Abstract
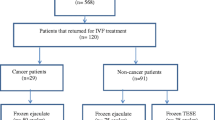
Infertile male cancer survivors may benefit from the use of sperm cryopreserved before starting antineoplastic treatments or by attempting testicular sperm retrieval, if they did not bank sperm, or by using donor sperm.
Intrauterine insemination (IUI) with cryopreserved sperm provides a clinical pregnancy rate of 13.1% per cycle with a live birth rate of 9.3%. IUI is simple and affordable but requires sperm of good quality. Intrauterine insemination with donor sperm (IUI-D) provides higher success rates, although there are no specific reports in cancer survivors. In unselected population, live birth rates per IUI-D range from 8.4% in the natural cycle to 21.3% using hormonal stimulation.
Conventional in vitro fertilization (IVF) is more complex and expensive but can be used with sub-optimal sperm and provides higher success rates than IUI (clinical pregnancy rate of 27.8% per cycle with a live birth rate of 24.6%). Intracytoplasmic sperm injection (ICSI) is the most efficient option when sperm parameters (number, motility, and morphology) are very poor. ICSI clinical pregnancy rate and live birth rate per cycle are 38.2% and 32.9%, respectively. The ICSI combined with surgically retrieved testicular sperm (TESE or micro-TESE) is the most expensive option with clinical pregnancy rate per cycle of 32.3% and the live birth rate of 23.9%.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Meistrich ML. Effects of chemotherapy and radiotherapy on spermatogenesis in humans. Fertil Steril. 2013;100(5):1180–6. https://doi.org/10.1016/j.fertnstert.2013.08.010.
Tournaye H, Dohle GR, Barratt CL. Fertility preservation in men with cancer. Lancet. 2014;384(9950):1295–301. https://doi.org/10.1016/S0140-6736(14)60495-5.
Gunnes MW, Lie RT, Bjorge T, Ghaderi S, Ruud E, Syse A, et al. Reproduction and marriage among male survivors of cancer in childhood, adolescence and young adulthood: a national cohort study. Br J Cancer. 2016;114(3):348–56. https://doi.org/10.1038/bjc.2015.455.
Stensheim H, Cvancarova M, Moller B, Fossa SD. Pregnancy after adolescent and adult cancer: a population-based matched cohort study. Int J Cancer. 2011;129(5):1225–36. https://doi.org/10.1002/ijc.26045.
Botchan A, Karpol S, Lehavi O, Paz G, Kleiman SE, Yogev L, et al. Preservation of sperm of cancer patients: extent of use and pregnancy outcome in a tertiary infertility center. Asian J Androl. 2013;15(3):382–6. https://doi.org/10.1038/aja.2013.3.
Chan PT, Palermo GD, Veeck LL, Rosenwaks Z, Schlegel PN. Testicular sperm extraction combined with intracytoplasmic sperm injection in the treatment of men with persistent azoospermia postchemotherapy. Cancer. 2001;92(6):1632–7. https://doi.org/10.1002/1097-0142(20010915)92:6<1632::aid-cncr1489>3.0.co;2-i.
Levi-Setti PE, Negri L, Baggiani A, Morenghi E, Albani E, Dioguardi CMC, et al. Testicular sperm extraction and intracytoplasmic sperm injection outcome in cancer survivors with no available cryopreserved sperm. J Assist Reprod Genet. 2020;37(4):875–82. https://doi.org/10.1007/s10815-020-01697-7.
Ferrari S, Paffoni A, Filippi F, Busnelli A, Vegetti W, Somigliana E. Sperm cryopreservation and reproductive outcome in male cancer patients: a systematic review. Reprod Biomed Online. 2016;33(1):29–38. https://doi.org/10.1016/j.rbmo.2016.04.002.
Rauck AM, Green DM, Yasui Y, Mertens A, Robison LL. Marriage in the survivors of childhood cancer: a preliminary description from the childhood Cancer survivor study. Med Pediatr Oncol. 1999;33(1):60–3. https://doi.org/10.1002/(sici)1096-911x(199907)33:1<60::aid-mpo11>3.0.co;2-h.
