 1996;66:834–6.
Hsiao W, Deveci S, Mulhall JP. Outcomes of the management of post-chemotherapy retroperitoneal lymph node dissection-associated anejaculation. BJU Int. 2012;110:1196–200.
World Health Organization DoRHaR. WHO laboratory manual for the examination and processing of human semen. Fifth ed. WHO: Geneva; 2010.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 3rd ed. Cambridge: Published on behalf of the World Health Organization by Cambridge University Press; 1992.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Published on behalf of the World Health Organization by Cambridge University Press; 1999.
Schoor RA, Elhanbly S, Niederberger CS, Ross LS. The role of testicular biopsy in the modern management of male infertility. J Urol. 2002;167:197–200.
Hendriks DJ, Mol BW, Bancsi LF, Te Velde ER, Broekmans FJ. Antral follicle count in the prediction of poor ovarian response and pregnancy after in vitro fertilization: a meta-analysis and comparison with basal follicle-stimulating hormone level. Fertil Steril. 2005;83:291–301.
La Marca A, Sighinolfi G, Radi D, Argento C, Baraldi E, Artenisio AC, et al. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update. 2010;16:113–30.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26:1616–24.
Negri L, Albani E, DiRocco M, Morreale G, Novara P, Levi-Setti PE. Testicular sperm extraction in azoospermic men submitted to bilateral orchidopexy. Hum Reprod. 2003;18:2534–9.
Hauser R, Botchan A, Amit A, Ben Yosef D, Gamzu R, Paz G, et al. Multiple testicular sampling in non-obstructive azoospermia--is it necessary? Hum Reprod. 1998;13:3081–5.
Ziegler WF, Chapitis J. Human motile sperm recovery after cryopreservation: freezing in nitrogen vapor vs the direct plunge technique. Prim Care Update Ob Gyns. 1998;5:170.
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17–8.
Levi Setti PE, Albani E, Matteo M, Morenghi E, Zannoni E, Baggiani AM, et al. Five years (2004-2009) of a restrictive law-regulating ART in Italy significantly reduced delivery rate: analysis of 10,706 cycles. Hum Reprod. 2013;28:343–9.
Sharpe RM, Skakkebaek NE. Testicular dysgenesis syndrome: mechanistic insights and potential new downstream effects. Fertil Steril. 2008;89:e33–8.
Bleyer A VA, Barr R. Cancer epidemiology in older adolescents and young adults 15 to 29 years of age, including SEER incidence and survival: 1975–2000: National Cancer Institute, Bethesda; 2006.
Tournaye H, Dohle GR, Barratt CL. Fertility preservation in men with cancer. Lancet. 2014;384:1295–301.
Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes. Br J Cancer. 2013;108:1602–15.
Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952–7.
Gilbert K, Nangia AK, Dupree JM, Smith JF, Mehta A. Fertility preservation for men with testicular cancer: is sperm cryopreservation cost effective in the era of assisted reproductive technology? Urol Oncol. 2018;36:92 e1–9.
Ragni G, Somigliana E, Restelli L, Salvi R, Arnoldi M, Paffoni A. Sperm banking and rate of assisted reproduction treatment: insights from a 15-year cryopreservation program for male cancer patients. Cancer. 2003;97:1624–9.
Bahadur G, Ozturk O, Muneer A, Wafa R, Ashraf A, Jaman N, et al. Semen quality before and after gonadotoxic treatment. Hum Reprod. 2005;20:774–81.
Magelssen H, Haugen TB, von During V, Melve KK, Sandstad B, Fossa SD. Twenty years experience with semen cryopreservation in testicular cancer patients: who needs it? Eur Urol. 2005;48:779–85.
Bizet P, Saias-Magnan J, Jouve E, Grillo JM, Karsenty G, Metzler-Guillemain C, et al. Sperm cryopreservation before cancer treatment: a 15-year monocentric experience. Reprod BioMed Online. 2012;24:321–30.
Pettus JA, Carver BS, Masterson T, Stasi J, Sheinfeld J. Preservation of ejaculation in patients undergoing nerve-sparing postchemotherapy retroperitoneal lymph node dissection for metastatic testicular cancer. Urology. 2009;73:328–31 discussion 31-2.
Damani MN, Master V, Meng MV, Burgess C, Turek P, Oates RD. Postchemotherapy ejaculatory azoospermia: fatherhood with sperm from testis tissue with intracytoplasmic sperm injection. J Clin Oncol. 2002;20:930–6.
Dar S, Orvieto R, Levron J, Haas J, Gat I, Raviv G. IVF outcome in azoospermic cancer survivors. Eur J Obstet Gynecol Reprod Biol. 2018;220:84–7.
Hibi H, Ohori T, Yamada Y, Honda N, Hashiba Y, Asada Y. Testicular sperm extraction and ICSI in patients with post-chemotherapy non-obstructive azoospermia. Arch Androl. 2007;53:63–5.
Hsiao W, Stahl PJ, Osterberg EC, Nejat E, Palermo GD, Rosenwaks Z, et al. Successful treatment of postchemotherapy azoospermia with microsurgical testicular sperm extraction: the Weill Cornell experience. J Clin Oncol. 2011;29:1607–11.
Meseguer M, Garrido N, Remohi J, Pellicer A, Simon C, Martinez-Jabaloyas JM, et al. Testicular sperm extraction (TESE) and ICSI in patients with permanent azoospermia after chemotherapy. Hum Reprod. 2003;18:1281–5.
Shin T, Kobayashi T, Shimomura Y, Iwahata T, Suzuki K, Tanaka T, et al. Microdissection testicular sperm extraction in Japanese patients with persistent azoospermia after chemotherapy. Int J Clin Oncol. 2016;21:1167–71.
Shiraishi K, Matsuyama H. Microdissection testicular sperm extraction and salvage hormonal treatment in patients with postchemotherapy azoospermia. Urology. 2014;83:100–6.
Zorn B, Virant-Klun I, Stanovnik M, Drobnic S, Meden-Vrtovec H. Intracytoplasmic sperm injection by testicular sperm in patients with aspermia or azoospermia after cancer treatment. Int J Androl. 2006;29:521–7.
Practice Committee of the American Society for Reproductive M. Aging and infertility in women. Fertil Steril. 2006;86:S248–52.
Stahl O, Eberhard J, Cavallin-Stahl E, Jepson K, Friberg B, Tingsmark C, et al. Sperm DNA integrity in cancer patients: the effect of disease and treatment. Int J Androl. 2009;32:695–703.
Acknowledgments
The authors would like to thank Renzo Benaglia, Luca Cafaro and Alessandro Pizzocaro for their surgical and endocrinological support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by our hospital’s Institutional Ethics Committee, and all patients provided written informed consent for the scientific use of their clinical data. All the authors are consent to publication. The corresponding author has full control of all primary data. The datasets used and/or analysed during the current study have been sent to the publisher as supplementary material.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Levi-Setti, P.E., Negri, L., Baggiani, A. et al. Testicular sperm extraction and intracytoplasmic sperm injection outcome in cancer survivors with no available cryopreserved sperm. J Assist Reprod Genet 37, 875–882 (2020). https://doi.org/10.1007/s10815-020-01697-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01697-7