Pivetta E, Maule MM, Pisani P, Zugna D, Haupt R, Jankovic M, et al. Marriage and parenthood among childhood cancer survivors: a report from the Italian AIEOP off-therapy registry. Haematologica. 2011;96(5):744–51. https://doi.org/10.3324/haematol.2010.036129.
Frobisher C, Lancashire ER, Winter DL, Jenkinson HC, Hawkins MM. British childhood Cancer survivor S. long-term population-based marriage rates among adult survivors of childhood cancer in Britain. Int J Cancer. 2007;121(4):846–55. https://doi.org/10.1002/ijc.22742.
Fitoussi E. H, Tchen N, Berjon JP, Soubeyran P, Hoerni B. Semen analysis and cryoconservation before treatment in Hodgkin's disease. Ann Oncol. 2000;11(6):679–84. https://doi.org/10.1023/a:1008353728560.
Brydoy M, Fossa SD, Klepp O, Bremnes RM, Wist EA, Wentzel-Larsen T, et al. Paternity following treatment for testicular cancer. J Natl Cancer Inst. 2005;97(21):1580–8. https://doi.org/10.1093/jnci/dji339.
Sieniawski M, Reineke T, Josting A, Nogova L, Behringer K, Halbsguth T, et al. Assessment of male fertility in patients with Hodgkin's lymphoma treated in the German Hodgkin study group (GHSG) clinical trials. Ann Oncol. 2008;19(10):1795–801. https://doi.org/10.1093/annonc/mdn376.
Paoli D, Rizzo F, Fiore G, Pallotti F, Pulsoni A, Annechini G, et al. Spermatogenesis in Hodgkin's lymphoma patients: a retrospective study of semen quality before and after different chemotherapy regimens. Hum Reprod. 2016;31(2):263–72. https://doi.org/10.1093/humrep/dev310.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Published on behalf of the World Health Organization by Cambridge University Press; 1999.
World Health Organization DoRHaR. WHO laboratory manual for the examination and processing of human semen. 5th edition: Geneva : World Health Organization 2010.
Hamilton JA, Cissen M, Brandes M, Smeenk JM, de Bruin JP, Kremer JA, et al. Total motile sperm count: a better indicator for the severity of male factor infertility than the WHO sperm classification system. Hum Reprod. 2015;30(5):1110–21. https://doi.org/10.1093/humrep/dev058.
Borges E Jr, Setti AS, Braga DP, Figueira RC, Iaconelli A Jr. Total motile sperm count has a superior predictive value over the WHO 2010 cut-off values for the outcomes of intracytoplasmic sperm injection cycles. Andrology. 2016;4(5):880–6. https://doi.org/10.1111/andr.12199.
Degl'Innocenti S, Filimberti E, Magini A, Krausz C, Lombardi G, Fino MG, et al. Semen cryopreservation for men banking for oligospermia, cancers, and other pathologies: prediction of post-thaw outcome using basal semen quality. Fertil Steril. 2013;100(6):1555–63 e1-3. https://doi.org/10.1016/j.fertnstert.2013.08.005.
Hotaling JM, Lopushnyan NA, Davenport M, Christensen H, Pagel ER, Muller CH, et al. Raw and test-thaw semen parameters after cryopreservation among men with newly diagnosed cancer. Fertil Steril. 2013;99(2):464–9. https://doi.org/10.1016/j.fertnstert.2012.09.031.
Johnson MD, Cooper AR, Jungheim ES, Lanzendorf SE, Odem RR, Ratts VS. Sperm banking for fertility preservation: a 20-year experience. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):177–82. https://doi.org/10.1016/j.ejogrb.2013.06.021.
Hallak J, Kolettis PN, Sekhon VS, Thomas AJ Jr, Agarwal A. Sperm cryopreservation in patients with testicular cancer. Urology. 1999;54(5):894–9. https://doi.org/10.1016/s0090-4295(99)00267-8.
Bizet P, Saias-Magnan J, Jouve E, Grillo JM, Karsenty G, Metzler-Guillemain C, et al. Sperm cryopreservation before cancer treatment: a 15-year monocentric experience. Reprod Biomed Online. 2012;24(3):321–30. https://doi.org/10.1016/j.rbmo.2011.11.015.
Agarwal A. Semen banking in patients with cancer: 20-year experience. Int J Androl. 2000;23(Suppl 2):16–9. https://doi.org/10.1046/j.1365-2605.2000.00005.x.
Chung K, Irani J, Knee G, Efymow B, Blasco L, Patrizio P. Sperm cryopreservation for male patients with cancer: an epidemiological analysis at the University of Pennsylvania. Eur J Obstet Gynecol Reprod Biol. 2004;113(Suppl 1):S7–11. https://doi.org/10.1016/j.ejogrb.2003.11.024.
Kerin JF, Kirby C, Peek J, Jeffrey R, Warnes GM, Matthews CD, et al. Improved conception rate after intrauterine insemination of washed spermatozoa from men with poor quality semen. Lancet. 1984;1(8376):533–5. https://doi.org/10.1016/s0140-6736(84)90932-2.
Berger T, Marrs RP, Moyer DL. Comparison of techniques for selection of motile spermatozoa. Fertil Steril. 1985;43(2):268–73.
Stahl PJ, Stember DS, Mulhall JP. Options for fertility preservation in men and boys with cancer. Adv Exp Med Biol. 2012;732:29–39. https://doi.org/10.1007/978-94-007-2492-1_3.
Wang JH, Muller CH, Lin K. Optimizing fertility preservation for pre- and postpubertal males with cancer. Semin Reprod Med. 2013;31(4):274–85. https://doi.org/10.1055/s-0033-1345275.
Anger JT, Gilbert BR, Goldstein M. Cryopreservation of sperm: indications, methods and results. J Urol. 2003;170(4 Pt 1):1079–84. https://doi.org/10.1097/01.ju.0000084820.98430.b8.
Williams DH. Sperm banking and the cancer patient. Ther Adv Urol. 2010;2(1):19–34. https://doi.org/10.1177/1756287210368279.
Isachenko E, Isachenko V, Katkov II, Rahimi G, Schondorf T, Mallmann P, et al. DNA integrity and motility of human spermatozoa after standard slow freezing versus cryoprotectant-free vitrification. Hum Reprod. 2004;19(4):932–9. https://doi.org/10.1093/humrep/deh194.
Bagchi A, Woods EJ, Critser JK. Cryopreservation and vitrification: recent advances in fertility preservation technologies. Expert Rev Med Devices. 2008;5(3):359–70. https://doi.org/10.1586/17434440.5.3.359.
Barratt CL, Clements S, Kessopoulou E. Semen characteristics and fertility tests required for storage of spermatozoa. Hum Reprod. 1998;13(Suppl 2):1–7.; discussion 8-11. https://doi.org/10.1093/humrep/13.suppl_2.1.
Van Voorhis BJ, Barnett M, Sparks AE, Syrop CH, Rosenthal G, Dawson J. Effect of the total motile sperm count on the efficacy and cost-effectiveness of intrauterine insemination and in vitro fertilization. Fertil Steril. 2001;75(4):661–8. https://doi.org/10.1016/s0015-0282(00)01783-0.
Khalil MR, Rasmussen PE, Erb K, Laursen SB, Rex S, Westergaard LG. Homologous intrauterine insemination. An evaluation of prognostic factors based on a review of 2473 cycles. Acta Obstet Gynecol Scand. 2001;80(1):74–81. https://doi.org/10.1034/j.1600-0412.2001.800115.x.
Miller DC, Hollenbeck BK, Smith GD, Randolph JF, Christman GM, Smith YR, et al. Processed total motile sperm count correlates with pregnancy outcome after intrauterine insemination. Urology. 2002;60(3):497–501. https://doi.org/10.1016/s0090-4295(02)01773-9.
Freour T, Mirallie S, Jean M, Barriere P. Sperm banking and assisted reproductive outcome in men with cancer: a 10 years’ experience. Int J Clin Oncol. 2012;17(6):598–603. https://doi.org/10.1007/s10147-011-0330-3.
Nangia AK, Krieg SA, Kim SS. Clinical guidelines for sperm cryopreservation in cancer patients. Fertil Steril. 2013;100(5):1203–9. https://doi.org/10.1016/j.fertnstert.2013.08.054.
Practice Committee of American Society for Reproductive M. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2013;100(5):1214–23. https://doi.org/10.1016/j.fertnstert.2013.08.012.
Agarwal A, Sidhu RK, Shekarriz M, Thomas AJ Jr. Optimum abstinence time for cryopreservation of semen in cancer patients. J Urol. 1995;154(1):86–8.
Aboulghar M, Mansour R, Serour G, Abdrazek A, Amin Y, Rhodes C. Controlled ovarian hyperstimulation and intrauterine insemination for treatment of unexplained infertility should be limited to a maximum of three trials. Fertil Steril. 2001;75(1):88–91. https://doi.org/10.1016/s0015-0282(00)01641-1.
Morshedi M, Duran HE, Taylor S, Oehninger S. Efficacy and pregnancy outcome of two methods of semen preparation for intrauterine insemination: a prospective randomized study. Fertil Steril. 2003;79(Suppl 3):1625–32. https://doi.org/10.1016/s0015-0282(03)00250-4.
Tournaye H. Male factor infertility and ART. Asian J Androl. 2012;14(1):103–8. https://doi.org/10.1038/aja.2011.65.
Goverde AJ, McDonnell J, Vermeiden JP, Schats R, Rutten FF, Schoemaker J. Intrauterine insemination or in-vitro fertilisation in idiopathic subfertility and male subfertility: a randomised trial and cost-effectiveness analysis. Lancet. 2000;355(9197):13–8. https://doi.org/10.1016/S0140-6736(99)04002-7.
Practice Committee of the American Society for Reproductive M. Aging and infertility in women. Fertil Steril. 2006;86(5 Suppl 1):S248–52. https://doi.org/10.1016/j.fertnstert.2006.08.024.
Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H. Predictive factors for pregnancy after intrauterine insemination (IUI): an analysis of 1038 cycles and a review of the literature. Fertil Steril. 2010;93(1):79–88. https://doi.org/10.1016/j.fertnstert.2008.09.058.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of 'poor response' to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24. https://doi.org/10.1093/humrep/der092.
Audrins P, Holden CA, McLachlan RI, Kovacs GT. Semen storage for special purposes at Monash IVF from 1977 to 1997. Fertil Steril. 1999;72(1):179–81. https://doi.org/10.1016/s0015-0282(99)00163-6.
Kelleher S, Wishart SM, Liu PY, Turner L, Di Pierro I, Conway AJ, et al. Long-term outcomes of elective human sperm cryostorage. Hum Reprod. 2001;16(12):2632–9. https://doi.org/10.1093/humrep/16.12.2632.
Lass A, Akagbosu F, Brinsden P. Sperm banking and assisted reproduction treatment for couples following cancer treatment of the male partner. Hum Reprod Update. 2001;7(4):370–7. https://doi.org/10.1093/humupd/7.4.370.
Ragni G, Somigliana E, Restelli L, Salvi R, Arnoldi M, Paffoni A. Sperm banking and rate of assisted reproduction treatment: insights from a 15-year cryopreservation program for male cancer patients. Cancer. 2003;97(7):1624–9. https://doi.org/10.1002/cncr.11229.
Agarwal A, Ranganathan P, Kattal N, Pasqualotto F, Hallak J, Khayal S, et al. Fertility after cancer: a prospective review of assisted reproductive outcome with banked semen specimens. Fertil Steril. 2004;81(2):342–8. https://doi.org/10.1016/j.fertnstert.2003.07.021.
Schmidt KL, Larsen E, Bangsboll S, Meinertz H, Carlsen E, Andersen AN. Assisted reproduction in male cancer survivors: fertility treatment and outcome in 67 couples. Hum Reprod. 2004;19(12):2806–10. https://doi.org/10.1093/humrep/deh518.
Meseguer M, Molina N, Garcia-Velasco JA, Remohi J, Pellicer A, Garrido N. Sperm cryopreservation in oncological patients: a 14-year follow-up study. Fertil Steril. 2006;85(3):640–5. https://doi.org/10.1016/j.fertnstert.2005.08.022.
van Casteren NJ, van Santbrink EJ, van Inzen W, Romijn JC, Dohle GR. Use rate and assisted reproduction technologies outcome of cryopreserved semen from 629 cancer patients. Fertil Steril. 2008;90(6):2245–50. https://doi.org/10.1016/j.fertnstert.2007.10.055.
Crha I, Ventruba P, Zakova J, Huser M, Kubesova B, Hudecek R, et al. Survival and infertility treatment in male cancer patients after sperm banking. Fertil Steril. 2009;91(6):2344–8. https://doi.org/10.1016/j.fertnstert.2008.03.053.
Zakova J, Lousova E, Ventruba P, Crha I, Pochopova H, Vinklarkova J, et al. Sperm cryopreservation before testicular cancer treatment and its subsequent utilization for the treatment of infertility. ScientificWorldJournal. 2014;2014:575978. https://doi.org/10.1155/2014/575978.
Muller I, Oude Ophuis RJ, Broekmans FJ, Lock TM. Semen cryopreservation and usage rate for assisted reproductive technology in 898 men with cancer. Reprod Biomed Online. 2016;32(2):147–53. https://doi.org/10.1016/j.rbmo.2015.11.005.
Khalifa E, Oehninger S, Acosta AA, Morshedi M, Veeck L, Bryzyski RG, et al. Successful fertilization and pregnancy outcome in in-vitro fertilization using cryopreserved/thawed spermatozoa from patients with malignant diseases. Hum Reprod. 1992;7(1):105–8. https://doi.org/10.1093/oxfordjournals.humrep.a137539.
Hourvitz A, Goldschlag DE, Davis OK, Gosden LV, Palermo GD, Rosenwaks Z. Intracytoplasmic sperm injection (ICSI) using cryopreserved sperm from men with malignant neoplasm yields high pregnancy rates. Fertil Steril. 2008;90(3):557–63. https://doi.org/10.1016/j.fertnstert.2007.03.002.
Depalo R, Falagario D, Masciandaro P, Nardelli C, Vacca MP, Capuano P, et al. Fertility preservation in males with cancer: 16-year monocentric experience of sperm banking and post-thaw reproductive outcomes. Ther Adv Med Oncol. 2016;8(6):412–20. https://doi.org/10.1177/1758834016665078.
Garcia A, Herrero MB, Holzer H, Tulandi T, Chan P. Assisted reproductive outcomes of male cancer survivors. J Cancer Surviv. 2015;9(2):208–14. https://doi.org/10.1007/s11764-014-0398-7.
Levi-Setti PE, Negri L, Baggiani A, Morenghi E, Albani E, Parini V, et al. Delayed childbearing and female ageing impair assisted reproductive technology outcome in survivors of male haematological cancers. J Assist Reprod Genet. 2018;35(11):2049–56. https://doi.org/10.1007/s10815-018-1283-5.
Ethics Committee of the American Society for Reproductive M. Disparities in access to effective treatment for infertility in the United States: an ethics committee opinion. Fertil Steril. 2015;104(5):1104–10. https://doi.org/10.1016/j.fertnstert.2015.07.1139.
Girasole CR, Cookson MS, Smith JA Jr, Ivey BS, Roth BJ, Chang SS. Sperm banking: use and outcomes in patients treated for testicular cancer. BJU Int. 2007;99(1):33–6. https://doi.org/10.1111/j.1464-410X.2006.06537.x.
Gilbert K, Nangia AK, Dupree JM, Smith JF, Mehta A. Fertility preservation for men with testicular cancer: is sperm cryopreservation cost effective in the era of assisted reproductive technology? Urol Oncol. 2018;36(3):92 e1–9. https://doi.org/10.1016/j.urolonc.2017.11.002.
Wu AK, Odisho AY, Washington SL 3rd, Katz PP, Smith JF. Out-of-pocket fertility patient expense: data from a multicenter prospective infertility cohort. J Urol. 2014;191(2):427–32. https://doi.org/10.1016/j.juro.2013.08.083.
Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91(6):2281–94. https://doi.org/10.1016/j.fertnstert.2009.04.029.
Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Wing H, et al. Costs of infertility treatment: results from an 18-month prospective cohort study. Fertil Steril. 2011;95(3):915–21. https://doi.org/10.1016/j.fertnstert.2010.11.026.
Ombelet W, Cooke I, Dyer S, Serour G, Devroey P. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14(6):605–21. https://doi.org/10.1093/humupd/dmn042.
Zuzuarregui JL, Meseguer M, Garrido N, Simon C, Pellicer A, Remohi J. Parameters affecting the results in a program of artificial insemination with donor sperm. A 12-year retrospective review of more than 1800 cycles. J Assist Reprod Genet. 2004;21(4):109–18. https://doi.org/10.1023/b:jarg.0000029494.55273.a2.
van Rumste MM, Custers IM, van der Veen F, van Wely M, Evers JL, Mol BW. The influence of the number of follicles on pregnancy rates in intrauterine insemination with ovarian stimulation: a meta-analysis. Hum Reprod Update. 2008;14(6):563–70. https://doi.org/10.1093/humupd/dmn034.
Cohlen B, Bijkerk A, Van der Poel S, Ombelet W. IUI: review and systematic assessment of the evidence that supports global recommendations. Hum Reprod Update. 2018;24(3):300–19. https://doi.org/10.1093/humupd/dmx041.
Kop PA, van Wely M, Mol BW, de Melker AA, Janssens PM, Arends B, et al. Intrauterine insemination or intracervical insemination with cryopreserved donor sperm in the natural cycle: a cohort study. Hum Reprod. 2015;30(3):603–7. https://doi.org/10.1093/humrep/dev004.
Patton PE, Burry KA, Thurmond A, Novy MJ, Wolf DP. Intrauterine insemination outperforms intracervical insemination in a randomized, controlled study with frozen, donor semen. Fertil Steril. 1992;57(3):559–64. https://doi.org/10.1016/s0015-0282(16)54900-0.
Carroll N, Palmer JR. A comparison of intrauterine versus intracervical insemination in fertile single women. Fertil Steril. 2001;75(4):656–60. https://doi.org/10.1016/s0015-0282(00)01782-9.
Gorrill MJ, Burry KA, Patton PE. Pregnancy outcomes using donor sperm insemination after failed in vitro fertilization with intracytoplasmic sperm injection cycles in couples with complex infertility disorders. Fertil Steril. 2003;80(4):936–8. https://doi.org/10.1016/s0015-0282(03)01120-8.
Zhang A, Ma X, Zhang L, Zhang X, Wang W. Pregnancy and offspring outcomes after artificial insemination with donor sperm: a retrospective analysis of 1805 treatment cycles performed in Northwest China. Medicine (Baltimore). 2019;98(16):e14975. https://doi.org/10.1097/MD.0000000000014975.
Han JS, Brannigan RE. Donor insemination and infertility: what general urologists need to know. Nat Clin Pract Urol. 2008;5(3):151–8. https://doi.org/10.1038/ncpuro1018.
Le Lannou D. Is the limitation to 6 cycles of insemination with donor sperm justified? Gynecol Obstet Fertil. 2002;30(2):129–32. https://doi.org/10.1016/s1297-9589(01)00279-x.
Egan J. Wanted: a few good sperm (looking for Mr. Good Sperm). N Y Times Mag. 2006:44–51, 66, 81, 98, 100.
Payne D, Flaherty SP, Jeffrey R, Warnes GM, Matthews CD. Successful treatment of severe male factor infertility in 100 consecutive cycles using intracytoplasmic sperm injection. Hum Reprod. 1994;9(11):2051–7. https://doi.org/10.1093/oxfordjournals.humrep.a138392.
Verheyen G, Tournaye H, Staessen C, De Vos A, Vandervorst M, Van Steirteghem A. Controlled comparison of conventional in-vitro fertilization and intracytoplasmic sperm injection in patients with asthenozoospermia. Hum Reprod. 1999;14(9):2313–9. https://doi.org/10.1093/humrep/14.9.2313.
Fisch B, Kaplan-Kraicer R, Amit S, Zukerman Z, Ovadia J, Tadir Y. The relationship between sperm parameters and fertilizing capacity in vitro: a predictive role for swim-up migration. J In Vitro Fert Embryo Transf. 1990;7(1):38–44. https://doi.org/10.1007/BF01133882.
Grow DR, Oehninger S, Seltman HJ, Toner JP, Swanson RJ, Kruger TF, et al. Sperm morphology as diagnosed by strict criteria: probing the impact of teratozoospermia on fertilization rate and pregnancy outcome in a large in vitro fertilization population. Fertil Steril. 1994;62(3):559–67. https://doi.org/10.1016/s0015-0282(16)56946-5.
van Weert JM, Repping S, Van Voorhis BJ, van der Veen F, Bossuyt PM, Mol BW. Performance of the postwash total motile sperm count as a predictor of pregnancy at the time of intrauterine insemination: a meta-analysis. Fertil Steril. 2004;82(3):612–20. https://doi.org/10.1016/j.fertnstert.2004.01.042.
Van Voorhis BJ, Sparks AE, Allen BD, Stovall DW, Syrop CH, Chapler FK. Cost-effectiveness of infertility treatments: a cohort study. Fertil Steril. 1997;67(5):830–6. https://doi.org/10.1016/s0015-0282(97)81393-3.
Nagy ZP, Liu J, Joris H, Verheyen G, Tournaye H, Camus M, et al. The result of intracytoplasmic sperm injection is not related to any of the three basic sperm parameters. Hum Reprod. 1995;10(5):1123–9. https://doi.org/10.1093/oxfordjournals.humrep.a136104.
Tournaye H, Goossens E, Verheyen G, Frederickx V, De Block G, Devroey P, et al. Preserving the reproductive potential of men and boys with cancer: current concepts and future prospects. Hum Reprod Update. 2004;10(6):525–32. https://doi.org/10.1093/humupd/dmh038.
Dohle GR. Male infertility in cancer patients: review of the literature. Int J Urol. 2010;17(4):327–31. https://doi.org/10.1111/j.1442-2042.2010.02484.x.
Revel A, Haimov-Kochman R, Porat A, Lewin A, Simon A, Laufer N, et al. In vitro fertilization-intracytoplasmic sperm injection success rates with cryopreserved sperm from patients with malignant disease. Fertil Steril. 2005;84(1):118–22. https://doi.org/10.1016/j.fertnstert.2005.01.121.
Zorn B, Virant-Klun I, Stanovnik M, Drobnic S, Meden-Vrtovec H. Intracytoplasmic sperm injection by testicular sperm in patients with aspermia or azoospermia after cancer treatment. Int J Androl. 2006;29(5):521–7. https://doi.org/10.1111/j.1365-2605.2006.00684.x.
Ishikawa H, Kaneko S, Miyaji K, Takamatsu K. Cryopreservation of human sperm in patients with malignancy: first 2 years' experience. Reprod Med Biol. 2007;6(2):127–31. https://doi.org/10.1111/j.1447-0578.2007.00175.x.
Gil-Villa AM, Cardona-Maya W, Agarwal A, Sharma R, Cadavid A. Role of male factor in early recurrent embryo loss: do antioxidants have any effect? Fertil Steril. 2009;92(2):565–71. https://doi.org/10.1016/j.fertnstert.2008.07.1715.
Brandes M, Verzijden JC, Hamilton CJ, de Weys NP, de Bruin JP, Bots RS, et al. Is the fertility treatment itself a risk factor for early pregnancy loss? Reprod Biomed Online. 2011;22(2):192–9. https://doi.org/10.1016/j.rbmo.2010.10.013.
Silber SJ, van Steirteghem A, Nagy Z, Liu J, Tournaye H, Devroey P. Normal pregnancies resulting from testicular sperm extraction and intracytoplasmic sperm injection for azoospermia due to maturation arrest. Fertil Steril. 1996;66(1):110–7. https://doi.org/10.1016/s0015-0282(16)58396-4.
Schlegel PN. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod. 1999;14(1):131–5. https://doi.org/10.1093/humrep/14.1.131.
Corona G, Minhas S, Giwercman A, Bettocchi C, Dinkelman-Smit M, Dohle G, et al. Sperm recovery and ICSI outcomes in men with non-obstructive azoospermia: a systematic review and meta-analysis. Hum Reprod Update. 2019;25(6):733–57. https://doi.org/10.1093/humupd/dmz028.
Hsiao W, Stahl PJ, Osterberg EC, Nejat E, Palermo GD, Rosenwaks Z, et al. Successful treatment of postchemotherapy azoospermia with microsurgical testicular sperm extraction: the Weill Cornell experience. J Clin Oncol. 2011;29(12):1607–11. https://doi.org/10.1200/JCO.2010.33.7808.
Damani MN, Master V, Meng MV, Burgess C, Turek P, Oates RD. Postchemotherapy ejaculatory azoospermia: fatherhood with sperm from testis tissue with intracytoplasmic sperm injection. J Clin Oncol. 2002;20(4):930–6. https://doi.org/10.1200/JCO.2002.20.4.930.
Meseguer M, Garrido N, Remohi J, Pellicer A, Simon C, Martinez-Jabaloyas JM, et al. Testicular sperm extraction (TESE) and ICSI in patients with permanent azoospermia after chemotherapy. Hum Reprod. 2003;18(6):1281–5. https://doi.org/10.1093/humrep/deg260.
Hibi H, Ohori T, Yamada Y, Honda N, Hashiba Y, Asada Y. Testicular sperm extraction and ICSI in patients with post-chemotherapy non-obstructive azoospermia. Arch Androl. 2007;53(2):63–5. https://doi.org/10.1080/01485010600915152.
Shiraishi K, Matsuyama H. Microdissection testicular sperm extraction and salvage hormonal treatment in patients with postchemotherapy azoospermia. Urology. 2014;83(1):100–6. https://doi.org/10.1016/j.urology.2013.08.043.
Shin T, Kobayashi T, Shimomura Y, Iwahata T, Suzuki K, Tanaka T, et al. Microdissection testicular sperm extraction in Japanese patients with persistent azoospermia after chemotherapy. Int J Clin Oncol. 2016;21(6):1167–71. https://doi.org/10.1007/s10147-016-0998-5.
Dar S, Orvieto R, Levron J, Haas J, Gat I, Raviv G. IVF outcome in azoospermic cancer survivors. Eur J Obstet Gynecol Reprod Biol. 2018;220:84–7. https://doi.org/10.1016/j.ejogrb.2017.11.015.
Stahl O, Eberhard J, Cavallin-Stahl E, Jepson K, Friberg B, Tingsmark C, et al. Sperm DNA integrity in cancer patients: the effect of disease and treatment. Int J Androl. 2009;32(6):695–703. https://doi.org/10.1111/j.1365-2605.2008.00933.x.
Landres IV, Milki AA, Lathi RB. Karyotype of miscarriages in relation to maternal weight. Hum Reprod. 2010;25(5):1123–6. https://doi.org/10.1093/humrep/deq025.
Wang JX, Davies MJ, Norman RJ. Polycystic ovarian syndrome and the risk of spontaneous abortion following assisted reproductive technology treatment. Hum Reprod. 2001;16(12):2606–9. https://doi.org/10.1093/humrep/16.12.2606.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Negri, L., Patrizio, P., Levi-Setti, P.E. (2022). ART in Male Cancer Patients Including Sperm Donation. In: Grynberg, M., Patrizio, P. (eds) Female and Male Fertility Preservation. Springer, Cham. https://doi.org/10.1007/978-3-030-47767-7_35
Download citation
DOI: https://doi.org/10.1007/978-3-030-47767-7_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-47766-0
Online ISBN: 978-3-030-47767-7
eBook Packages: MedicineMedicine (R0)